Shozo Sueda1 and HiroakiKohno2
1Department of Cardiology, EhimePrefectural Niihama Hospital, Japan
2Department of cardiology, TsukazakiHospital, Japan
*Corresponding Author:
Shozo Sueda
The Department of Cardiology, EhimeNiihama Prefectural Hospital, Hongou 3choume 1-1, Niihama City, Ehime 792-0042,Japan
Tel: +81-897-43-6161
Fax: +81-897-41-2900
E-mail: EZF03146@nifty.com
Received Date: December 07, 2015 Accepted Date: December 15, 2015 Published Date:December24, 2015
Citation: Sueda S, Kohno H. Less Racial Difference in Coronary Artery Spasm; Caucasian versus Japanese. Interv Cardiol J 2015, 1:1. DOI: 10.21767/2471-8157.10007
Keywords
Coronary artery spasm, Caucasian, Japanese, Racial difference
Racial difference about coronary artery spasm between Caucasian and Japanese patients was reported in the past study [1]. Pristipino et al. reported the three times higher provoked spasm incidence in Japanese patients with acute myocardial infarction compared with those Italian Caucasian patients [2]. In the United State of America and Europe, the majority of cardiologists did not perform the spasm provocation tests in the cardiac catheterization laboratory, whereas Japanese cardiologists have been interested in performing the spasm provocation tests for more than 30 years. Since Yasue and Okumura et al. established the usefulness of intracoronary acetylcholine test for diagnosing patients with coronary spasm in Japan [3-5], many cardiologists employed the acetylcholine testing. Bertrand et al. reported the provoked spasm frequency in 1089 consecutive French Caucasian patients undergoing coronary arteriography in 1982 by the intravenous injection of ergonovine [6], while Nosaka and Nobuyoshi et al. reported the provoked spasm incidence in 3000 consecutive Japanese patients in 1986 via the intravenous injection of eronovine [7]. We already reported the provoked spasm frequency in 685 consecutive Japanese patients by intracoronary acetylcholine testing in 1999 [8]. Recently, Ong et al. disclosed first the provoked spasm incidence in 847 consecutive white Caucasian patients in 2014 by using the intracoronary acetylcholine test [9]. In this article, we investigated the racial difference concerning the provoked coronary artery spasm between Caucasian and Japanese patients in the past four consecutive series undergoing coronary arteriography with the same spasm provocation testing.
Definition of positive spasm and organic stenosis
Bertrand et al. defined positive spasm as more than 75% narrowing and significant stenosis was >50% luminal narrowing, whereas Nosaka et al. assessed positive spasm as subtotal or total obstruction and fixed stenosis was more than 70%. Positive spasm in Ong et al. study was >75% narrowing together with the reproduction of the patient’s symptoms and ischemic ECG shifts. Obstructed coronary artery was >50% narrowing. We assessed positive coronary artery spasm as total or near total occlusion focally and significant organic stenosis as >75% luminal narrowing. All four studies had the slight different definition of positive provoked spasm and significant organic stenosis.
Dose of pharmacologic agents
Maximal intravenous ergonvoine dose was not different between the two studies. Bertrand et al. injected the bolus ergonovine into the femoral vein, whereas Nosaka et al. administered the bolus ergonovine into the ascending aorta, as shown in Table 1. In contrast, maximal intracoronary administration of acetylcholine into the left coronary artery was different between Ong et al. study and our trial. We employed the maximal acetylcholine dose of 100 μg into the left coronary artery, while maximal acetylcholine dose into the left coronary artery was 200 μg in Ong et al. study. However, maximal acetylcholine dose into the right coronary artery was similar on both studies.
