Agar N1*, Gremeau AS1, Bonnin M1 and Vendittelli F1,2
1Pôle Femme et Enfant, CHU Clermont-Ferrand, Hôpital Estaing, 1 place Lucie Aubrac, 63003 Clermont-Ferrand cedex1, France
2Clermont Universite, Universite d'Auvergne, EA 4681, PEPRADE (Perinatalite, grossesse, Environment, Pratiques medicales et Development), 63001 Clermont-Ferrand cedex 1, France
*Corresponding Author:
Nicolas Agar
Centre Hospitalo-Universitaire de Clermont-Ferrand, Site Estaing, Pôle Femme et Enfant, 1 Place Lucie Aubrac, France
Tel: +33473755039
E-mail: nagar@chu-clermontferrand.fr
Received date: February 10, 2016 Accepted date: March 16, 2016 Published date: March 18, 2016
Precis
We report the cases of three patients, who presented with acute pelvic dysfunction syndrome postpartum. All received local infiltration, which had rapid and long-lasting effects, that was successfully combined with analgesia and pelvic belts.
Keywords
Symphysis pubis dysfunction; Post-partum; Pregnancy; Local analgesic infiltration
Introduction
Symphysis pubis dysfunction (SDP), which was recognized by Hippocrates, was first described in 1870 by Snelling. The pubic symphysis can normally widen 2 or 3 mm but during pregnancy the gap can be up to 10 mm. SDP is defined on the basis of mechanical pelvic pain associated with a widening of the symphysis of more than 10 mm.
Studies variously estimate that SDP affects 1 in 300 to 1 in 30000 pregnant women [1]. The clinical picture is characterized by sudden or insidious pelvic pain during the peri- or postpartum period. The pain is located on the pubis and is exacerbated on palpation of the symphysis and/or trochanter. Functional troubles include pubic pain aggravated by walking or standing, and disorders such as a waddling gait. Diagnosis is confirmed by anteroposterior pelvic x-ray. Diastasis greater than 10 mm is associated with partial or total rupture of the pubic ligament. Lesions greater than 4 cm are unstable and require surgical repair. However, diastasis size is not correlated with the severity of symptoms [2].
Treatment of a stable lesion is conservative and combines rest, oral analgesia, pelvic contention with a maternity belt and, when indicated, a course of physiotherapy. However, in some cases this management is not effective, especially in the event of acute pain. In 2006 our team reported the beneficial results achieved with a single pubic infiltration [3]. We will present the cases of three other patients who received this treatment with immediate relief of pain and excellent longterm evolution.
Cases
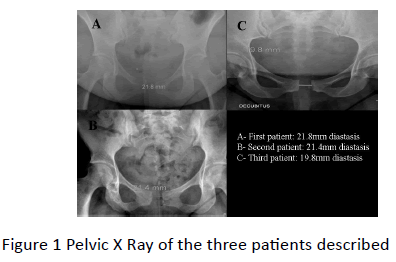
All three patients had hyperalgesic SDP diagnosed postpartum, which was associated with functional impotence and treated by local infiltration. All had delivered vaginally in the supine position, under epidural analgesia. X-rays of these patients were presented in Figure 1.
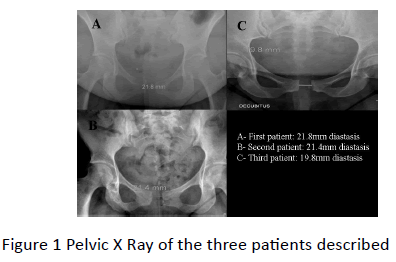
Figure 1 Pelvic X Ray of the three patients described
The first patient was a 33-year-old, G4P1 (one vacuum vaginal birth of 3500 g infant for ineffective expulsive efforts and two early miscarriages) and had a history of dorsal pain due to L5-S1 and L4-L5 discopathy, obesity (BMI = 32) and laparoscopic ovarian cystectomy for endometrioma. She was admitted to the high-risk pregnancy unit at 37 + 2 weeks of gestation for left leg erysipelas. Four days later she complained of vulvar swelling, pelvic pain and inability to walk. Neurological examination by a specialist was normal. In view of her symptoms, labor was induced by oxytocic perfusion, after epidural analgesia at 38 + 1 weeks of gestation. She gave spontaneous vaginal birth to a 3700 g girl, with complete delivery of the placenta. On the second post-partum day, she still complained of pelvic pain and difficulty in walking. X-ray revealed a 21.8 mm diastasis (which was probably present before birth). Local pubic infiltration was performed on day 3, after the failure of medical treatment with combined lidocaine 1% and methylprednisolone. On day 5, the patient showed clear improvement, was able to walk, and to wash and bathe unaided. She was discharged on day 6. At the post-partum consultation 6 weeks later she reported no recurrence of pain or other symptoms.
