- (2012) Volume 13, Issue 2
Claudio Ricci, Riccardo Casadei*, Salvatore Buscemi, Francesco Minni
Department of Surgical and Anesthesiological Sciences, Alma Mater Studiorum, University of Bologna, “S.Orsola-Malpighi” Hospital. Bologna, Italy
Received December 17th, 2011 - Accepted January 10th, 2012
Context Post-pancreatectomy hemorrhage is one of the most common complications after pancreaticoduodenectomy. Objective To evaluate the late post-pancreatectomy hemorrhage rate according to the International Study Group of Pancreatic Surgery criteria and to recognize factors related to its onset. Methods A prospective study of 113 patients who underwent pancreaticoduodenectomy was conducted. Late post-pancreatectomy hemorrhage was defined according to the criteria of the International Study Group of Pancreatic Surgery. Demographic, clinical, surgical and pathological data were considered and related to late post-pancreatectomy hemorrhage. Results Thirty-one (27.4%) patients had a post-pancreatectomy hemorrhage. Twenty-five (22.1%) patients developed late post-pancreatectomy hemorrhage: 19 (16.8%) grade B, 6 (5.3%) grade C. Surgical re-operation was performed in 2 out of the 25 cases with late post-pancreatectomy hemorrhage (8.0%) grade C associated with postoperative pancreatic fistula. At univariate analysis, the only factor significantly related to late post-pancreatectomy hemorrhage was postoperative pancreatic fistula (P<0.001) and pancreatic anastomosis (P=0.049) independently increased the risk of late hemorrhage. Conclusion In patients undergoing pancreaticoduodenectomy, the criteria introduced by International Study Group of Pancreatic Surgery to define late postpancreatectomy hemorrhage are related to a higher incidence of hemorrhage than previously detected because they considered also mild hemorrhage.
Pancreatectomy, Hemorrhage, Pancreatic Fistula
ASA: American Society of Anesthesiologists; ISGPS: International Study Group of Pancreatic Surgery; PPH: post-pancreatectomy hemorrhage
Pancreaticoduodenectomy is a technically complex procedure owing to its significant postoperative morbidity and mortality rate. However, while the mortality rate is lower in high volume centers, the morbidity rate still ranges from 22.7 to 57% [1, 2]. Morbidity most frequently results from pancreatic fistulas and delayed gastric emptying [1, 2]. Postpancreatectomy hemorrhage (PPH) is reported less frequently from 5 to 12% [3, 4, 5, 6] but, in some patients, it represents a devastating complication [3]. In 2007, the International Study Group of Pancreatic Surgery (ISGPS) proposed a new classification system of PPH [7] with the aims to allow a proper diagnosis and to evaluate the severity of the hemorrhage.
While the causes of early bleeding are well recognized (usually they are the result of simple technical failure), the factors related to late hemorrhage are still uncertain. The aims of our study were to evaluate the factors influencing late PPH in patients undergoing pancreaticoduodenectomy using the criteria of the International Study Group of Pancreatic Surgery (ISGPS) classification and to recognize factors related to its onset.
A prospective study of 113 consecutive patients who underwent pancreaticoduodenectomy at the First Surgical Clinic of the University of Bologna, S.Orsola- Malpighi Hospital, from January 2009 to January 2011 was conducted. Overall postoperative mortality and morbidity were reported according to the Clavien- Dindo classification system [8]. The diagnosis of postpancreatectomy hemorrhage was evaluated for each patient according to the criteria of the International Study Group of Pancreatic Surgery (ISGPS) [7]. Postpancreatectomy hemorrhage was considered extraluminal (extraenteric, bleeding into the abdominal cavity) or intraluminal (intraenteric) and early (less than, or equal to, 24 h after the end of the operation) or late (greater than 24 h after the end of the operation). The diagnosis and severity of PPH was based on clinical aspects, hemoglobin concentration and type of treatment. Severity of hemorrhage was considered as mild (small or medium volume blood loss from drains; nasogastric tube with decrease in hemoglobin concentration less than 3g/dL; mild clinical impairment of the patient; no therapeutic consequence, or at most the need for noninvasive treatment with blood transfusions of 2-3. units packed cells within 24 h of end of operation or 1-3 units if later than 24 h after operation) or severe (large volume blood loss with drop of hemoglobin level equal to, or greater than, 3 g/dL; clinically significant impairment; need for blood transfusions (more than 3 packed cells) and for invasive treatment as well as interventional angiographic embolization or relaparotomy). Three grades of severity were recognized: PPH grade A is an early, intra- or extra-luminal, mild hemorrhage and it has no major clinical impact; PPH grade B can be early, intra- or extra-luminal and severe or late; intraor extra-luminal and mild hemorrhage. Early PPH grade B requires adjustment of a given clinical pathway, including additional diagnostic examinations and intervention; late PPH grade B, need observation, blood count, transfusion of fluid or blood but it does not require interventional therapy. Finally, PPH grade C is late, intra- or extra-luminal and severe hemorrhage. It requires interventional angiographic embolization or relaparotomy and should always be considered potentially life threatening [7].