| |
Bertrand et al. [6] |
Nosaka et al. [7] |
p value |
Ong et al. [9] |
Sueda et al. [8] |
p value |
| Year |
1982 |
1987 |
|
2014 |
1999 |
|
| Study country (race) |
French (Caucasian) |
Japan (Japanese) |
|
German (Caucasian) |
Japan (Japanese) |
|
| Sample size |
1089 |
3000 |
|
847 |
685 |
|
| male |
- |
1785 (59.5%) |
|
362 (42.7%) |
477 (69.6%) |
<0.001 |
| Age (year) |
- |
55.8 (23-83) |
|
62 ± 12 |
63.2 ± 7.5 |
|
| methodology |
Intravenous ER injection |
Ascending aorta ER injection |
|
Intracoronary ACh over 3 minutes |
Intracoronary ACh for 20 seconds |
|
| Pharmacological dose |
Methergine 0.4 mg |
ER 0.05-0.4 mg |
|
RCA(80 mg) LCA(2/20/100/200 g) |
RCA(20/50/80 mg) LCA(20/50/100 mg) |
|
| Epicardial spasm (pts) |
134 |
383 |
|
283 |
221 |
|
| Epicardial spasm (vessel) |
143 |
466 |
|
378 |
299 |
|
| Ischemic heart disease |
20.1% (128/638) |
22.4% (345/1543) |
ns |
33.4% (283/847) |
45.7% (198/433) |
<0.001 |
| Angina at rest |
37.9% (77/203) |
21% (137/653) |
<0.001 |
32.4% (112/346) |
66.9% (83/124) |
<0.001 |
| Angina on effort |
4.3% (5/117) |
18.3% (42/230) |
<0.001 |
32.4% (72/222) |
33.8% (25/74) |
ns |
| Angina on effort & rest |
13.8% (19/138) |
28.6% (75/262) |
<0.001 |
34.5% (82/238) |
49.0% (25/51) |
ns |
| Myocardial infarction |
15.0% (27/180) |
22.9% (91/398) |
<0.05 |
41.5% (17/41) |
37.6% (44/117) |
ns |
| After PCI |
- |
- |
- |
0% |
31.3% (21/67) |
- |
| Non-ischemic heart disease |
1.3% (6/451) |
2.6% (38/1457) |
ns |
0% |
9.1% (23/252) |
|
| Atypical chest pain |
1.2% (3/248) |
1.2% (8/648) |
ns |
0% |
4.8% (4/83) |
- |
| Valvular heart disease |
2.0% (3/154) |
4.8% (10/208) |
ns |
0% |
12.5% (4/32) |
- |
| Dilated cardiomyopathy |
0% (0/49) |
2.4% (1/41) |
ns |
0% |
3.4% (1/28) |
- |
| Hypertrophic cardiomyopathy |
- |
9.5% (7/74) |
- |
0% |
19.0% (4/21) |
- |
| Other |
- |
3.5% (12/340) |
- |
0% |
11.4% (10/88) |
- |
| |
|
|
|
|
|
- |
| Ischemic heart disease |
58.6% (638/1089) |
51.4% (1543/3000) |
<0.001 |
100% (847/847) |
63.2% (433/685) |
< 0.001 |
| Non-ischemic heart disease |
41.4% (451/1089) |
48.6% (1457/3000) |
<0.001 |
0% |
36.8% (252/685) |
- |
| Lesion > 75% |
15.6% (79/508) |
33.1% (203/613) |
<0.001 |
0% |
35.9% (69/192) |
- |
| Lesion < 75% |
9.5% (55/581) |
7.5% (180/2387) |
ns |
33.4% (283/847) |
30.8% (152/493) |
ns |
| Multiple spasm |
7.5 % (10/134) |
19.3% (74/383) |
<0.001 |
32.5% (92/283) |
29.0% (64/221) |
ns |
| Over all |
12.3% (134/1089) |
12.8% (383/3000) |
ns |
33.4% (282/847) |
32.3% (221/685) |
ns |
(ER: Ergonovine; ACh: Acetylcholine; PCI: Percutaneous Coronary Intervention)
Table 1: Comparisons of provoked spasm frequency among four consecutive studies.
