Original Article - (2019) Volume 20, Issue 2
Balakumaran Sathyamoorthy, Karthick Rajendran, Bennett Duraisamy, Prabhakaran Raju, Amudhan Anbalagan, Kannan Devy Gounder
Institute of Surgical Gastroenterology, Rajiv Gandhi Government General Hospital, Madras Medical College, Chennai, India
Received Date: November 28th, 2018; Accepted Date: February 10th, 2019
Background Even with duodenum-preserving pancreatic head resection such as with the Frey procedure, the rate of recurrence of pain and analgesic drug usage is greater with small duct chronic calcific pancreatitis. The use of intraoperative neurolytic celiac plexus block in chronic calcific pancreatitis is not yet clearly defined. Objective To assess the effectiveness of neurolytic celiac plexus block while performing Frey’s procedure in a single center setting with a randomized double blind placebo controlled trial. Methods 136 chronic calcific pancreatitis patients admitted to our hospital with intractable pain were included in the study. 68 patients were allocated to Frey’s procedure with neurolytic celiac plexus block (Group I) and the remaining 68 patients were allocated to Frey’s procedure with placebo (Group II). Mean follow up period was 2.2 ± 0.5(range 1.5-3.4) years. Pain relief was the primary end-point. Results The neurolytic celiac plexus block group reported significant (P<0.0001) pain relief (98.5%) when compared with the placebo group (83.1%). Neurolytic celiac plexus block group had less opioid requirement, and better weight gain. Physical and Mental Health Composite Scales in Quality of life assessment were better in group I (P<0.0001). Multivariate regression analysis showed small duct disease significantly affects outcome (p=0.006, OR, 0.049; 95% CI, 0.006-0.421). Sub group analysis indicated that ductal diameter of 4.6-5 mm significantly affected the outcome (p=0.036). Conclusion The novel combination of Frey’s procedure with neurolytic celiac plexus block represents an effective tool in the treatment of pain in patients particularly those with small duct disease and improve quality of life in all chronic calcific pancreatitis patients.
Celiac plexus; Nerve Block; Pancreatic Diseases; Pancreatitis, Calcific; Visual Analog scale
CCP chronic calcific pancreatitis; DPPHR duodenumpreserving pancreatic head resection; LPJ lateral pancreatic jejunostomy; NCPB neurolytic celiac plexus block; QOL quality of life
Background and Objectives
In chronic calcific pancreatitis (CCP), the most worrisome feature is debilitating chronic abdominal pain (90-100%) which increases analgesic requirement and leads to poor quality of life [1]. Around 40-50% of patients can be managed conservatively, but the remaining 50-60% eventually requires surgical therapy [2, 3].
Lateral pancreatico jejunostomy provides symptomatic relief in 50-70% of patients especially in those who have a wide duct (>7 mm), suggesting that this procedure addresses only the ductal hypertension theory [4, 5]. Randomized controlled trials comparing resectional and non resectional procedures have proved that Frey’s procedure is superior since it was introduced in 1987 [6]. Although it addresses both ductal hypertension and the pacemaker theory, it provides only 80 to 90% pain relief [7, 8]. Small duct disease, alcoholic pancreatitis, longer disease duration, multiple prior endoscopic interventions, centralized (non-visceral) pain state and pre-operative opioid usage are factors found to be associated with failure of surgical therapy [9, 10]. However, the reason for the 10- 20% of failure is probably due to unaddressed or partially addressed neurogenic mechanisms of pain.
Neuro ablation can be considered not only for malignancy but also for CCP without pancreatic duct dilation [11]. In identifying the neurogenic cause as the main culprit for failure of Frey’s procedure the efficacy of intra operative celiac plexus neurolysis was tested by conducting a randomized trial. Until the present, there are no prospective studies comparing this technique in combination with the Frey’s procedure in the treatment of CCP.
This study was started after getting approval from institutional ethical committee of Madras Medical College, Chennai, Tamil Nadu, India. This trial was registered at clinical trials.gov: NCT- 02735330.