Demographic data (age and sex), preoperative factors (presence of comorbidities, American Society of Anesthesiologists (ASA) score [9], operative factors (type of pancreaticoduodenectomy: pylorus-preserving pancreaticoduodenectomy or pancreaticoduodenectomy with partial gastrectomy, extended or standard; intraoperative blood loss, intraoperative blood transfusion), characteristics of the pancreas remnant (texture and Wirsung duct dilatation greater than 3 mm), treatment of the pancreatic stump (with or without anastomosis), presence of postoperative pancreatic fistula and pathological diagnosis were reported for each patient and related to late PPH.
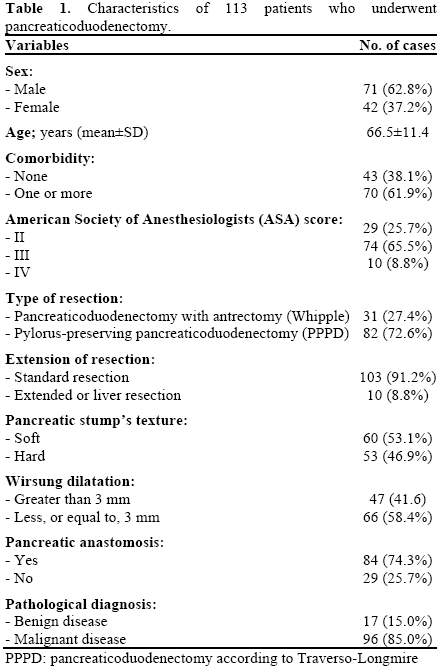
The characteristics of the 113 patients who underwent pancreaticoduodenectomy are summarized in Table 1. The patients were more frequently male (with a mean age of 66.5±11.0 years) one or more comorbidities and ASA score equal III. Type of resection was more frequently a standard pylorus-preserving resection. Pancreas remnant was usually soft and without Wirsung dilation; its treatment was usually with a pancreaticojejunostomy. Malignant diseases (52 pancreatic head ductal carcinomas, 54.2%; 17 carcinomas of the papilla of Vater, 17.7%; 13 bile duct cancers, 13.5%; 6 duodenal carcinomas, 6.3%; 7 neuroendocrine carcinomas, 7.3%; and 1 pancreatic metastasis, 1.0%) were more frequent than benign diseases (6 chronic pancreatitis, 35.3%; 5 intraductal papillary mucinous adenomas, 29.4%; 4 serous cystic tumors, 23.5%; and 2 autoimmune pancreatitis, 11.8%).
A postoperative pancreatic fistula was defined as a drain output of any measurable volume of fluid on or after the third postoperative day, with an amylase content greater than three times the serum amylase activity. Three grades of postoperative pancreatic fistula (A, B, C) were proposed according to the criteria of the International Study Group of Pancreatic Fistula [10]. Postoperative mortality was defined as all deaths within 30 days after surgery or before discharge from the hospital. Re-operation was defined as any surgical procedure performed in the first 30 postoperative days or before discharge from the hospital; indications for surgery have previously been described [3].
