Key words
African-Caribbean mental health, focus
groups, national guideline development, violence
and mental health
Introduction
This paper reports on an approach to the development
of sensitive and clinically appropriate recommendations
for a mental health guideline. The UK’s National Institute
for Health and Clinical Excellence (NICE) commissioned
theNationalCollaborating Centre forNursing
andSupportiveCare(NCC-NSC) toproduceaguideline
on the short-term management of disturbed/violent
behaviour in adult psychiatric inpatients and emergency
departments. The description ‘short-term’ refers
to any violent incidentwithin a 72-hour period. This is
a sensitive topic requiring consideration of the rights
of patients and staff involved in the violent incident.
The importance of this guideline’s topic to African-
Caribbean service users in the UK is widely recognised
by healthcare professionals (Fernando et al, 1998;
Ndegwa, 2000; Sasidharan, 2003). The national census
of inpatients in mental hospitals and facilities in
England and Wales found black Caribbean, black
African and other black groups were more likely (by
33–44%) to be detained under the Mental Health Act
1983 when compared with the average for all inpatients
(Commission for Healthcare Audit and Inspection,
2005). In particular, African-Caribbean men are overrepresented
in mental health services (Pereira et al,
2006), and black men are eight times more likely to be
detained under the Mental Health Act (Audini and
Lelliott, 2002). They are more likely to access care
through a criminal justice agency, involving negative
experiences, coercion and disengagement, and ethnic
explanations for ‘negative pathways to care are not
fully explained by differences in diagnosis, social
circumstances and the involvement of others’ (Morgan
et al, 2005). A number of high-profile inquiries have
raised concerns about the nature and quality of the
treatment and care that African-Caribbean people
receive in mental health services. One example is the
inquiry into the death of David ‘Rocky’ Bennett.
Bennett was an African-Caribbean who died in a
secure unit in 1998 following restraint after he hit
and injured a female nurse (Independent Inquiry into
the Death of David Bennett, 2003).
Forms of evidence used in the
guideline’s development
Guideline methodology continues to develop (National
Institute of Health and Clinical Excellence, www.
nice.org.uk/aboutnice/howwework/developingnice
clinicalguidelines/clinicalguidelinedevelopment
methods/theguidelinesmanual2006/; The Guideline
International Network, www.g-i-n.net/index.cfm?fuse action=membersarea; The AGREE Collaboration (www.agreecollaboration.org/pdf/aitraining.pdf))within the context
of translating evidence into clinical practice. While
research evidence is crucial there is also a need for clinical
expertise, local data and patient experiences and preferences
(Rycroft-Malone, 2004; Jarret, 2004). In the work
reported here, the guideline development group took
into consideration multiple forms of evidence. First
systematic reviews collated all relevant research with no
restrictions on study design. Second, expert reports were
considered, and third, the findings fromthe focus groups
were examined.
Focus groups are used extensively in research, but
less so in guideline development, to collect information
or investigate individual responses to different
situations or policy initiatives, particularly those of a
sensitive nature (Grbich, 1999). They are useful for
encouraging participation from people who are reluctant
to be interviewed individually or who feel they
have nothing to contribute, or to tap into a specific
cultural context (Kitzinger, 1994). Studies show that
focus groups are useful and appropriate when working
with ethnic minority groups (Hennings et al, 1996;
Winslow et al, 2002). This paper presents an account
of the conduct of the focus groups convened to inform
the development of the guideline and the data obtained.
It then moves on to discuss how the guideline was
developed.
Methods
The rationale for conducting the focus groups was to
consult with African-Caribbean service users giving or
receiving care in psychiatric inpatient settings. The key
objectives were to:
• gather data to inform the NICE guideline development
of recommendation formulation
• provide an opportunity for the ‘voice’ of this ethnic
group to be heard in the guideline process.
Data collection
We conducted the three groups over a period of two
months in 2003. We were involved as observers in the
groups and took supplementary notes to clarify and
supplement the taped discussion. There was an additional
independent observer from the Patient Involvement
Unit (PIU), which provides support to the
guideline development process on behalf of NICE for
the involvement of service users in the guideline
process. There were two observers with the facilitator
in each focus group.