Gender and age
Male were approximately 60% of patients in the Nosaka et al. study, while Bertrand et al. did not write the distributions of sex in detail. In contrast, male were observed in approximately 70% of patients in our study. However, male were just 42.7% of patients in Ong et al. study, as shown in Table 1. There were sex distribution differences in each cohort. Moreover, the mean age was different among three studies. Because age and sex are natural predictors of impaired endothelial function, these differences might be concerned the results of each study [10].
Intravenous ergonovine test (French Caucasian vs. Japanese)
Provoked spasm incidence was not different between French Caucasian and Japanese patients by using the intravenous injection of ergonvoine tests as shown in Table 1 (12.3% vs. 12.8%, ns). There was no difference in patients with ischemic heart disease (20.1% vs. 22.4%, ns) and without ischemic heart disease (1.3% vs. 1.2%, ns). However, in patients with rest angina, provoked spasm frequency was approximately two fold higher in French Caucasian patients than Japanese patients (37.9% vs. 21%, p<0.001), whereas provoked spasm incidence in all patients with ischemic heart disease except rest angina was significantly higher in Japanese patients than French Caucasian populations. Provoked spasm in patients with fixed stenosis in Japanese patients was significantly higher than in French Caucasian populations (33.1% vs. 15.6%, p<0.01), whereas there was no difference in patients without fixed stenosis (7.5% vs. 9.5%, ns). Multiple spasm was three fold higher in Japanese patients than French Caucasian patients (19.3% vs. 7.5%, p<0.001).
Intracoronary acetylcholine test (German Caucasian vs. Japanese)
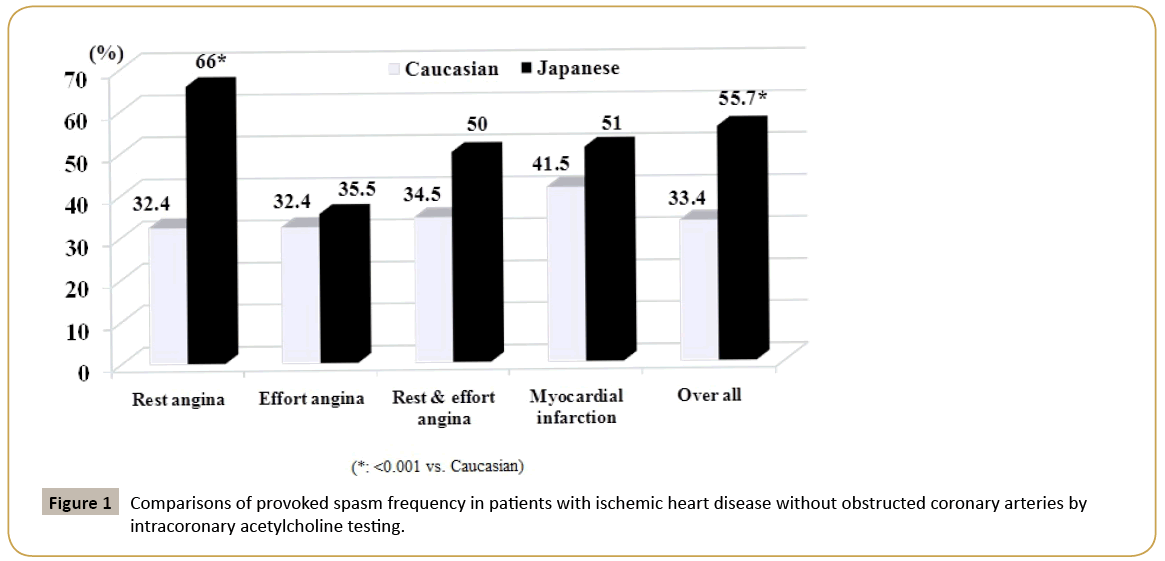
Total provoked spasm frequency was not different between German Caucasian and Japanese populations by using the intracoronary administration of acetylcholine tests as shown in Table 1 (33.4% vs. 32.3%, ns). Patients with rest angina had higher provoked spasms in Japanese patients than in German Caucasian populations (66.9% vs. 