- (2004) Volume 5, Issue 3
Ioannis Baraboutis1, Athanasios Skoutelis2
1Hellenic Center for Infectious Diseases Control. Athens, Greece.
2Infectious Diseases Division, Department of Medicine, University Hospital of Patras. Rio/Patra, Greece
Received: 05 February 2004 Accepted: 09 February 2004
Cystadenocarcinoma; Diagnosis; Diagnosis, Differential; Laboratory Techniques and Procedures; Pancreatic Cyst; Pancreatic Neoplasms; Tomography, Spiral Computed; Tuberculosis, Gastrointestinal; Ultrasonography
CA: carbohydrate antigen; HIV: human immunodeficiency virus
A 45 year old African-American woman from Chicago, Illinois was evaluated because of “hot flashes” and an 11 kg weight loss over three months without fever, respiratory or abdominal symptoms. Her past medical history was unremarkable for chronic diseases or hospitalization. She was not a smoker and only drank socially. She denied any foreign travel and had no risk factors for human immunodeficiency virus (HIV) infection. She had a normal white blood cell count and differential. Hepatic transaminases, alkaline phosphatase, carbohydrate antigen (CA) 19-9 and HIV assays were all normal. The chest radiograph was completely normal. She was found to be reactive to tuberculin purified protein derivative with 20 mm of induration. The patient reported a non-reactive skin test which had been done during an outpatient visit by her primary care physician ten years previously.
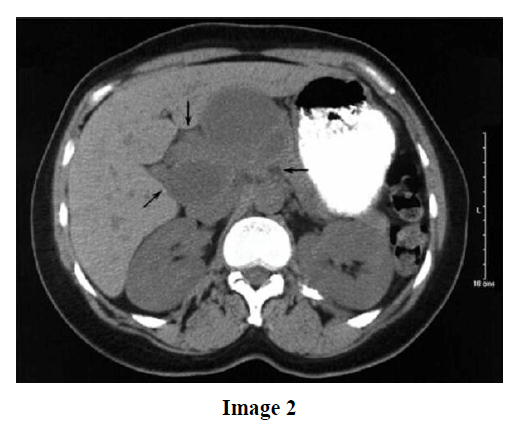
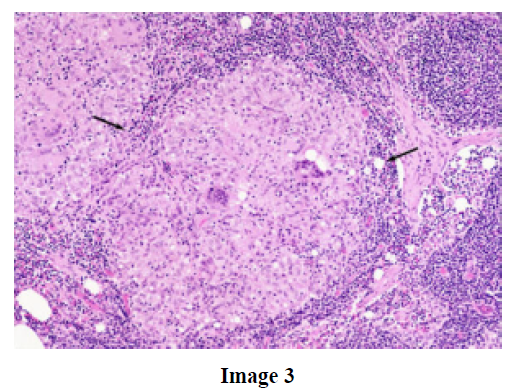
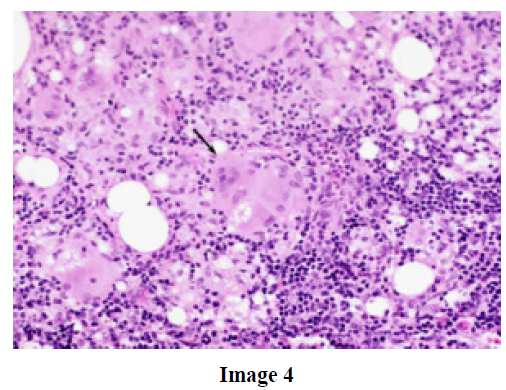
Upon further testing computed tomography of the abdomen and retroperitoneum demonstrated a 6.3x9.1 cm complex cystic mass in the neck and body of the pancreas (Images 1 and 2), displacing the liver anteriorly. Because of a suspected pancreatic adenocarcinoma, a laparotomy was advised. Upon surgical access to the area of the mass, multiple abnormal lymph nodes were observed. During further manipulations, the mass was entered and a large amount of yellow fluid was recovered. Biopsies from the pancreatic mass and lymph nodes revealed multiple granulomas (arrows) with areas of caseating necrosis and clusters of multinucleated giant cells (Image 3). A close view of a multinucleated giant cell from the peripancreatic lymph node biopsy is shown in Image 4. The planned Whipple procedure was cancelled. Stains for funghi and mycobacteria, and polymerase chain reaction assay for Mycobacterium tuberculosis were negative; however, pan-susceptible Mycobacterium tuberculosis was isolated from the culture after four weeks of incubation. This case represents the typical presentation for tuberculosis of the pancreas, masquerading as a tumor. This patient received 300 mg of isoniazid daily, 600 mg of rifampin daily, 1200 mg of ethambutol daily, and 1.5 g of pyrazinamide daily for two months and completed therapy with ten additional months of isoniazid and rifampin at the above doses. The symptoms resolved and follow-up imaging showed a complete resolution of the mass.

Abdominal infection with tuberculosis commonly affects the spleen, liver, ileocecal region and peritoneum [1]. Tuberculosis of the pancreas is considered a rare entity in developed countries, occurring mostly in the setting of HIV infection or immunosuppression for transplantation [2, 3]. Nevertheless, there has been an increase in the number of cases reported involving immunocompetent patients, originating mostly from developing countries [1, 4, 5, 6, 7, 8, 9]. In a large portion of these cases, there is neither concomitant disease elsewhere nor evidence of miliary dissemination [4].
The pathogenesis of pancreatic tuberculosis remains speculative and may involve: 1) pancreatic involvement during miliary disease, 2) hematogenous dissemination from an occult site elsewhere (possibly the lungs) and 3) direct spread from contiguous lymph nodes [1]. In support of the last theory, in most of the cases with perceived isolated pancreatic tuberculosis (such as in our patient), there is radiographic and/or histopathologic evidence of regional lymph node involvement [1].
Pancreatic tuberculosis may present with protean manifestations, including various combinations of systemic and abdominal symptoms [1, 4]. Interestingly, our patient did not complain of any abdominal symptoms whatsoever. A laboratory workup is also commonly non-specific. The purified protein derivative test may or may not be positive [1, 4]. Imaging with abdominal ultrasound (US), computed tomography (CT) or magnetic resonance usually reveals complex multicystic pancreatic masses, most frequently at the head of the pancreas [1]. The above constellation of findings frequently leads to the erroneous diagnosis of pancreatic malignancy or pseudocyst, and, quite often, to unnecessary laparotomies [5, 6, 7, 8, 10, 11]. Fine needle aspiration, guided by CT or US, may prevent these unnecessary procedures [12].
Diagnosis of pancreatic tuberculosis is usually done on histopathologic and microbiologic grounds [1, 4]. Biopsies reveal granulomas in over 60% of the cases (12/16 obtained by laparotomy and 10/16 obtained by fine needle aspiration in one series), with many of them exhibiting caseation necrosis (6/16 from the same series) [4, 13]. Smears for acid-fast bacilli are seldom positive and the role of nucleic acid amplification techniques for negative smears is under study. The yield of mycobacterial cultures may be higher [1, 4, 13].
Most cases of pancreatic tuberculosis have responded well to anti-tuberculin therapy. The most frequently used combinations from our review of the literature were isoniazid/ rifampin/pyrazinamide/streptomycin or ethambutol and isoniazid/rifampin/ streptomycin (older studies) [4, 7, 9]. The duration of the therapy is usually 6-12 months [1, 4, 5, 6, 7, 8, 10, 11, 14]. In one series, the mean time to radiographic resolution was 132 days [4]. Usually no surgical intervention is necessary and recurrences are rare [4].