Service users
Neither of the authors was African-Caribbean and so
they identified two black and minority ethnic (BME)
advocacy organisations: one had a diverse and transient
population, the other a long-established and marginalised
population. Two nominated facilitators from
these organisations identified African-Caribbean participants
with inpatient experience of mental health
services.We consulted with these facilitators to develop
participant information and a topic guide for the focus
groups based on guideline-specific topics. Written and
oral information was given to the people selected by
the facilitators; informed written consent was obtained
via the nominated facilitators. Participation in the focus
groups was voluntary. The facilitators organised venues
familiar to the participants, and lunch appropriate to
their needs. The BME facilitators conducted one service
user focus group each, with nine and 15 participants,
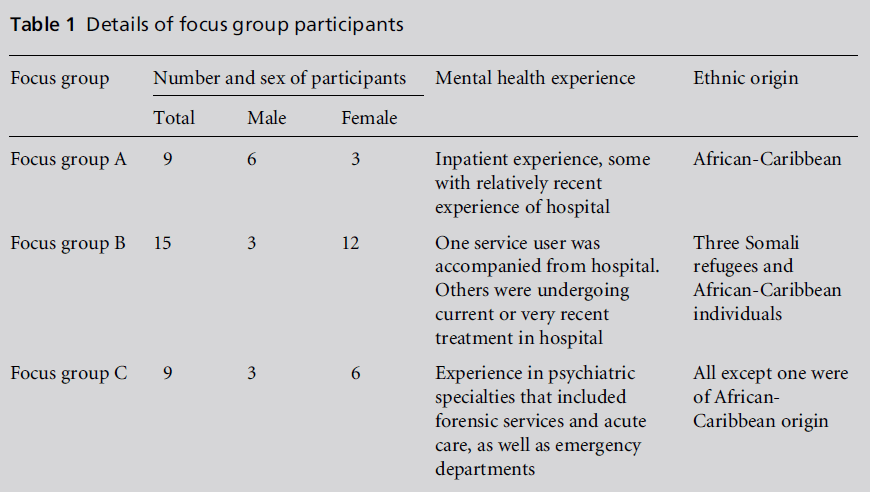
respectively (Table 1). One of the authors and the PIU
member of staff facilitated the staff focus group of nine
participants (Table 1). Participants were informed that
all information received would remain confidential and
anonymous. They were also assured that care and future
treatment would not be affected as a result of their
participation. Participants were also asked to respect
the confidentiality of other participants.
The BME facilitators in both organisations offered
one-on-one discussionswith any participantwho wanted
to further explore issues raised before or after the focus
groups. This was part of the support service provided
by the BME advocacy organisation. The BME facilitators
were experienced advocates within their organisation.
Specific focus group training was not provided
as this was not a research study but a consultation with African-Caribbean mental health service users. Facilitators
were selected from within their organisations
and the groups conducted on their premises.
The NCC-NSC decided formal ethical approval was
not required because the focus groups were not considered
to be a research study. However, ethical issues
such as confidentiality were taken into account. Information
leaflets on topics for discussion, and consent
forms were given to the organisations several months
in advance and the facilitators purposively sampled
participants fitting the inclusion criteria. Participants
and the groups were allocated a personal identifier
(number and a letter) to maintain confidentiality.
Topic areas covered in the discussions included the
ward environment, predictions of violence, interventions,
de-escalation and observation techniques,
restraint and seclusion including training, rapid
tranquillisation, staff and service user relationship,
and use of interventions in emergency departments.
Three or four questions were asked under each topic
area focusing on service users’ experience, observation
of other service users, and their views on staff use of
practices and techniques.