Pancreaticoduodenectomy was performed according to two different procedures: pylorus-preserving pancreaticoduodenectomy (Traverso-Longmire technique) or pancreaticoduodenectomy with antrectomy (Whipple technique). Usually, we performed pylorus-preserving pancreaticoduodenectomy as the standard procedure; in cases with possible malignant involvement of the pylorus or a history of previous Billroth II resection, a Whipple procedure was preferred. At laparotomy, hepatic and peritoneal metastases were excluded; the duodenum was mobilized by means of a Kocher maneuver to assess resectability. En bloc resection of the duodenum with 10-20 cm of the jejunum distal to the ligament of Treitz, pancreatic head, common bile duct, gallbladder was performed. In the classical Whipple procedure an antrectomy was added. The common bile duct was resected proximal to its confluence with the cystic duct in malignancy, distal in benign disease. A standard lymph nodes dissection was performed. Usually the pancreas remnant was anastomosed with a jejunal loop. In selected cases of high risk patients (age greater than 80 years with important co-morbidities) with very high risk pancreatic stump (very soft pancreatic parenchyma, with Wirsung duct not visible) the pancreatic resection was extended distally of 4-5 cm and the closure of the pancreas remnant was performed. Pancreaticojejunostomy was performed according two different techniques: end-to-end binding pancreaticojejunostomy according to the Peng procedure [11] or end-to-side, duct-to mucosa pancreaticojejunostomy. The majority of cases were treated without pancreatic stenting. Two intraperitoneal drains were placed: the first, posterior to the hepaticojejunostomy, the second, on the anterior surface of the pancreaticojejunostomy or of the closed pancreas remnant. Subcutaneous somatostatin, 200 μg subcutaneously three times a day, was initiated on the first day after surgery. Routine intravenous perioperative antibiotic (1 g cefuroxime) was given three times daily. Amylase and lipase levels in serum and in abdominal drain were monitored daily: if amylase and lipase in abdominal drain were normal on days 4 after surgery, we removed the abdominal drains. Nasogastric tube was removed on day 4 after surgery and enteral diet was started if there was no sign of anastomotic leakage.
The study protocol conforms to the ethical guidelines of the “World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects” adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004. The signed informed consent was obtained from each patient for any surgical and clinical procedure according to the common clinical practice. The a priori approval by the appropriate institutional review committee was not required because the data of the present study were collected in the course of the usual clinical practice.
Means, standard deviations and frequencies were used to describe the data. The Fisher’s exact test, the linearby- linear chi squared and the Mann-Whitney U tests were applied when appropriate to conduct the univariate analysis. Multivariate analysis was performed by using logistic regression. All statistical analyses were made by running the SPSS for Windows (SPSS Inc., Chicago, IL, USA, version 13.0) by means of a personal computer. Two-tailed P values less than 0.05 were considered statistically significant.
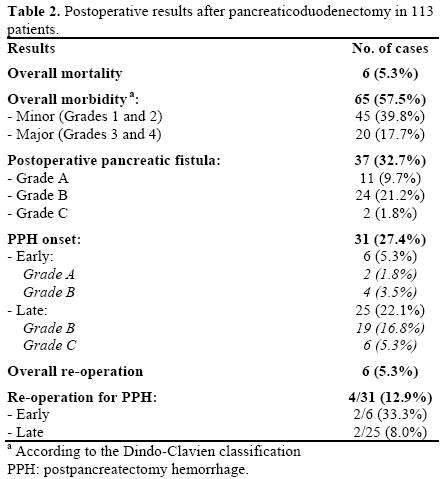
The results after pancreaticoduodenectomy are shown in Table 2. Overall postoperative mortality and morbidity rates were 5.3% (6 cases) and 57.5% (65 cases, of which the major part (45 cases, 39.8%) of grade 1-2 according to Clavien-Dindo classification), respectively. Postoperative pancreatic fistula rate was 32.7% (37 cases) even if 11 cases (9.7%) had grade A. Thirty-one (27.4%) patients had a PPH; PPH was early in 6 cases (5.3%) and late in 25 cases (22.1%). Among early hemorrhage, 2 cases (1.8%) were grade A and 4 cases (3.5%) were grade B. Among late PPH, 19 cases (16.8%) were grade B and 6 cases (5.3%) were grade C. Overall re-operations were performed in 6 patients (5.3%). Within patients with PPH, re-operations were performed in 4/31 (12.9%) patients: 2/6 (33.3%) for early, grade B hemorrhage, consisting in a completion pancreatectomy because of the massive bleeding from the pancreatic stump; and 2/25 (8.0%) for late grade C hemorrhage associated with postoperative pancreatic fistula, consisting in the sutures of the bleeding vessels that were in one case a branch of the splenic vein and in the other case a branch of the hepatic artery. The other 4 patients with late PPH grade C required blood transfusion and interventional angiographic embolization of a branch of the hepatic artery. In the remaining 19 patients with late PPH grade B, 4 (21.1%) required blood transfusion (1-3 units of packed cells; 2 because they had cardiopathy with a decreased of hemoglobin concentration between 1 and 2 g/dL and 2 patients because presented a rapid decrease of hemoglobin concentration between 2 and 3 g/dL) and 15 (78.9%) were monitored only with blood count because they had a decreased of hemoglobin concentration between 1 and 2 g/dL and they were in well clinical conditions.
