Shadi Seraji*, Svetoslav Bardarov and Claudia Ravens
Department of Obstetrics and Gynecology, South Nassau Communities Hospital, USA
*Corresponding Author:
Shadi Seraji
Department of Obstetrics and Gynecology
South Nassau Communities Hospital Oceanside
New York, USA
Tel: 15166524222
E-mail: shadiaghilimd@gmail.com
Received date: May 08, 2017; Accepted date: June 16, 2017; Published date: June 21, 2017
Citation: Seraji S, Bardarov S, Ravens C. Intrapartum Hemorrhage secondary to Decidua Peritonea. Gynecol Obstet Case Rep 2017, 3:2. doi:10.21767/2471-8165.1000052
Keywords
Decidua Peritonea; Endometriosis; Peritoneal implants; Hemorrhage
Introduction
The presence of decidualized endometrial implants has been widely reported in the past. These generally involve the ovaries, the uterus and cervix [1]. They have also been reported in old cesarean section and episiotomy scars [2]. Less commonly they can be found involving the peritoneum. They are often asymptomatic and discovered during cesarean sections. They have also been detected histologically in visceral serosa of various abdominal organs and in retroperitoneal lymph nodes [3]. We present a case report of peritoneal implants involving the parietal peritoneum and the fallopian tubes in an asymptomatic 33-year-old, prima-gravida Asian woman undergoing a primary cesarean section.
Case Report
A 33-year-old prima-gravida female, admitted at 39 weeks 4 days of gestation, for prolonged monitoring when the NST at her PMDs office showed 2 variable decelerations. Her history was significant for endometriosis and infertility, with pregnancy achieved by in vitro fertilization. Prenatal course was unremarkable except for sero-positivity of HSV II for which she was on Valcyclovir. She was found to be dilated and admitted for delivery. She progressed in labor and after she had an epidural developed hypotension which was resolved subsequently she developed a non-reassuring fetal tracing and taken to the operating room for urgent abdominal delivery. She was delivered of a female infant weighing 6lb 9.1oz, with APGAR’s of 9/9 by Manuscript Click here to download Manuscript corrected Decidua Peritonea.docx Cesarean Section. The approach was through a pfannenstiel incision with a low transverses uterine incision in the standard fashion. Intraoperatively, after closure of the uterine incision the uterus was noted to be well contracted. However, excessive bleeding was noted from the posterior aspect of the uterus and on inspection the entire Cul-De-Sac and pelvic side walls and fallopian tubes were noted to be covered with small papules, whitish in color and measuring 1 mm to 5 mm in size. The underlying serosa of the entire area appeared hyperaemic and “beefy red”, which easily bled with any contact. This was more severe of the left fallopian tube, where bilateral hydrosalpinx and adhesions were also noted. Hemostasis was eventually achieved using a combination of electro-cautery, Surgiflo® hemostatic matrix and Evicel® fibrin and a left partial salpingectomy. Estimated blood loss was 2,500 ml, resulting in drop of H/H from 13.7/38.8 on admission to 6.8/19.7. Tranexamic acid was given intravenously as well as 4 units of PRBCs, one unit of Cryoprecipitate and FFP each, intraoperatively resulting in a post-operative H/H of 14.7/40.8. The patient was observed in the intensive care unit overnight and had an unremarkable post-partum course and discharged home on day 4.