Sample Size
This study was based on a retrospective study undertaken by Carlos Chan et al. [12]. Pain control was the primary endpoint. Based on the literature pain control was recorded as 85% for Frey’ procedure. To have 95% confidence interval and 10% clinically expected variability, 136 subjects would be required, 68 in each arm of the study.
Formula used for this trial is,
N = [Z / d]2 × P × Q
N = 67.79 (68)
N = size per group; p = the response rate of standard treatment group. Q = Complement of P. d = the real difference between two treatment effect.
Inclusion Criteria
Patients considered for inclusion were those CCP patients between 13 to 65 years of age, with a pain score greater than 7, preoperative opioid use, must have desisted from alcohol and smoking for at least 6 months and with good performance status (ECOG ≤1- Eastern Cooperative Oncology Group).
Exclusion Criteria
Patients with mild to moderate pain score, continuous substance abuse, poor performance status (ECOG>1) were excluded from the study.
Primary Outcome
Post-operative pain relief measured by Visual Analogue Scale (VAS) (Range, 0-10) was the primary end-point of this study.
Secondary Outcome
Izbicki pain score [8] improvement, decrease in opioid analgesic consumption, weight gain, improvement in exocrine and exocrine function, as well as improvement in QOL were the secondary indicators.
Method of Study
The study comprised a single center, randomized (simple), double- blind, placebo- controlled, parallel arm, superiority trial. Randomization was undertaken at the time of surgery by an office staff using a random number table created with computerized software by a statistician not involved in the study. Blinding and allocation concealment was performed by using pre numbered containers previously filled with either absolute alcohol or saline according to the randomization chart which was kept sealed by office staff until the end of the study. Both subjects and response assessor were blinded.
Morphological and ductal anatomy was defined by contrast enhanced computed tomography (CT) / magnetic resonance cholangio pancreatography (MRCP). Pancreatic head mass was defined if antero-posterior diameter of head was >35 mm on CT. Type-1 pain was defined as shorter episodes of pain separated by pain-free intervals of several months. Type-2 pain was defined as prolonged periods of persistent (daily) or clusters of recurrent severe pain exacerbations. The small duct disease was defined as those having duct diameter of less than or equal to 5mm at the neck [12, 13].
Intra operatively anesthetists were informed while performing the NCPB/Placebo. Peripancreatic inflammation was diagnosed as inflammation extending beyond pancreas involving retropritoneum and adjacent structures noted by CT scan and confirmed during surgery.
Analgesics were given in the early post-operative period in the form of epidural bupivacaine and tramadol and beyond post-operative period given according to WHO ladder (paracetamol, week opioids like tramadol and strong opioids like morphine).
The pain score was recorded every 3 months by the primary investigator Patients who had a VAS score of >3 and requiring increased opioid analgesics were considered as failures of the procedure. Patients are considered as opioid dependent when they required opioids even though having mild pain score (<3) after surgery. The patients with poor surgical outcome (failure) were referred to pain clinic
Izbicki et al. proposed a scoring system in CCP using 4 variables with scores ranging between 0-100 for each variable namely frequency of pain attacks, VAS sore, analgesic medication(morphine related analgesic potency, time of disease related inability to work [8]. Secondary outcome measures were noted at the end of every 6 months. The mean values at the last follow up were taken as end-points for assessment of secondary outcomes.
Standard questionnaire format of SF 12 Version-2 with 4 weeks recall protocol was used for QOL assessment.
Data Collection
The preoperative baseline details such as etiology, morphology, associated complications and VAS pain score, Izbicki pain score, weight loss, endocrine status, exocrine status (fecal elastase) were collected on admission.
Additional procedures, the presence of chronic peripancreatic inflammatory changes [1] as evidenced by difficult Kocharisation due to adherent capsule and intraoperative complications were recorded during surgery.
Follow up details including pain relief measured by VAS score and Izbicki pain score, analgesics requirement weight gain, improvement in steatorrhoea (improvement in fecal elastase>200 μg/g of stool when associated with subjective reduction in foul smelling oily diarrhea), improvement in diabetic status (insulin& oral hypoglycemic agents requirement, HgbA1c), new onset diabetes (fasting glucose, GTT) mortality and morbidity were noted.