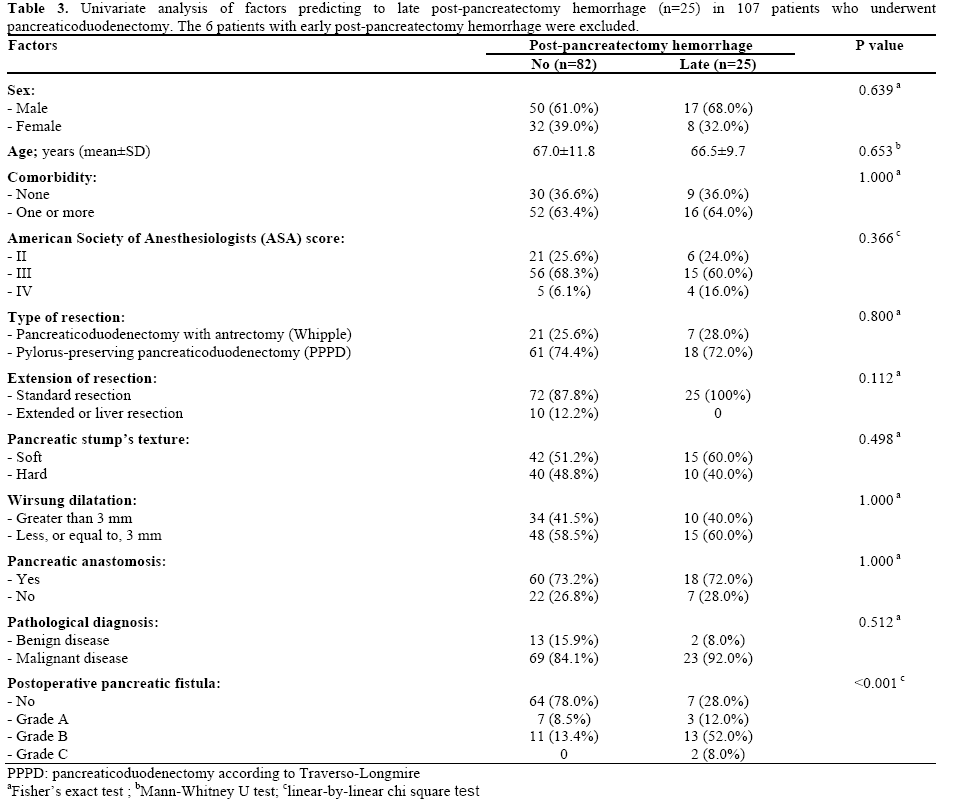
For the evaluation of the factors influencing late PPH, the 6 patients with early bleeding were excluded because the present study is focused to late hemorrhage. At univariate analysis, sex, age, presence of comorbidities, ASA score, type and extension of resection, texture of the pancreatic stump, Wirsung duct dilatation, treatment of the pancreatic stump and pathological data were not significantly related to the presence of late PPH. Postoperative pancreatic fistula was the unique factor significantly related to the presence of late PPH: patients without postoperative pancreatic fistula were rarely associated with late PPH (28.0% versus 78.0%) (P<0.001); therefore, 72.0% of the patients with late PPH had postoperative pancreatic fistula (grade A, 12.0%; grade B, 52.0%; grade C, 8.0%) versus 22.0% of the patients with no PPH (grade A, 8.5%; grade B, 13.4%; no patients with grade C) (Table 3).
Multivariate analysis showed that the risk of late PPH and pancreatic anastomosis entered the procedure; the risk of late PPH significantly increased with increasing postoperative pancreatic fistula severity (OR: 4.93; 95% CI: 2.46-9.85; P<0.001) and in case of pancreatic anastomosis (OR: 4.22; 95% CI: 1.00-17.7; P=0.049).