32.4%, p<0.001). In contrast, the provoked spasm incidence in patients with ischemic heart disease except rest angina was not different between German Caucasian and Japanese patients. The study populations by Ong et al. were non-obstructive and ischemic heart disease, whereas our study patients included both ischemic and non-ischemic heart disease. In patients with ischemic heart disease, the provoked coronary spasm frequency was higher in Japanese patients than in German Caucasian patients (45.7% vs. 33.4%, p<0.001). Especially, in patients with rest angina, Japanese patients had two fold higher provoked spasm frequency than German Caucasian patients (66.9% vs. 32.4%, p<0.001). Multiple-spasm was not different between the two species (32.5% vs. 29%, ns). As shown in Figure 1, we compared the provoked spasm incidence in patients with non-obstructive and ischemic heart disease between the two studies. Over all provoked spasm rate was one and half fold over in Japanese patients than in German Caucasian patients (55.7% vs. 33.4%, p<0.001). Provoked spasm frequency concerning the rest angina was approximately two fold higher in Japanese patients than in German Caucasian patients, while provoked spasm incidence in patients with effort angina, rest and effort angina, and myocardial infarction was not different between Japanese and German Caucasian patients. The racial difference about provoked coronary spam between German Caucasian and Japanese populations was less than two fold. In Ong et al. study, the angiographical epicardial spasm with and without ischemic ECG changes or chest symptoms was observed in 357 patients (42.1%). Epicardial provoked spasm was significantly higher in Japanese patients than in German Caucasian patients (55.7% vs. 42.1%, p<0.001). Angiographical provoked spasm was approximately 1.3 fold higher in Japanese patients than in German Caucasian patients.
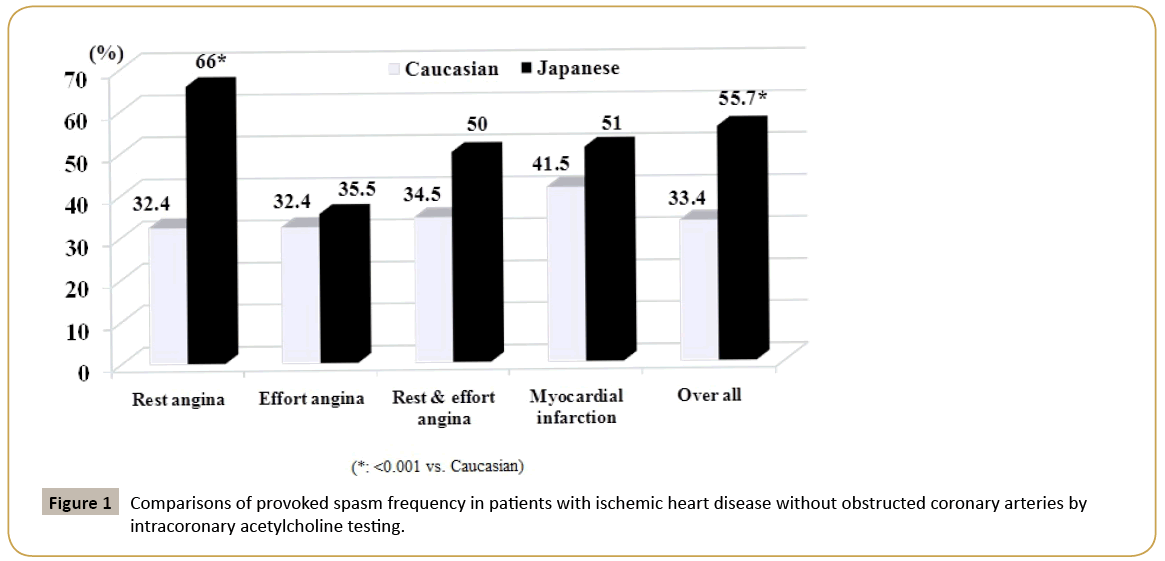
Figure 1: Comparisons of provoked spasm frequency in patients with ischemic heart disease without obstructed coronary arteries by intracoronary acetylcholine testing.