Follow up data were collected every 3 months on an outpatient basis. QOL assessment was done with a face to face interview as outpatient basis every 6months. The last follow up scores were used for analysis.
Statistical Analysis
Statistical analysis was performed in SPSS version 20. Continuous variables were presented as mean, standard deviation and 95% confidence interval; categorical variables were presented as frequencies. The chi-square test and the Fisher exact test were used to analyze categorical variables. The unpaired Student t test was used to analyze continuous variables. Missing values are treated with last observed value carried forward method. P value <0.05 was considered statistically significant. Factors found significant on univariate logistic regression analysis were incorporated in to the multivariate logistic regression analysis for odds ratio with 95% confidence intervals to analyze the significant factors affecting the outcome of surgery.
Procedure
All patients underwent Frey’s procedure irrespective of the presence or abcence of pancreatic headmass [14]. Additional procedures were performed as indicated to address specific complications. Operative procedures were performed by a single team with 2 experienced surgeons having more than 20 years of experience in this field. NCPB was performed after the head coring but before pancreatico jejunostomy, to avoid undue tension over anastamosis.The fascia overlying the aorta and celiac axis was not disected to facilitate diffusion of the drug or placebo. NCPB was performed either with 20 ml absolute alcohol diluted to 40 ml(50%) in study group or with 20 ml of saline mixed with 20 ml of distilled water in placebo group using a 22 gauge spinal needle injected just below the crus of the diaphragm, 20 ml on either side of celiac axis in a four quadrant fashion.
Study Population
165 consecutive CCP patients admitted in our department since January 2013 were screened for eligibility (Figure 1). 29 patients were excluded (25 were not meeting the inclusion criteria and 4 patients not willing to participate). After exclusion 136 patients were included in our study. They were randomized in to 2 groups, one group was treated by Frey’s procedure with NCPB (Group-I) and the other by Frey’s procedure with saline as placebo (Group-II).
All patients in this study were taking opioid preoperatively either continuously or intermittently depending upon the type of pain. Pancreatic pain was the most common indication for surgery. Type 2 pain was more common in alcoholic CCP and in those with associated complications (Table 1).
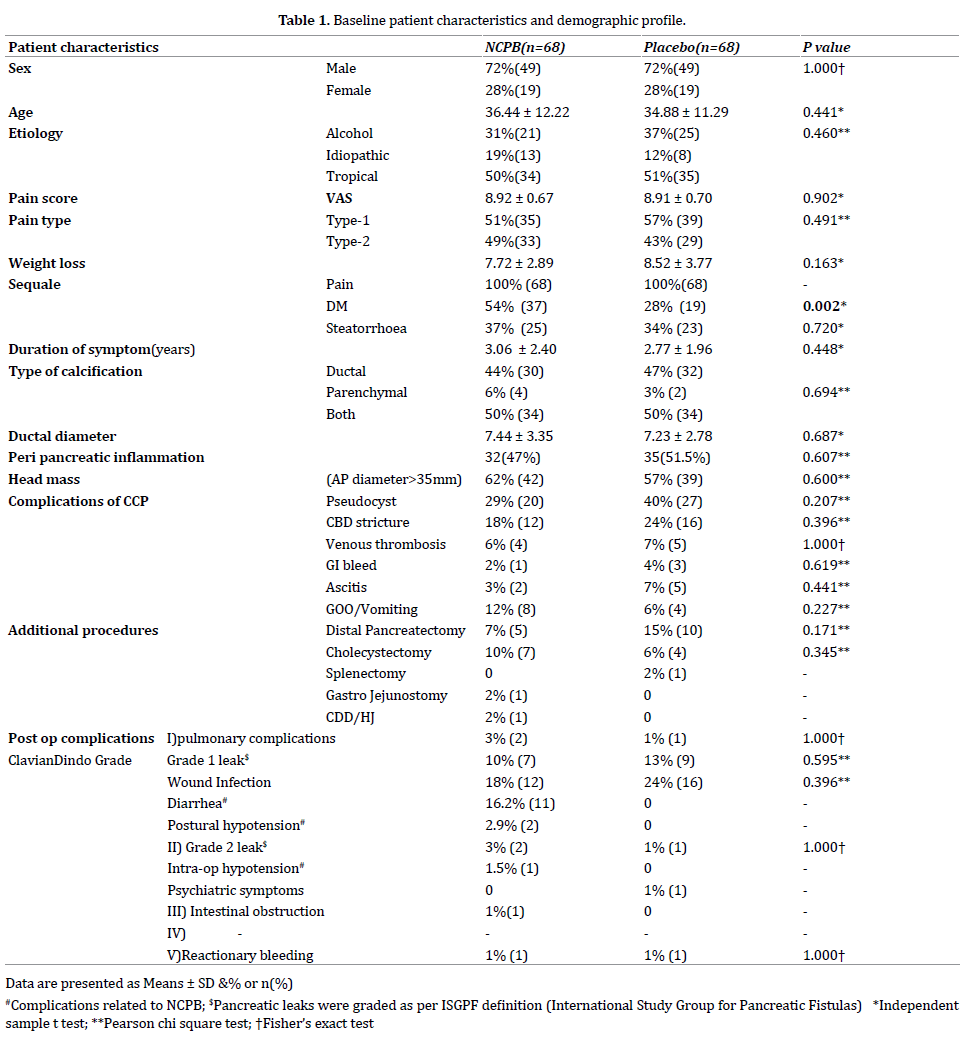