Staff
In order to present views from both sides of the
therapeutic relationship we sought the perspectives
of African-Caribbean staff working in the mental
health sector. We had already established a network
of contacts within the sector via our stakeholder list,
and snowballed for appropriate members for a third
focus group. We sought members of staff who were
African-Caribbean. One participant was white, and
was included because he had extensive experience with African-Caribbean service users. Nine participants
agreed to take part (Table 1). All participants had
some expertise with black service users in psychiatric
inpatient settings or emergency departments. Aims
and objectives of the focus groups with the topics to be
covered were provided to participants before the
group. Their views were requested on the use ofmanagement
of disturbed behaviour interventions, relationships
between staff and service users, the inpatient environment
and its impact on disturbed behaviour. Written
consent was obtained from all participants for the focus
groups to be taped and transcribed and for anonymous
data to be used in a publicly available report.
Table 1 :Details of focus group participants
Data analysis
Thematic content analysis was used to analyse focus
group transcripts. Thematic content analysis is described
as linking together patterns of experience and
behaviour, creating categories of main and subthemes
(high or low order; Aronson, 1994). We used a stageby-
stage method of analysing transcripts from semistructured
open-ended interviews proposed by
Burnard (1991). Participants were given individual
codes, and material was not personally identifiable.
Focus group findings
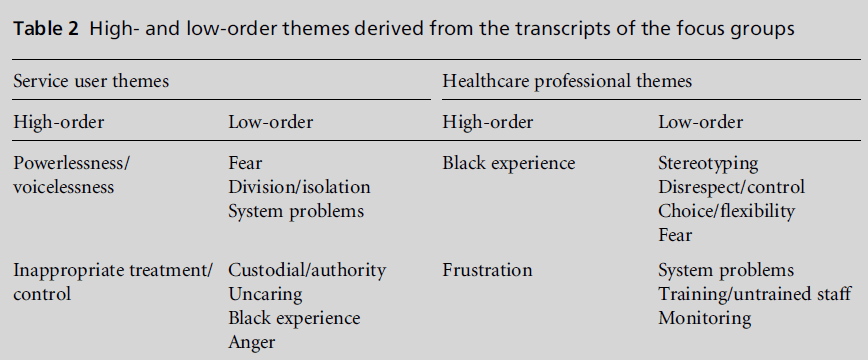
Table 2 summarises the main themes from the three
groups. The service user themes combine the data
from both groups while the staff data were analysed
separately. Themes were generated from verbatim
transcripts of the focus group data. These themes
emerge and are derived from exhaustive categories
taken from the focus group data. A systematic approach
was used (Burnard, 1991) that iteratively clustered the
themes and built up to the main (high-order) themes.
The low-order themes are subthemes to these main themes. Powerlessness/voicelessness was identified as a
main theme because service user participants expressed
an inability to influence their care or to have their
needs met.
‘When you got to staff members and say ‘‘I’m feeling a bit
worse’’, it’s ‘‘Go and sit down’’, ‘‘Go away’’, they don’t
want to hear when you’re actually acknowledging that you
are actually feeling worse, they’re not prepared to hear.’
(participant 2, group A)
‘The system is failing us.’ (participant 5, group A)
Service user participants also expressed experiencing
racial stereotyping and the inappropriate use of disturbed
behaviour management techniques – hence the
main theme of inappropriate treatment/control.
‘On the ward, African-Caribbean people, we’re seen as a
lot more aggressive rather than this is how we culturally
are, so we’re treated this way.’ (participant 1, group A)
‘I was restrained by a particular nurse who had a technique
where he put my arm behind my back and crunched
my fingers together until the knuckles swapped over and
wrench it in a different direction so it would swell up like
when you do boxing and I couldn’t usemy fingers at all ... I
plait my little girl’s hair, so I wasn’t able to plait her hair
for her and it was making me more upset.’ (participant 7,
group A)
The healthcare professional main themes of black
experience also concurred with the service users’ experiences,
particularly fear.
‘One interesting dynamic is that one of staff fear the
patients more than the patients fear each other.’ (participant
26, group C)
They particularly expressed frustration with the systems:
‘We know from whatever little data is available that black
patients are more likely to be restrained, secluded,
medicated and so on, so that the whole process of
heavy-handed management is an issue for black patients.’
(participant 31, group C) These findings are consistent with the report of
the Sainsbury Centre for Mental Health (2002), which
included 31 focus groups with African-Caribbean
mental health service users. Key themes from this
report include circles of fear, inhumane and unhelpful
care, problematic care pathways, and conflict between
professionals and service users not being addressed.