The second patient was 27 years old, G3P1 (normal vaginal delivery of 3860 g infant and an early miscarriage) and had a history of hypothyroidism and obesity (BMI = 35). At 33 + 4 weeks of gestation, she spontaneously went into labor, after an intrauterine death due to an undetected polymalformative syndrome. Delivery of a 3255 g infant was difficult and vacuum-assisted with reduction of shoulder dystocia. She had post-partum bleeding and required artificial placenta delivery, dinoprostone and uterine embolization. She developed an acute lung edema in the intensive care unit. On post-partum day 5, she complained of pubic pain, and pain during thigh flexion and on walking. SDP was diagnosed after pelvic X-ray showed 21.4 mm diastasis. Conservative treatment was unsuccessful and so she was given local infiltration as described further in the discussion, which had immediate and long-term effects.
The third patient was 31 years old, G3P1 (one vaginal birth at 41 WG of 3500 g infant and an ectopic pregnancy managed by laparoscopic salpingectomy). She presented with a twin dichorionic diamnotic pregnancy after in vitro fertilization. She delivered at 36 + 1 weeks of gestation after prostaglandin labor induction for amniotic sac rupture. The first infant (2870 g) was born without difficulty (cephalic presentation), but the second (2980 g) required Lovset and Bracht maneuvers for breech presentation. On day 2 postpartum, the patient quickly complained of pain and a waddling walk. She had elective pain during symphysis palpation. Pelvic X-ray showed diastasis of 19.8 mm and SDP was diagnosed. On day 3, she received the same local infiltration. On day 5 she had totally recovered and returned home.
All medical managements involved oral analgesia, such as paracetamol or anti-inflammatory drugs, for a few days, and contention with a pelvic belt, which alleviates pain by significantly reducing sacroiliac joint mobility. At the 6-8 weeks post natal visit, none of the women reported a recurrence of their symptoms.
The first and the second patients are lost to follow-up. The third one gave birth 3 years later without any recurrence of SDP.
Comment
During pregnancy, there are physiological changes in pelvic geography and in the mobility of the sacroiliac joints due to hormones such as progesterone and relaxin, which cause general laxity in the soft tissues. The effect is to facilitate delivery by increasing the sagittal diameter of the pelvis. Enlargement of the symphysis is tolerated up to 9 mm; if it is any greater SDP should be considered as the cause. SDP is a condition that is too often under-recognized during pregnancy and postpartum and is subsequently poorly managed. It is responsible for significant morbidity, which can persist several years after delivery. Certain risks factors have been identified [4]: rapid labor, especially second phase, rapid descent of the fetus, pelvic anomalies (such as dysplasia, osteomalacia or rickets), macrosomia, multiparity, twins, shoulder dystocia and obstetrical maneuvers. Some of these factors were observed in our cases, as was obesity or shoulder dystocia which has also been frequently reported [4,5].
Clinical examination is essential for diagnosis and can be complemented by pelvic X-ray, which is an easy and reproducible technique. An alternative, especially earlier in pregnancy, is ultrasound scanning, with linear probes from 5-7.5 MHz [6]. Typical symptoms include pubic pain with inguinal radiation, trouble in walking, symphyseal edemas, and sometimes, palpation of a real symphyseal space. The intensity of the pain is variable but is always exacerbated by movement involving the symphyseal joint such as standing, walking, climbing stairs or heavy lifting. Diastasis greater than 4 cm is generally indicative of a lesion that is unstable and which requires surgical treatment.
Medical treatment for mild to moderate SDP includes rest, painkillers such as paracetamol, anti-inflammatory drugs and sometimes codeine, physiotherapy, osteopathy, pelvic belt and local infiltration [4]. When diastasis is larger than 4 cm surgical treatment with fixation can, according to some authors, allow earlier ambulation and hospital discharge. Anti-clotting treatment with heparin is necessary in the event of prolonged immobilization. A rare case has been reported of recourse to epidural analgesia during the second trimester of a twin pregnancy in a woman with severe SDP and total impotence [7]. The main problem is the management of acute pain, especially when it is resistant to oral therapy (opioids) and results in a total inability to walk. In 2006, our team described the first use of a single local infiltration, which was highly successful [3].