Combined ductal and parenchymal calcification pattern (50%) was more common rather than pure ductal (45.5%) and parenchymal (4.5%) calcification. Mean ductal diameter was 7.3 mm. 36% of patients had small duct disease 60% of the study populations had a pancreatic head mass. 50 % of patients had peripancreatic inflammation.
Pseudocyst was the most common complication followed by CBD stricture, venous thrombosis, GI bleeding, ascitis, and gastric outlet obstruction (GOO). Most of the CBD strictures were only radiological evidence of smooth narrowing of distal intra pancreatic bile duct without any biochemical changes like jaundice or elevated ALP (in which the decompression of the head itself will produce good relief) except in one case where persistent biochemical changes were present which necessitated surgical bypass. Notably the functional gastric outlet obstruction (gastro paresis) was more (8.8%) with those having small duct disease. Alcoholic CCP patients had more complications in this study.
In addition to Frey’s procedure, additional procedures were performed for complications of CCP. After randomization the baseline variables are equally distributed in both groups except for diabetes mellitus which were more in NCPB group (p=0.002).
Morbidity and Mortality
One patient had intra operative hypotension. Grade 1 pancreatic leaks (n=2) were managed conservatively. There were two grade 1 pancreatic leaks which resolved on conservative management. One Grade 2 leak resolved with percutaneous drainage under ultrasound guidance and octreotide infusion. Pulmonary complications and wound infections were more common in the placebo group. The most common complication associated with NCPB was diarrhea and postural hypotension usually after the 2nd postoperative day. All were successfully treated conservatively with crystalloids infusion (Table 1).
There were two postoperative deaths within 30 days (1.4%),one in each group. One patient (group I) sustained reactionary hemorrhage following Frey’s procedure combined with distal pancreatectomy and splenectomy. The second patient (group II) experienced splenic vein thrombosis without varices but did not undergo splenectomy, however developed massive gastrointestinal haemorrhage and shock 28 days after surgery.One patient (group I) died in a road traffic accident 6 months after the procedure.
There was a significant decrease (P<0.0001) in VAS mean pain score in group I (NCPB) up to3 years of postoperative assessment (Figure 2). Few patients had milder pain (VAS≤3) in the postoperative period either due to complications or wound pain due to surgical procedures in both groups. Even in this recurrence group, there was a significant pain free interval of 4 months in group I. There were twelve patients considered as treatment failures but only one in group 1 (Figure 3a).