Table 2 :High- and low-order themes derived from the transcripts of the focus groups.
Limitations
The guideline development process was constrained
by the guideline timelines. Time for preparation and
data analysis of the focus groups was limited, and the
emphasis was on using our time effectively to achieve
our aim. Much of the material gathered in the focus
groups did relate specifically to the experience of BME
service users but, as there was no comparison group of
non-black service users, it could be suggested that
some of the views expressed could relate to all mental
health service users irrespective of their ethnicity.
It is acknowledged that the focus group data represent
a small group of individual views that are not
directly verifiable. However, they are consistent with
other focus group data of African-Caribbean mental
health service user experiences undertaken by the
Sainsbury Centre for Mental Health (2002). If the focus
group material had been inconsistent with other findings,
further data collection would have been required.
Development of recommendations
The recommendations were developed to improve the
overall experience of care by shifting the focus away
from custodial and control techniques towards an
approach that responded to the needs of the individual
service user. The development process endeavoured to
be as transparent as possible.
The guideline development group was composed of
12 expert clinicians representing medicine (4), nursing
(2), pharmacy (1), allied healthcare professionals
(1), emergency medicine (1), physical management
training (1), economics (1), legal (1), and two service
users. These service users were not from a BME group.
Service user and professional BME representatives were
specifically co-opted to increase representation; they
were not involved in the focus groups.
The guideline development group drew on all three
sources of information: systematic reviews, expert reviews
and the focus group data. A modified nominal
consensus technique was used for recommendation
development, amendment and ratification (Trickey,
1998; Rycroft-Malone and Duff, 2000). This technique
has been used in the development of similar guidelines
with a variable research evidence base that included
other forms of evidence, for example patients’ experiences
(Trickey, 1998; Rycroft-Malone, 2004). The guideline was peer reviewed and went through two
stakeholder consultation processes.
An independent external facilitator chaired the
consensus meetings. This person was familiar with
guideline development, but not experienced with the
particular guideline topic under development. The
consensus process was facilitated by computerised
voting consoles, which assured anonymity and allowed
percentages to be quickly calculated. Consensus was
set at 80% unless a significant number within the
group all voted against a recommendation. For example,
if all the psychiatrists had voted against a recommendation,
even though 80% agreement was achieved,
consensus would not have been reached. No abstentions
were allowed. The computerised voting system
permitted an inclusive, constructive discussion before
the vote. It included microphones that required switching
on and off, and members wishing to be heard were
allocated in turn to speak on the screen. The wording
and amendment of the recommendations were facilitated
by this process. Changes were viewed as they
were made, allowing an iterative refinement. This helped
to ensure that all members of the guideline development
group, including two service users, were able to
contribute equally.
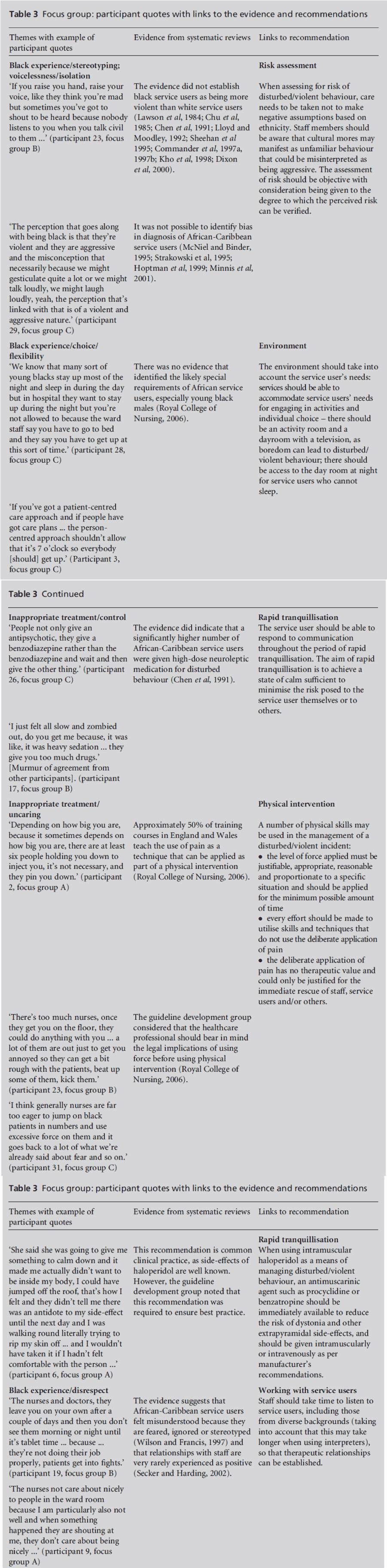
Table 3 shows examples of the links established
between the systematic review evidence, extracts from
the focus groups, and recommendations made. Themes
from the focus groups echo the literature which suggests
an imbalance of African-Caribbean representation
(Commission for Healthcare Audit and Inspection,
2005), in mental health service environments, and that
African-Caribbean individuals experience conflict and
fear (Sainsbury Centre for Mental Health, 2002).
