- (2011) Volume 12, Issue 4
Jia Li1, John Ng2, John Allendorf3, Muhammad W Saif4
1VA Connecticut Healthcare System, Yale School of Medicine, Yale Cancer Center. West Haven, CT, USA
2Department of Radiation Oncology
3Division of Gastrointestinal/Endocrine Surgery
4Division of Hematology and Oncology; Columbia University College of Physicians and Surgeons. New York, NY, USA
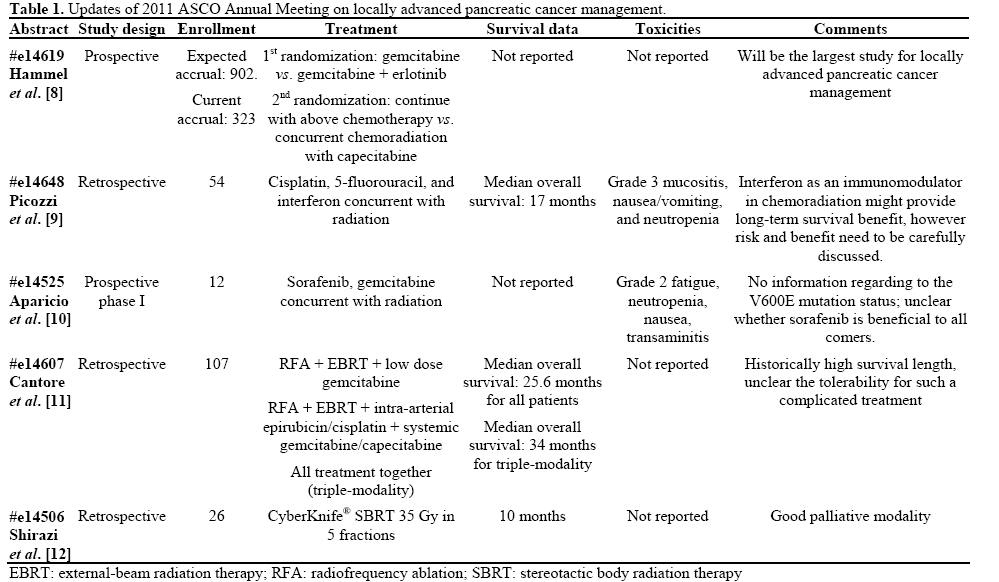
Pancreatic cancer, as the 4th leading cause of cancer death in the U.S., remains a challenging disease for all oncologists. Less than 20% of all cases could be potentially cured by surgical resection, while the majority of cases are deemed either unresectable or metastatic upon diagnosis. In this year’s American Society of Clinical Oncology (ASCO) Annual Meeting, several studies were presented with novel approaches towards treating locally advanced pancreatic cancer. The LAP-07 study, a large phase III study with two separate randomizations, updated their accrual status, but with no interim data yet reported (Abstract #e14619). A single institutional review study reported its promising results on the incorporation of interferon to chemoradiation, but the toxicities could be concerning (Abstract #e14648). Abstract #e14607 demonstrated promising survival data from a tri-modality approach incorporating local and systemic chemotherapy concurrent with external beam radiation as well as radiofrequency ablation. The tolerability of sorafenib in locally advanced pancreatic cancer was shown in a small phase I study (Abstract #e14525). CyberKnife® stereotactic body radiation therapy was investigated as a modality for local palliation (Abstract #e14506). More effective therapeutic agents and approaches are still needed in this difficult disease. This highlight article will focus on the management of locally advanced pancreatic cancer.
Combined Modality Therapy; erlotinib; Fluorouracil; gemcitabine; Pancreatic Neoplasms; Radiation; Radiosurgery; sorafenib
Abbreviations
ASCO: American Society of Clinical Oncology; EBRT: external-beam radiation therapy; ECOG: Eastern Cooperative Oncology Group; FFCD-SFRO: Federation Francophone de Cancerologie Digestive-Societe Francaise de Radiotherapie Oncologique; SBRT: stereotactic body radiation therapy
In 2010, there were an estimated 43,140 new cases and 36,800 deaths attributed to pancreatic cancer in the United States [1]. The prognosis of pancreatic cancer, regardless of stage, is extremely poor despite recent successes in translational research with an overall 5- year survival rate around 5%. Only a small percent of highly selected patients are able to undergo complete surgical resection with prolonged survival. Unfortunately, the majority of the patients with pancreatic cancer present with unresectable or metastatic stage upon diagnosis. Treatment for metastatic disease is mainly focused on palliation and quality of life, and several regimens are widely used, such as gemcitabine [2], gemcitabine in combination with erlotinib [3] and more recently 5-fluorouracil, leucovorin, irinotecan, oxaliplatin (FOLFIRINOX) [4]. The choice of regimen can depend on patient age, comorbidities and performance status, However, to date there is no clear superior treatment option for locally advanced pancreatic cancer, which carries a median survival of 10 to 13 months. As a result, treatments offered tend to be institution-dependent. It is encouraging to see many studies demonstrating the collective effort of the oncology community to address the different clinical scenarios of pancreatic cancer. This highlight article will discuss five abstracts focusing on the management of locally advanced pancreatic cancer published at the 2011 American Society of Clinical Oncology (ASCO) Annual Meeting.