Limitations
This review had several limitations. The first limitation is that all four studies had not the same cardiac disorder distributions irrespective of consecutive series. The second limitation is that these four consecutive studies had the slight different definition of provoked positive spasm. The third limitation is that four studies had not the same age nor sex. The fourth limitation is that maximal acetylcholine dose into the left coronary artery was different between Ong et al. study and our study. If Ong et al. employed the maximal acetylcholine dose of 100 μg into the left coronary artery instead of 200 μg, provoked positive spasm rate might be lower than the reported data. The fifth limitation is that Ong et al. performed the acetylcholine testing on both coronary arteries in only a third study patients (34%), whereas we performed the acetylcholine tests on both coronary arteries in almost all study patients. If Ong et al. performed the acetylcholine testing on both coronary arteries in all patients, positive spasm might be higher than the reported results. In the future, a further prospective worldwide trial in consecutive patients between Caucasian and Japanese populations using the same pharmacologic agents is needed to clarify the real truth of racial difference concerning the coronary spasm.
Conclusions
We may have less racial difference concerning the provoked spasm between Caucasian and Japanese patients when we performed the spasm provocation testing routinely in the cardiac catheterization laboratory.
Acknowledgement
We acknowledge the helpful comments of Professor Yuji Shigematsu, MD, Professor Mareomi Hamada MD, Professor Jitsuo Higaki MD, and Professor Kunio Hiwada MD.
References
- Beltrame JF, Sasayama S, Maseri A (1999)Racial heterogeneity in coronary artery vasomotor reactivity: Differences between Japanese and Caucasian patients. J Am CollCardiol 33: 1442-1452.
- Pritipino C, Beltrame JF, Finocchiaro ML, Hattori R, Fujita M, et al. (2000) Major racial differences in coronary constrictor response between Japanese and Caucasians with recent myocardial infarction. Circulation 101: 1102-1108.
- Yasue H, Horio Y, Nakamura N, Fujii H, Imoto N, et al. (1986) Induction of coronary artery spasm by acetylcholine in patients with variant angina : possible role of the parasympathetic nervous system in the pathogenesis of coronary artery spasm. Circulation 74: 955-963.
- Okumura K, Yasue H, Matsuyama K, Goto K, Miyagi H, et al. (1988) Sensitivity and specificity of intracoronary injection of acetylcholine for the induction of coronary artery spasm. J Am CollCardiol 12: 883-888.
- Okumura K, Yasue H, Horio Y, Takaoka K, Matsuyama K, et al. (1988) Multivessel coronary spasm in patients with variant angina: a study with intracoronary injection of acetylcholine. Circulation 77: 535-542.
- Bertrand ME, LaBlanche JM, Tilmant PY, Thieuleux FA, Delforge MR, et al. (1982) Frequency of provoked coronary arterial spasm in 1089 consecutive patients undergoing coronary arteriography. Circulation 65:1299-1306.
- Nosaka H, Nobuyoshi M (1987) Coronary arterial spasm and symptomatology in ischemic and nonischemic heart disease: study of the erronovine maleate provocation test in 3,000 consecutive patients. J CardiolSuppl12: 35-47.
- Sueda S, Ochi N, Kawada H, Matsuda S, Hayashi Y, et al. (1999) Frequency of provoked coronary vasospasm in patients undergoing coronary arteriography with spasm provocation test of acetylcholine. Am J Cardiol 83: 1186-1190.
- Ong P, Athanasiadis A, Borgulya G, Vokshi I, Bastiaenen R, et al. (2014) Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation 129: 1723-1730.
- Ciccone MM, Bilianou E, Balbarini A, Gesualdo M, Ghiadoni L, et al. (2013) Task force on: ‘Early markers of atherosclerosis: influence of age and sex.J Cardiovasc Med 14: 757-766.