Post-pancreatectomy hemorrhage is a life threatening complication and remains a significant cause of morbidity following pancreaticoduodenectomy. Before the introduction of the ISGPS definition, several authors reported a prevalence of PPH following pancreaticoduodenectomy which ranged from 5 to 12% [3, 4, 5, 6]. The ISGPS definition of PPH recognized early and late hemorrhage in relation to the time of onset; mild or severe due to clinical conditions, decrease of hemoglobin concentration and type of treatment. To our knowledge, only three previous studies have reported the occurrence of PPH in patients undergoing pancreaticoduodenectomy, using this classification system. Rajarathinam et al. [12] reported a PPH rate of 3.1%, but these authors considered only severe hemorrhage and did not report the overall PPH rate. Sanjay et al. [13]. reported a PPH rate of 10.4%, but these authors considered only late PPH and defined hemorrhage as postoperative bleeding from the surgical site with a drop in hemoglobin concentration greater than 3 g/dL with peripheral circulatory impairment requiring medical intervention. Eckardt et al. [14] reported a PPH rate of 8.4% but the hemorrhage was defined as a decrease in hemoglobin level of at least 2 g/L, hemodynamic instability and/or requirement for more than 2 units of blood transfusion with signs of gastrointestinal bleeding, intra-abdominal bleeding, or both. In our experience, using the ISGPS definition, the overall PPH rate was 27.4%, with prevalence of late PPH as compared to early PPH (22.1% and 5.3%, respectively). The correct application of the ISGPS definition probably increased the overall incidence of PPH and in particular of late PPH (22.1%) because it also considers mild hemorrhage as a drop in hemoglobin concentration less than 3 g/dL. In our experience, in fact, we considered post-pancreatectomy hemorrhage a decrease in hemoglobin level of at least 1 g/dL. Among the 19 patients with late PPH grade B, the vast majority of cases (17; 89.5%) had a decrease in hemoglobin inferior to 2 g/dL and only 2 (10.5%) had a decrease between 2 and 3 g/dL. Thus, if we consider only patients with severe hemorrhage with a drop of hemoglobin concentration equal to, or greater than, 3 g/dL (PPH grade C), the incidence of late PPH resulted much more low than overall late PPH rate (5.3% versus 22.1%). Finally, if we consider all the patients with clinical impact and therapeutic consequences, the incidence of late PPH was 8.8% (8 cases, that is 6 PPH grade C and 2 PPH grade B). Thus, about two-third of the patients were classified as late PPH grade B, with mild hemorrhage and they had well clinical conditions and did not require blood transfusion or interventional angiographic embolization. The ISGPS classification of the PPH resulted very useful to diagnose and recognize the different severity of the postpancreatectomy hemorrhage.
Regarding factors related to late PPH, actually they are still unknown. The exact mechanism of hemorrhage after pancreatic surgery is unclear but the presence of local sepsis and association with a pancreatic fistula appear to be common predisposing factors [13, 15, 16, 17]. Brodsky and Turnbull [18] have reported that 75% of their patients having a late hemorrhage had an associated pancreatic leak. Yekebas et al. [3] reported a large cohort of patients who underwent pancreatic resection in which a pancreatic fistula was significantly associated with PPH. These authors pointed out that PPH associated with a preceding postoperative pancreatic fistula was more frequently lethal than the group without a postoperative pancreatic fistula. However, the real temporal correlation between PPH and a postoperative pancreatic fistula remains unknown. In our study, we showed a statistically significant correlation between the presence of a postoperative pancreatic fistula, with major clinical impact (grades B and C), and the development of late PPH. In fact, about two-thirds of patients who developed late PPH presented a postoperative pancreatic fistula grade B or C, suggesting that pancreatic juice and local infection could be the cause of the vascular injury. It is well-known that the closure of pancreatic stump, increase the risk of pancreatic fistula [10] but, in our experience, it does not increase the risk of late PPH.
In conclusion, in patients undergoing pancreaticoduodenectomy, the incidence of late postpancreatectomy hemorrhage, according the criteria of the International Study Group of Pancreatic Surgery, resulted higher than previously detected, even if the hemorrhage was quite always mild, without clinical impact and therapeutic consequences. Thus, the ISGPS classification of PPH seems to be a useful system able to diagnose and stratify the severity of the postpancreatectomy hemorrhage. The onset of late PPH seems to be related to a postoperative pancreatic fistula having a clinical impact.
The authors declare that they have no conflict of interest