Gemcitabine, Erlotinib and Radiation
The role of chemoradiation after induction gemcitabine-based chemotherapy vs. chemotherapy alone has been a long standing debated issue. Two recent key randomized trials which have been influential are the Federation Francophone de Cancerologie Digestive-Societe Francaise de Radiotherapie Oncologique (FFCD-SFRO) study and the Eastern Cooperative Oncology Group (ECOG) 4201 study, but they have shown conflicting results. Historically, chemoradiation with 5-FU had achieved overall survival ranging 8.6-11 months: 8.6 months (FFCD-SFRO study) [5], 9.3 months (Gastrointestinal Tumor Study Group, GITSG 9273 study), [6] and 11.0 months (gemcitabine-based chemoradiation, ECOG 4201 study) [7]. Chemotherapy with gemcitabine alone had achieved overall survival ranging 9.2-14 months: 9.2 months in ECOG 4201 [7], 14 months in FFCDSFRO [5]. Furthermore, whether a targeted therapy such as erlotinib could play a role in locally advanced pancreatic cancer is also a key area of investigation.
The LAP-07 study (Hammel et al., Abstract #e14619), a multi-institutional phase III trial, was designed to address the above clinical questions [8]. The study started in 2008 with a targeted accrual of 902 patients and has enrolled 323 patients by the ASCO Annual Meeting this year. To date, LAP-07 is expected to be the largest randomized study dedicated towards locally advanced pancreatic cancer.
There are two randomizations within this phase III study. First, patients will be randomized to receive either gemcitabine alone or gemcitabine/erlotinib (100 mg/day). Then for patients with stable disease after 4 months of chemotherapy, there is a second randomization of either continuing their chemotherapy or receiving chemoradiation to 54 Gy with concurrent capecitabine 1,600 mg/m2. Patient in the erlotinib combination arm will continue with erlotinib alone as maintenance therapy at 150 mg/day after completion of their chemotherapy or chemoradiation. Patients will be stratified by performance status, center, and initial arm of treatment. The abstract updated on the current accrual status, and there will be significant anticipation towards the final results of this large phase III trial.
Interferon Based Therapy
There is now increased interest in the role of immunomodulation in chemoradiation approaches to disease with poor prognosis. Interferon-based chemoradiation has been explored as a therapeutic option for both resectable and locally advanced pancreatic cancer. The addition of interferon to chemoradiation may provide a potential therapeutic benefit through possible synergism with 5-FU, radiosensitization, and/or through immunomodulation.
Picozzi et al. (Abstract #e14648) reported a single center experience on using interferon-based chemoradiation as initial therapy for locally advanced pancreatic cancer [9]. In this abstract, the investigators studied the efficacy of interferon-based chemoradiation for locally advanced pancreatic cancer. Fifty-four patients were reported. The regimen included radiation to 5,040 Gy (28 fractions), cisplatin 30 mg/m2 i.v. weekly for 5 weeks, 5-FU 175-200 mg/m2 i.v. continuous on days 1-38, and interferon 3x106 U every 3 days per week for a total of 17 doses. Although the response rate was 10% per Response Evaluation Criteria in Solid Tumors (RECIST) criteria and the median overall survival was 17 months, there were significant side effects to the regimen, with several grade 3 toxicities including mucositis, nausea/ vomiting, and neutropenia. Larger, randomized studies will be needed to further investigate the efficacy of this approach.