All the evidence obtained during the guideline
development process was taken collectively into account
to generate recommendations. The different
information sources gathered for this guideline were
not weighted. The guideline development group gave
due consideration to all the information presented to
them. The information was presented in a written
review or orally via expert representation. The purpose
of Table 3 is to illustrate and provide a structure to
show that concerns raised in the focus groups fed into
guideline recommendations.
The guideline development deliberations on recommendations
involved much debate on the management
of the physical intervention (restraint) and
the use of medication (rapid tranquillisation). Focus
group themes about inappropriate treatment/control,
uncaring and powerlessness referred to participants’
experiences of receiving medication and physical
interventions during disturbed or violent episodes.
In particular they expressed concern about the overuse
of the techniques, a lack of alternatives, and a readiness
by staff to use medications, physical intervention
(restraint) and seclusion (isolation).
Table 3 :Focus group: participant quotes with links to the evidence and recommendations.
‘It’s about controlling people ... it’s keeping them in a
zombiefied state so that their job is made easier and then
they feel powerful.’ (participant 1, group A)
‘I just think that there should be something where they
constantly train people in restraint ... people tend to get
hurt, the patient tends to get hurt.’ (participant 6,
group A)
It was also expressed by participants that management
of violence techniques were particularly overused on
black people.
‘There was a women that was constantly being picked on
with regards to restraint and she was a Jamaican.’ (participant
7, group A)
‘Most of the time, if you’re black, you’re going to get bent
and twisted up and carried into seclusion.’ (participant
23, group B)
As a result, the guideline development group used this
opportunity to address racial and other issues of
equality. Furthermore, an emphasis on staff and service
users’ safety was also incorporated into guideline
recommendations. The recommendations emphasise
continuous risk assessment and the ongoing use of deescalation
techniques in the care pathway for managing
short-term disturbed/violent behaviour. Table 3 identifies specific recommendations in relation to
focus group concerns. There is also an overarching
recommendation to ensure that responsibility for racial
and other equality issues is addressed at the organisational
level. Additionally consultation with local
BME groups is promoted (Royal College of Nursing,
2006).
Discussion
Focus groups as a qualitative method to gain patient
opinion in health research have become increasingly
popular (Webb and Kevern, 2001; Barbour, 2005).
However, focus groups often do not report participant
interaction and the group dynamic is an important
part of the method (Webb and Kevern, 2001). The
limitations of the guideline timelines did not allow a
fuller exploration. Consensus of opinion in the group
is an emergent property, not an individual participant
opinion, and although inference can be drawn this
does not indicate the strength of an opinion (Barbour,
2005). Caution must also be used against attempting
to generalise focus group findings (Sim, 1998). We
used a multi-method approach within the guideline
methodology, and sought the perceptions of care of a
specific population. The overall negative opinion of
care expressed by the service users in the focus groups
could indicate the group selecting negative rather than
positive experiences to fit in with an emergent group
trend. Data analysis needs to be more thorough and
effective, and inclusive of group interaction and dynamics
to determine whether this might actually be
the case (Barbour, 2005). An example is shown in
Table 3 under inappropriate treatment and control.