The protocol we used for local infiltration was described by Bonnin et al. [3] in 2006 and must be performed aseptically in an operating room. Infiltration consists of 5 ml of lidocaine 1% and 40 mg of methylprednisolone to potentiate the analgesic effect. In the case report of Bonnin et al. infiltration with lidocaine alone was weakly effective but a second injection in combination with corticosteroids was successful. A 24G needle of 50 mm was used and inserted perpendicularly to the skin, directly toward the center of the pubic symphysis. The needle is stopped by the fibroelastic cartilage and must then be withdrawn slightly out of the joint so that the injection can be performed without resistance. Caution should be taken before injection to ensure that the aspiration test is negative and that there is no paresthesia. The advantages of local infiltration are its ease, speed and long-term effectiveness. The drawbacks are the need for an anaesthesiologist trained in local anaesthesia and the “potential risk” of iatrogenic infection and allergic reaction. This treatment is contraindicated if the patient is hypersensitive to any component.
Documented results report that functional recovery is achieved in 6-8 weeks to 6-8 months [4]. The long term outcome is generally excellent. It was recently shown that almost half of women with persistent post-partum pelvic pain were able to do physical activity 6 months after giving birth. Regular physical activity before pregnancy does not, however, affect the risk of chronic pain in the post-partum period [8].
Chronic pelvic pain is the main risk of SDP if the condition is not properly treated. Idress et al. recently reported the case of a 39-year-old woman with chronic neuropathic pain that persisted 6 years after delivery. Her symptoms improved only after the installation of a spinal cord stimulator [9]. This confirms the importance of an early diagnosis and immediate, appropriate treatment. Rheumatologists and physiotherapists frequently encounter post-partum pubic pain but management is often inadequate. In combination with a suitable analgesic treatment, the patient can be offered osteopathy, physiotherapy (massage and stretching), electrotherapy and cryotherapy [10].
The management of SPD is multidisciplinary and should involve obstetricians, anaesthetists and physiotherapists. In patients with a severe form, local infiltration is a simple and effective treatment that can be successfully combined with appropriate painkillers and pelvic belts.
References
- Yoo JJ, Ha YC, Lee YK, Hong JS, Kang B-J, et al. (2014) Incidence and risk factors of symptomatic peripartum diastasis of pubic symphysis. J Korean Med Sci29:281-286.
- Snow RE, Neubert AG (1997) Peripartum pubic symphysis separation: a case series and review of the literature. Obstet Gynecol Surv52:438-443.
- Bonnin M, Bolandard F, Storme B, Sibaud F, Rabishong B (2006) Pelvic pain by acute symphysis pubis separation after vaginal delivery. Ann FrAnesthèsieRèanimation25:644-647.
- Seth S, Das B, Salhan S (2003) A severe case of pubic symphysis diastasis in pregnancy. Eur J Obstet Gynecol Reprod Biol 106:230-232.
- Laadioui M, Slimani W, Jayi S, Alaoui FF, Bouguern H, et al. (2014) Symphysis disjunction after an obstructed viginal delivery: report of a case. Pan Afr Med J17:33.
- Scriven MW, Jones DA, McKnight L (1995) The importance of pubic pain following childbirth: a clinical and ultrasonographic study of diastasis of the pubic symphysis. J R Soc Med 88:28-30.
- Scicluna JK, Alderson JD, Webster VJ, Whiting P (2004) Epidural analgesia for acute symphysis pubis dysfunction in the second trimester. Int J Obstet Anesth13:50-52.
- Mogren IM (2008) Physical activity and persistent low back pain and pelvic pain post partum. BMC Public Health8:417.
- Idrees A (2012) Management of chronic symphysis pubis pain following child birth with spinal cord stimulator. JPMA J Pak Med Assoc62:71-73.
- Fry D, Hay-Smith J, Hough J, McIntosh J, Polden M, et al. (1997) National clinical guidelines for the care of women with symphysis pubis dysfunction. Association of Chartered Physiotherapists in Women’s Health. Midwives Off J R Coll Midwives110:172-173.