Pathological Findings
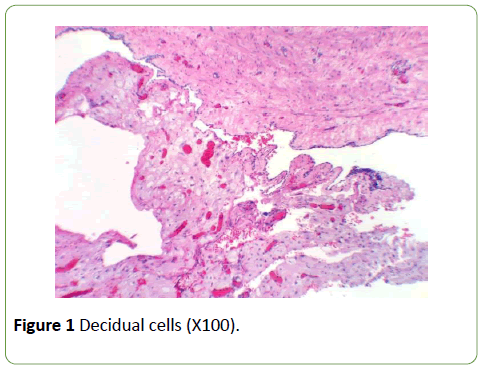
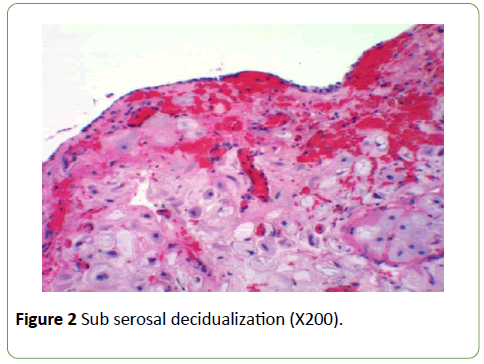
Standard Hematoxylin and Eosin stain was used. Decidualized tissue, with large polygonal eosinophilic cells was noted partially covered by mesothelium attached to the fallopian tube (Figures 1 and 2). Mitotic activity, nuclear polymorphism or nuclear membrane irregularities were not observed. No endometrial glands or desmoplastic reaction were noted.
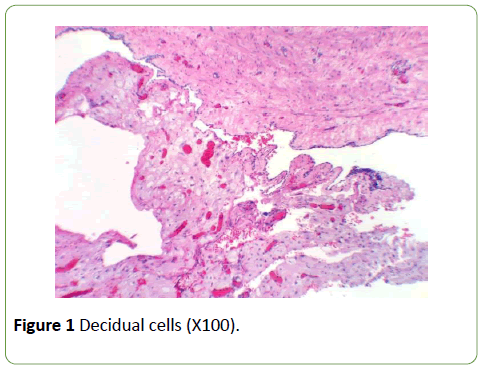
Figure 1:Decidual cells (X100).
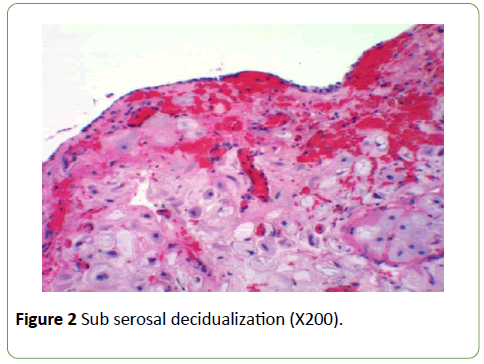
Figure 2:Sub serosal decidualization (X200).
Discussion
Ectopic decidualized implants have been widely reported in various locations in the pelvis and abdomen. Invariably these are thought to have developed as a result of progestational effect of pregnancy hormonal milieu and resolve spontaneously at pregnancy termination [4]. Rare cases involving post-menopausal patient have also been reported [5]. They are often asymptomatic and noted during cesarean sections with no significant sequela.
They occasionally and rarely can cause complications directly, or indirectly as a result of their location and appearance. They have involved ovarian endometriomas, mimicking the appearance of neoplastic lesions [6,7]. Acute appendicitis has also been reported as a result of deciualization of endometrial cells on it [8,9]. Several cases of the same within old abdominal wall scars [10], especially cesarean sections [2] are noted. The most acute presentation is seen in cases of florid diffuse peritoneal deciduosis, when it can mimic carcinomatosis [11] or bleeding and hemorrhage antenatally [12] or during the delivery as occurred in the current case. Diagnostic modalities are limited in scope and limited to endometriotic cysts [13,14] and therefore not helpful. It is not clear if endometriotic cells need to be present prior to pregnancy in order for decidualization to take place. There are multiple incidence of decidualized tissue found where endometriotic cell are not usually found [15]. Moen et al. reported that 77% of women with proven endometriosis showed decidualization of their biopsies versus only 31% of those without [16]. Like the majority of these reports, the case patient had extensive endometriosis and infertility making in vitro fertilization necessary. Zayestev et al. presented two theories to explain ectopic peritoneal lesions [17]. The more widely accepted theory suggests that sub-coelomic mesenchymal cells undergo a metaplasia under progesterone effect. The second theory explains that the decidual cells are already distributed in the peritoneum. Deciduosis is a clinicopathologic process distinct from endometriosis [18,19].