Members of the group responded to one individual by
murmuring agreement. This happened on a number
of occasions, and a better description of the group
processes could have enabled this information to be
used more effectively in illustrating one aspect of focus
group experience, which is the recognition of experience
between group members.
Focus group studies need to be congruent with the
qualitative tradition and context appropriate (Hughes
and Dumont, 1993). The guideline consultation focus
groups were conducted as part of the guideline development
methodology and had specific aims and
objectives. The task of a guideline is to ensure quality
clinical practice based on evidence at best, or at the
least use of formal consensus techniques. The literature
did not provide information or evidence on the
more subtle and sensitive issues of racial stereotyping,
but the focus group findings channelled information
into the guideline development process to fill the gap.
The importance of this work illustrates the requirement
for guideline development to be flexible and
responsive, to meet the clinical need for best practice
in the absence of good-quality and relevant evidence.
It also needs to avoid tokenism in gaining the service
user perspective.
In addition, this experience of conducting focus
groups as part of guidelinemethodology has highlighted
the importance of establishing transparent methods
to report sources of evidence, their context and their
synthesis.Wehave clearly stated that there was no formal weighting of evidence and that consensus methods
were used to develop guideline recommendations. A
refined conceptual framework for consideration of
evidence and context to be applied to the development
of health policy recommendations acknowledges the
role of agreement-based consensus methods alongside
rule-based grading schemes (Dobrow et al, 2006). The
sensitivity given to the context, as in this instance, of
health policy will promote the improvement ofmethods
for utilising evidence in development of health policy
(Dobrow et al, 2006).
Validity and consistency
Respondent validation was conducted via the black
advocacy organisations; no significant changes were
required and participants seemed satisfied with the
draft report. The analysis was not conducted by an
independent assessor. However, as the focus group
observers did not attend all the groups they did analyse
the taped data of all three groups individually. The two
guideline developers and the PIU representative discussed
the key findings and agreed themes together.
This was done through a process of presenting individual
themes and collectively agreeing common
themes. The findings were consistent with other reports
such as Breaking Circles of Fear, which conducted
31 focus groups with African-Caribbean service
users (Sainsbury Centre for Mental Health, 2002). This
report, the Independent Inquiry into the Death of
David Bennett (2003), and the focus group material
provided an overall picture of an untherapeutic environment
that is threatening and fearful for both staff
and service users. It also suggests that there is a
perpetuation of cycles of violence leading to a culture
of violence on some wards.
Conclusion
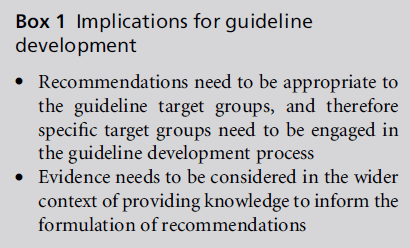
This paper’s key messages and the implications for
guideline development (Box 1) are the value of focus
groups as part of a strategy in guideline development
to engage the voice of African-Caribbean mental health
service users to inform the generation of clinically
sensitive recommendations. The primary focus throughout
the development process was on the staff and
patient relationship as crucial to the short-term management
of disturbed/violent behaviour. Erosion of
the therapeutic relationship was a principal concern.
Focus groups informed the development of recommendations
to address staff behaviour and attitudes
by ensuring that the African-Caribbean service users’
voices made a direct contribution to the process. The
purpose of this paper has been to show the rationale
for using focus groups in guideline development and
the impact on aiding recommendation generation. We suggest an evaluation of focus group work across
guidelines to ascertain the advantage of using focus
groups, as an additional form of evidence to aid
guideline development.
"
ACKNOWLEDGEMENTS
We would like to thank Joan Field-Thorn, BlackOrchid,
Bristol and Pauline Abbott-Butler, Footprints UK,
London for facilitating the focus groups on our behalf
of the NCC-NSC. We would also to acknowledge and
thank Jane Cowl, Patient Involvement Unit, NICE for
her collaboration with the authors on this project. The
authors would also like to thank Dr Jo Rycroft-Malone
for comments on drafts of the paper.