Out of twelve treatment failure patients seven underwent successful CT guided celiac plexus neurolysis and 4 had failed neurolysis (Figure 3b). One patient in group 2 underwent revisional surgery and intraoperative NCPB. This patient was having centralized pain state and was experiencing recurrence of pain every 2 months. He underwent CT guided NCPB on three occasions and continued to have a requirement for morphine.
Figure 3: Recurrence and Reinterventions. (a). Recurrence in both groups with etiological subtypes. Failure rates are depicted as percentage. (b). Reinterventions performed for the poor outcome patients. Failed attempts for 4 patients indicate difficulty in placing the needle due to altered anatomy in the postoperative period.
There was a significant reduction of all variables in Izbicki score, when compared to preoperative value in both groups, except for analgesic intake which was significantly altered only in the NCPB group (85% vs. 13%, P<0.0001) (Table 2). The overall improvement in Izbicki score was 86% in the NCPB group compared to 58% in placebo group [P<0.0001] (Figure 4).
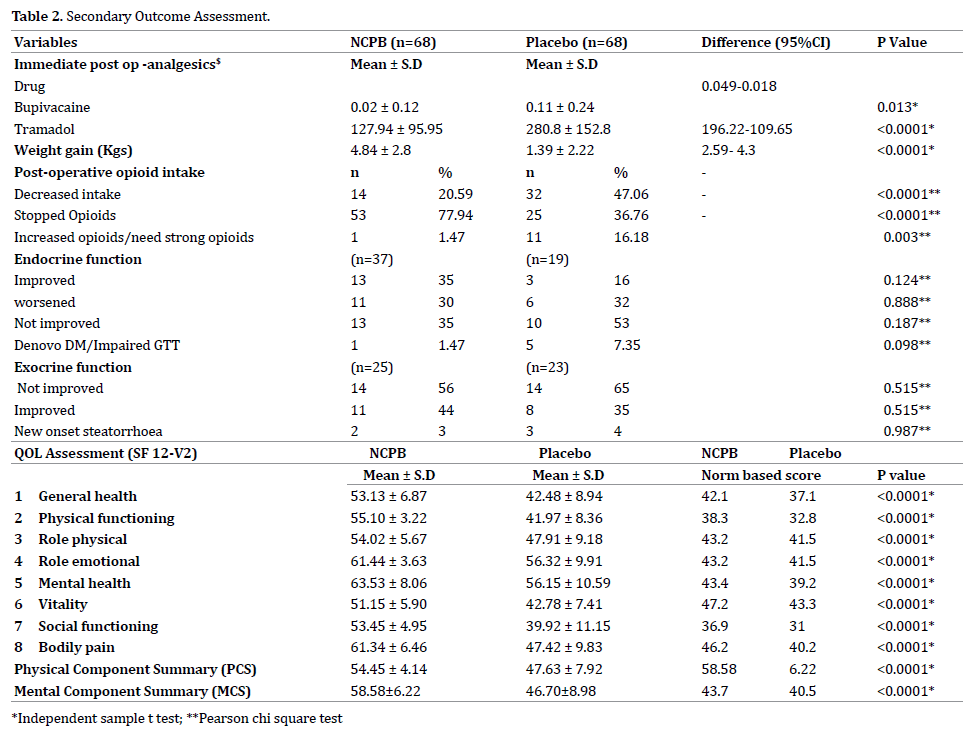
There was a significant reduction in dose and number of patients requiring post-operative epidural analgesics injection. 77.9% of patients in group I had completely stopped opioids compared to only 36.8% in group II (p=<0.0001). In group II 44.6% of patients had opioid dependency when compared to 15.6% in group I. One patient in group I (1.47 %) and 11 patients in group II (16.18%) required increased dose of opioids or required stronger opioids which represented a failure of the procedure. Mean weight gain significantly high in group I. In both groups there was an improvement in exocrine function but this was not statistically significant (P=0.833). There was a non-significant decrease (35%) in insulin/ OHA intake in group I. Interestingly; all six new onset DM patients underwent distal resection (40%).