Conclusion
The acute presentation in this case in an asymptomatic patient and its subsequent complication of acute bleeding, large volume blood loss and ICU admission was not easily predictable or preventable. However, awareness of its possibility in patients with pre-existing endometriosis must be considered by the clinician in order to facilitate patient education and management planning to assure an acceptable outcome. This could be potentially a critical step to consider the decidualization of endometriotic lesions. More over further evaluation should be made to see what predisposing factors, if any can contribute to this process, as it is clear that not all endometriosis decidualizes.
References
- Kindra P, Sen A, Sharma J (2006) Ectopic decidual reaction: A case report. MJAFI 62: 280-281.
- Alam S, Mushtaq H, KafeelS (2013)Deciduosis in a cesarean scar. JIMDC2: 32-34.
- Mills SE (1983) Decidua and squamous metaplasia in abdominopelvic lymph nodes. Int J GynecolPathol 2: 209-215.
- Bolat F, Canpolat T, Tarin E (2012) Pregnancy-related peritoneal ectopic decidua (deciduosis): Morphology andclinical evaluation. Turk PatolojiDerg28: 56-60
- Kim HS, Yoon G, Kim BG, Song SY (2015) Decidualization of intranodal endometriosis in a postmenopausal woman. Int J ClinExpPathol8:1025-1030.
- Barbieri M, Somigliana E, Oneda S, Acaia B, Fedele L (2009) Decidualized ovarian endometriosis in pregnancy: A challenging diagnostic entity. Hum Reprod 24:1818-1824.
- Tazegul A, Kerimoglu OS, Dogan NU, Yilmaz SA, Celik C (2013) Decidualized endometrioma mimicking ovarian cancer during pregnancy. Case Rep Obstet Gynecol.
- Murphy S, Kaur A, Wullechleger M (2016)Endimetraldecidualization: A rare cause of acute appendecitis during pregnancy. J Surg Case reports 4: 1-3.
- Dogan E, Okyay E, Saatli B, Sarioglu S (2012)Tubo-ovarian abscesses formation from decidualized ovarian endometrioma after appendiceal endometriosis presenting as acute appendicitis inpregnancy. Iran J Reprod Med 10: 275-278.
- Kilinc N, Yalinkaya A, Ozaydin M (2002)Nondecidualizad and decidualized endometriosis of abdomial wall. Turk J Med Sci 32: 505-508.
- Adhikari L, Shen R (2013) Florid peritoneal deciduosis mimicking carcinomatosis in a primagravidapatient. Int J ExpPathol6:2615-2619.
- Aggarwal I, Tan P, Mathur M (2014) Decidualised fallopian tube endometriotic implant causing spontaneous haemoperitoneum in twin pregnancy. BMJ Case Rep.
- Nakai G, Kitano R, Yoshimizu N, Yamamoto K, Higashiyama A, et al. (2015) Acase of bilateral decidualized endometriomas during pregnancy: Radiologic-pathologic correlation. Kobe J Med Sci 61:40-46.
- Morisawa N, Kido A, Kataoka M, Minamiguchi S, Konish I, et al. (2014) MRI manifestations of decidualized endometriotic cyst. J Assist Tomogr38:879-884.
- Wu DC, Hirshowitz S, Natarajan S (2005) Ectopic decidua of pelvic lymph nodes: A potential diagnostic pitfall. Arch Pathol Lab Med 129: e117-e120.
- Moen MH, Muus KM (1991) Endometriosis in pregnant and non-pregnant women at tubal sterilization. Hum Reprod 6:699-702.
- Zaytsev P, Taxy B (1987) Pregnancy-associated ectopic decidua. Am J Surg Path 11:526-530.
- Skukla S, Pujani M, Singh SK (2008) Ectopic decidual reaction mimicking peritoneal tubercles. Indian J Pathol&Microb51:519-520.
- Rogers W, Seckinger D (1965)Decidualtissue as a cause of intra-abdominal hemorrhage during labor. Obst&Gynec 25: 391-397.