The recommendations were generated by consensus
techniques with the NICE Guideline Development
Group listed below:
William Bingley, University of Central Lancashire
Tony Bleetman, British Association for Accident &
Emergency Medicine
Frank Corr, Royal College of Nursing
Jane Cronin-Davis, Clinical Effectiveness Forum for
Allied Health Professionals
Donna-Maria Fraher, Independent Consultant
Phil Hardy, Institute of Conflict Management
Sophie Jones, National Voices Forum
Kevin Gournay, Institute of Psychiatry (Chair)
Edwin Gwenzi, Institute of Psychiatry
Sue Johnston, Royal College of Psychiatrists
Stephen Pereira, National Association of Psychiatric
Intensive Care Units
Peter Pratt, Royal Pharmaceutical Society of Great
Britain
Rick Tucker, Nursing & Midwifery Council
Aki Tsuchiya, SchAAR, Health Economist
References
- Aronson J (1994) A pragmatic view of thematic analysis.The Qualitative Report; 2(1) www.nova.edu/sss/QR/Back Issues/QR2-1/aronson.html
- Audini B and Lelliot P (2002) Age, gender and ethnicity ofthose detained under Part II of the Mental Health Act1983. British Journal of Psychiatry 180:222ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Barbour RS (2005) Making sense of focus groups. MedicalEducation 39:742ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â50.
- Burnard P (1991) A method of analysing interview transcriptsin qualitative research. Nurse Education Today11:461ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Chen EY, HarrisonGandStanden PJ (1991) Management offirst episode psychotic illness in Afro-Caribbean patients.British Journal of Psychiatry 158:517ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â22.
- Chu CC, Sallach HS, Zakeria S and Klein HE (1985)Differences in psychopathology between black and whiteschizophrenics. International Journal of Social Psychiatry31:252ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Commander MJ, Cochrane R, Sashidharan SP, Akilu Fand Wildsmith E (1997a) Ethnicity and Mental HealthService Provision. Birmingham: Academic Unit, NorthernBirmingham Mental Health Trust.
- Commander MJ, Cochrane R, Sashidharan SP, Akilu Fand Wildsmith E (1997b) Ethnicity and Mental HealthService Provision. Academic Unit, Northern Birmingham:Birmingham Mental Health Trust.
- Commission for Healthcare Audit and Inspection (2005)Count Me In: results of the national census of inpatients inmental health hospitals and facilities in England and Wales.London: Commission for Healthcare Audit and Inspection.
- Dixon M, Oyebode F and Brannigan C (2000) Formaljustifications for compulsory psychiatric detention. Medicine,Science and Law 40:319ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â26.
- Dobrow MJ, Goel V, Lemieux-Charles L and Black NA(2006) The impact of context on evidence utilization: aframework for expert groups developing health policyrecommendations. Social Science and Medicine 63:1811ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â24.
- Fern EF (2001) Advanced Focus Group Research. London:Sage Publications, p. 175.
- Fernando S, Ndegwa D and Wilson M (1998) ForensicPsychiatry, Race and Culture. London: Routledge.
- Fox DJ (1982) Fundamentals of Research in Nursing (4e).Newark, NJ: Appleton-Century-Crofts.
- Glaser BG and Strauss AL (1967) The Discovery of GroundedTheory. New York: Aldine.
- Grbich C (1999) Qualitative Research in Health. London:Sage Publications.
- Hennings J, Williams J and Hague BN (1996) Exploring thehealth needs of Bangladeshi women: a case in usingqualitative research methods. Health Education Journal55:11ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â23.
- Hoptman MJ, Yates, KF, Patalinjug MB, Wack RC andConvit A (1999) Clinical prediction of assaultive behavior among male psychiatric patients at a maximumsecurityforensic facility. Psychiatric Services 50:1461ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Hughes D and DuMont K (1993) Using focus groups tofacilitate culturally anchored research. American Journalof Community Psychology 21:775ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â805.
- Independent Inquiry into the Death of David Bennett (2003)An Independent Inquiry set up under HSG(94)27.Cambridge: Norfolk, Suffolk, Cambridgeshire StrategicHealth Authority.