Quality of Life (QOL)
The QOL at 6 months of follow up showed a significant improvement in group I patients (p<0.05). Both Physical and Mental Health Composite Scales were better in group I (Table 2).
The final success rate of the procedure was 98.5 % in group I and 83.8% in group II (P=0.003). Even though univariate analysis showed six parameters were having an association with outcome, (Table 3) multivariate analysis showed significance only for those having small duct disease (p=0.006, OR 0.049; 95% CI, 0.006-0.421) as shown in previous studies [15].
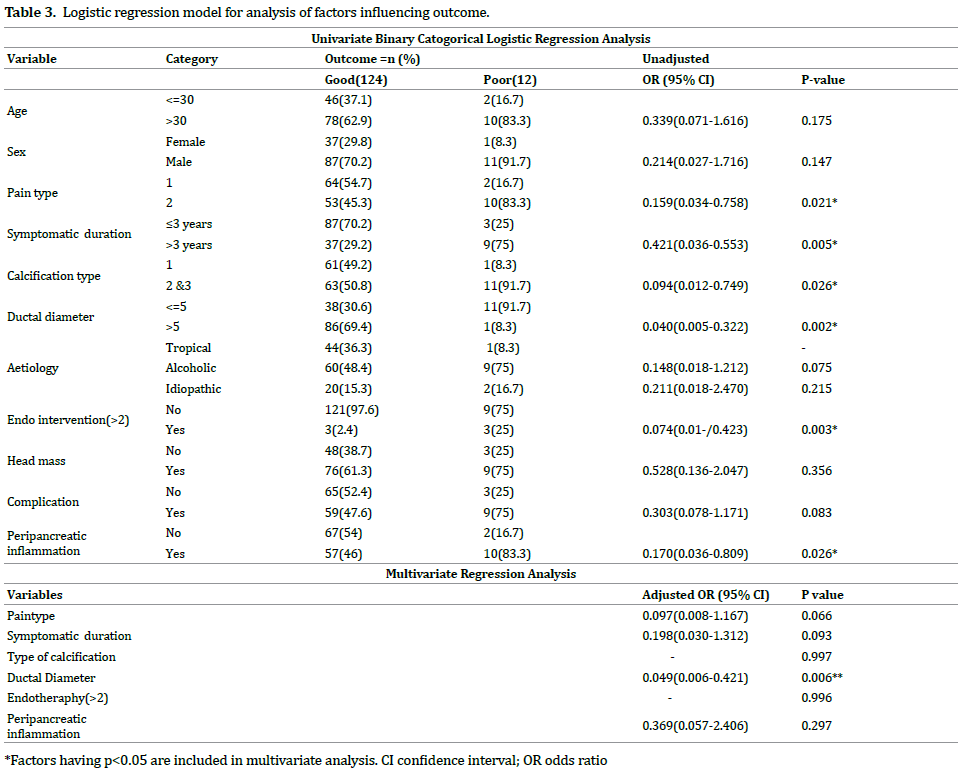
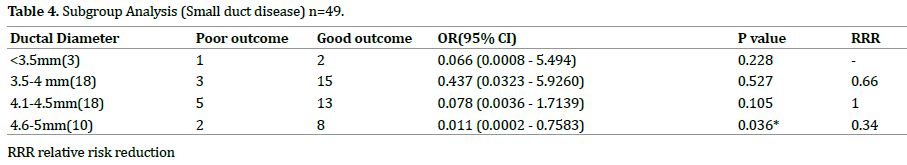
Non stratified Post–hoc analysis of the sub group of patients having small ductal diameter (n=49) was done to know which group of patients are good responders to treatment (Table 4, Figure 5). In patients with ductal diameter of 4.6-5 mm the pain relief was significant (p=0.036). The relative risk reduction (RRR) was high for 4.1-4.5 mm diameter and least when the diameter was between 4.6-5mm (0.34).
Concept of Multimodal Surgical Approach
There are three well known proposed theories for pain in chronic pancreatitis namely ductal and parenchymal hypertension, pacemaker and neurogenic theories [1, 16]. Other mechanisms are pancreatic ischemia, acute exacerbations of CP, and complications from the pancreas. The various mechanisms of pain namely nociceptive pain, neuropathic, neurogenic inflammation, neuro immune interactions are described in various articles [16, 17, 18, 19, 20]. All these mechanisms of pain when suspected must be addressed to achieve a better result. Requirement of multidisciplinary approach in the treatment of pain in chronic pancreatitis is stressed by many authors (SDC.1) [21].
Large duct disease with >7 cm diameter responds well to drainage procedures. Managing the chronic pancreatitis with small duct disease is always a daunting task. The predominant factor in pathogenesis of pain is neurological [12]. Small ductal diameter is the independent predictor of poor outcome following Frey’s procedure [15]. Few studies have claimed that modified ventral pancreas excision described by Izbicki [8, 12] and drainage procedures with head coring show promising long term results but at the cost of parenchymal loss [22]. Thoracoscopic splanchnicectomy was extensively studied in the treatment of small duct disease with good results [23].
Randomized controlled trials comparing surgery with endotherapy have proved that surgery provides long term pain relief (>80%) [24, 25]. Retrospective studies [3] have shown that early surgery will benefit the patient by delaying the endocrine and exocrine insufficiency and providing better quality of life. As on current practice the treatments followed after failure of Frey’s procedure are increasing the dose of opioid analgesics, celiac plexus block, if needed redo surgery for residual disease [26], which either increases the cost as an additional procedure in a separate setting, or increases the dependence of opioids there by severely affecting the mental well being of the patient. Hence adding celiac plexus neurolysis to the current standard procedure in a single sitting as a part of multimodal approach will provide additional benefit to the patient not only by improving the psychological wellbeing but also by reducing the opioid intake thereby leading to a better quality of life (Figure 6).
Intra Operative Neurolytic Celiac Plexus Block
Celiac plexus is the relay station for all visceral afferent fibers [2]. There are two groups of celiac ganglia (right and left) and its most reliable location is in relation to the celiac trunk [27]. Pain caused by cancer or by chronic pancreatitis which relay through celiac plexus can be treated using NCPB [28]. It is traditionally used in the form of either USG, CT or EUS guided techniques [29]. Intraoperative method of NCPB was used originally for inoperable pancreatic or advanced GI malignancies for effective pain relief and offered good QOL [30, 31]. Surgical splanchnicectomy offered good long term pain relief of about 46% up to 48 months after splanchnicectomy [32]. This technique is extensively used for small duct disease. NCPB has a better pain control compared with splanchnicectomy [33]. Intraoperative method of NCPB in combination with lateral pancreatico jejunostomy was originally studied for treatment of pain in CCP with a 94.4% pain relief in a retrospective study of 34 patients. But this study was done only on patients with large duct disease [12].
Various studies on CPB have shown conflicting results with an average of 10%-40% long-term benefit beyond 24 weeks [34, 35, 36] with EUS guided techniques scoring over image guided methods of block [37, 38]. Most of the studies were done by plexus block using steroids/bupivacaine rather than neurolysis. Alcohol as neurolytic agent was studied mainly in pancreatic malignancy with 73%-85% significant response [39]. But long term results beyond 1 year were not available when alcohol is used as neurolytic for malignancy as this method is used only in those with advanced malignancy. Regarding concentration of alcohol solution we have used only 50% hydrated solution as alcohol concentration greater than 50% might cause neurological complications [17, 27]. Bilateral injection is favored by most of the studies compared to unilateral and central injections [38].
The basis for celiac plexus block is it abolishes the visceral afferent sympathetic fibers that pass through the celiac plexus and ganglion [39]. Upward migration leads to coronary branch of vagus ablation and leads to hypotension and more downward migration leads to ablation of plexus around SMA which leads to more diarrheas. Splanchnic vasodilatation caused by sympathetic blockade produces both diarrhea &postural hypotension. It is usually mild and manageable with crystalloid solutions [40, 41]. Its incidence was higher when more injections injected below the level of celiac axis and when a bilateral neurolysis was performed. Hence we always inject more (30 ml) above the celiac axis and 10 ml below in a 4 quadrant manner and maintaining the patient in 45 degree head up position for about 15 minutes meanwhile preparing the jejunal loop for anastomosis to avoid upward diffusion of drug. Possibly this could have produced lesser incidence of intra operative hypotension in our series but with more incidence of diarrhea and postural hypotension. The local injection related pain, referred shoulder pain, paraplegia, chronic debilitating diarrhea [27, 41] were never occurred in our study population.