- Jarret L, Patient Involvement Unit (2004) A Report on aStudy to Evaluate Patient/Carer Membership of the firstNICE Guideline Development Groups. London: NationalInstitute for Clinical Excellence.
- Kho K, Sensky T, Mortimer A and Corcos C (1998) Prospectivestudy into factors associated with aggressiveincidents in psychiatric acute admission wards. BritishJournal of Psychiatry 172:38ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â43.
- Kitzinger J (1994) The methodology of focus groups: theimportance of interaction between participants. Sociologyof Health and Illness 16:103ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â21.
- Lawson WB, Yesavage MD and Werner PD (1984) Race,violence and psychopathology. Journal of Clinical Psychiatry45:294ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Lloyd K and Moodley P (1992) Psychotropic medicationand ethnicity: an inpatient survey. Social Psychiatry andPsychiatric Epidemiology 27:95ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â101.
- McNiel DE and Binder RL (1995) Correlates of accuracy inthe assessment of psychiatric inpatientsÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ risk of violence.American Journal of Psychiatry 152:901ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Minnis H, McMillan A, GilliesMand Smith S (2001) Racialstereotyping: survey of psychiatrists in the United Kingdom.BMJ 323:905ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Morgan C, Mallett R, HutchinsonGet al (2005) Pathways tocare and ethnicity. 2. Source of referral and help-seeking.British Journal of Psychiatry 186:290ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Ndegwa D (2000) Social Division and Difference: black andethnic minorities. London: NHS National Programme onForensic Mental Health Research and Development.
- Pereira S, Dawson P and Sarsam M (2006) The nationalsurvey of PICU and low secure services: 1. Patient characteristics.Journal of Psychiatric Intensive Care 2:7ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â12.
- Royal College of Nursing (2006) Violence: the short-termmanagement of disturbed/violent behaviour in in-patientpsychiatric settings and emergency departments. London:Royal College of Nursing. www.rcn.org.uk/development/practice/clinicalguidelines/violence
- Rycroft Malone J (2004) Formal consensus techniques: thedevelopment of a national clinical guideline. Quality inHealth Care 10:238ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â44.
- Rycroft Malone J and Duff L (2000) Developing clinicalguidelines: issues and challenges. Journal of Tissue Viability10:144ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9, 152ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â3.
- Sainsbury Centre for Mental Health Centre (2002) Breakingthe Circles of Fear ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â a Review of the Relationship BetweenMental Health Services and African and CaribbeanCommunities. London: The Sainsbury Centre for MentalHealth.
- Sasidharan SP (2003) Inside OutsideÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âImproving MentalHealth Services for Black and Minority Ethnic Communitiesin England. London: Department of Health.
- Secker J and Harding C (2002) African and AfricanCaribbean usersÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ perceptions of inpatient services. Journalof Psychiatric and Mental Health Nursing 9:161ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Sheehan JD, Hardie T and Watson JP (1995) Social deprivation,ethnicity and violent incidents on acute psychiatricwards. Psychiatric Bulletin 19:597ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Sim J (1998) Collecting and analyzing qualitative data: issuesraised by the focus group. Journal of Advanced Nursing28:345ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â52.
- Strakowski SM, Lonczak HS, SaxKWet al (1995) The effectsof race on diagnosis and disposition from a psychiatricemergency service. Journal of Clinical Psychiatry 56:101ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Trickey H, Harvey L, Wilcock G and Sharp D(1998) Formalconsensus and consultation: a qualitative method fordevelopment of a guideline for dementia. Quality in HealthCare 7:192ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Webb C and Kevern J (2001) Focus groups as a researchmethod: a critique of some aspects of their use in nursingresearch. Journal of Advanced Nursing 33:798ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â805.
- Wilson M and Francis J (1997) Raised Voices ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â African-Caribbean and African UsersÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ Views and Experiences ofMental Health Services in England and Wales. London:MIND Publication.
- Winslow WW, Honein G and Eluzubier MA (2002) SeekingEmirati womenÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s voices: the use of focus groups with anArab population. Qualitative Health Research 12:566ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â75.