Benefit of celiac plexus block (CPB) was least with previous pancreatic surgery and repeat blocks were unhelpful [34]. Hence it is always better to assess the patients at risk of developing recurrent pain and do it intra-operatively in a single sitting. In contrast to previous studies in which the effect of percutaneous NCPB is less in chronic pancreatitis when compared to malignancy due to adhesions which limits the diffusion of drug40, our study has proved that neurolysis in chronic pancreatitis using intraoperative method is effective as the diffusion of drug is better when injecting the drug at 4 quadrants in a controlled manner, when compared with radiological and endoscopic techniques. If recurrence of pain occurs repeated blocks after a neurolysis can be done even though we had difficulty in 36% using conventional percutaneous method. We want to express our view that there is a difference in pain relief according to the mode of neurolysis and this intra operative method is an easy, controlled and better way of neurolysis even though it is operator dependent. The diffusion of the drug is better, bilateral injections can be done without change in position unlike in EUS and percutaneous techniques and it can be easily done by the operating surgeon himself without a need for an endoscopic or interventional expertise more importantly without adding much cost to the procedure in a single sitting.
NCPB achieves better results in patients with small duct disease. Smaller the diameter better is the response. But if the patient is not responding to any kind of analgesics and neurolysis prior to surgery (centralized pain state [19]) the response to NCPB is still poor. The success rate of the procedure in placebo group is fairly comparable to previous study results (80-90%).There is even decrease in early post-operative pain in NCPB group. The exact reason for this is not known. But the possible mechanism that could have caused this difference may be, less post-operative ileus thereby decrease in the abdominal distension and eventually the parietal wound pain.
NCPB improves weight gain significantly. It may be explained by very good pain control and increased caloric intake. The 35% decrease in insulin/OHA intake in group I may be explained by the improved nutrition and mental wellbeing with possible effect on diabetic status.
NCPB improves the QOL in all types of pancreatitis. Various studies and RCTs on celiac plexus block also have shown to improve QOL in both chronic pancreatitis and unresectable pancreatic cancer [2, 41, 42]. SF36 is routinely used for assessing the QOL in pancreatic pathology. SF -12 version 2 questionnaire is equally good compared to SF 36 and EORTC Qlq–C30 for evaluation of QOL in pancreatic pain due to CP [43, 44, 45]. It is more reliable and easier to use.
Since opiate dependency with annoying side effects, increases the chances of centralized pain state [19] we strongly believe that adding neurolysis definitely had an additional benefit to these patients when combined with a standard procedure especially addressing the unidentifiable neurogenic mechanism rather than as an adjunct to incomplete surgery.
In accordance with the suggested multifactorial origin of pancreatitis pain and to address all well-known theories thereby improving the QOL, we suggest combined NCPB with Frey’s procedure for a complete solution in a single sitting without affecting the morbidity and mortality.
The injection of alcohol is operator dependent. Better methods to identify the plexus/ganglion intraoperatively and finding better agent for neurolysis may improve the long term effectiveness of the neurolysis. This article may shed some light on future combinations like neurolysis with intraoperative lithotripsy [46], splanchnicectomy etc. which can also theoretically give better results.
I sincerely thank our patients for participating in this study. Dr. Moses Vikraman Amarjyothi helped in English verification of the manuscript. Ms. Jegadeeswari helped in the data collection. Dr. Mohammed Ali & Dr. Heber David helped in statistical verification.
This trial was registered at clinical trial.gov. NCT02735330.The interim analysis data were presented at AP-HPBA meet at Singapore March 2105 and awarded as best paper.
The authors have no conflicts of interests to declare.