Sorafenib, Gemcitabine and Radiation
Aparicio et al. (Abstract #e14525) presented a small phase I study to investigate the tolerability of sorafenib to concurrent chemoradiation with gemcitabine in treating locally advanced pancreatic cancer [10]. Twelve patients with inoperable pancreatic cancer were enrolled in the study. All patients received gemcitabine 300 mg/m2 weekly x5 concurrent with 45 Gy radiation therapy targeting the primary tumor without prophylactic nodal coverage. Sorafenib dose was escalated from 200 mg daily (3 patients), 400 mg daily (6 patients), to 400 mg twice daily (3 patients). Sorafenib was well-tolerated with only grade 2 fatigue, neutropenia, nausea, and transaminitis as the most commonly observed toxicities. The abstract did not release some important information such as V600E mutation status or resectability rate, which could be addressed in later phase 2/3 trials. Combining conventional chemotherapy with molecular targeted therapy has been a common trend in recent cancer trials. However, in most scenarios, benefit has been seen for patients carrying specific mutations. Phase II and/or phase III studies enrolling selected patients will need to be conducted to see whether surgical resectability and/or survival will be improved with this combination therapy.
A Triple Approach Strategy
Cantore et al. (Abstract #e14607) presented a trial investigating the role of radiofrequency ablation (RFA) in locally advanced pancreatic cancer [11]. In addition to RFA, all patients were treated with either concurrent external-beam radiation therapy (EBRT) plus low dose gemcitabine (40 mg/m2 twice weekly) or intra-arterial epirubicin plus cisplatin (35 mg/m2 and 42 mg/m2 day 1 every 4 weeks, respectively) combined with systemic gemcitabine (1,000 mg/m2 on day 2 every 4 weeks) and capecitabine (650 mg/m2 x 14 days), or both. Among 107 patients, 32 had triple-modality treatment. The overall survival for unselected patients was 25.6 months while, for patients who received all three modalities, the median survival reached 34 months. Three patients in this group achieved pathological complete response. This triple-modality approach including both local and systemic chemotherapies, radiation as well as RFA shows promising preliminary results as a novel approach for locally advanced pancreatic cancer management. Unfortunately, the toxicity profile was not reported here, which would be important to note in this aggressive treatment approach. Larger randomized trials are needed to confirm the impressive results of this study.
CyberKnife® Stereotactic Radiation
Stereotactic body radiation therapy (SBRT) is an emerging recent technology which has produced promising results in palliation and local control of metastatic disease in several body sites. Whether SBRT provides palliative benefit in pancreatic cancer has not been established. A retrospective study (Shirazi et al., Abstract# e14506) reviewed 26 patients with locally advanced or metastatic disease [12]. In addition to CyberKnife® treatment (35 Gy in 5 fractions), the majority had either prior chemotherapy or prior chemoradiation. As expected, SBRT had no major toxicities while providing significant pain relief (86%) and local disease control (78%). The median overall survival in this heavily-pretreated population reached 10 months; however, the abstract lacked information regarding use of other lines of therapy such as capecitabine or erlotinib. Local palliation plays a major role in pancreatic cancer, and SBRT could be considered in selected patients.
The optimal therapy for patients with locally advanced pancreatic cancer remains unclear. The well-designed LAP07 study could provide significant insight towards this issue [8]. However, as current accrual is only at 36% of target, this large study may take another 2-3 years before the initial interim analysis.
Interferon is attractive with its potential roles as an immunomodulator, a radiosensitizer and/or synergistic to 5-FU based chemoradiation; however, interferon therapy is known to cause intolerable side effects even without concurrent radiotherapy. The true benefit of this approach needs to be carefully investigated in a larger study [9].
The multi-tyrosine kinase inhibitor, sorafenib, has gained significant attention in recent years. In addition to hepatocellular carcinoma and renal cell carcinoma, sorafenib has potential efficacy in other malignancies such as melanoma, thyroid cancer, and lung cancer. Most clinical trials investigating sorafenib are focusing on selected patients with the V600E mutation. The frequency of the V600E mutation in pancreatic cancer is relatively low, likely in the order of 10% at most. It would be interesting to note how many patients carry the V600E mutation in all the current early phase trials. For locally advanced pancreatic cancer, a median survival of close to 3 years is extremely impressive. However, Cantore’s triple-modality approach reports these excellent outcomes in their recent study [11]. Without detailed toxicity data, however, it is unknown how many patients were able to tolerate all the treatments including intra-arterial chemotherapy, systemic chemotherapy, external-beam radiation and RFA. This aggressive approach would require skillful coordination among the different oncologic specialties.
Stereotactic body radiation therapy (SBRT) is a recent non-invasive radiation therapy option with shorter courses of treatment than conventional fractionated therapy. SBRT could be considered for local symptomatic relief, especially for pain. However, the majority of patients selected in this retrospective study were previously treated with chemotherapy with or without concurrent radiation [12]. Therefore, how to optimally use SBRT in a cost-effective way will require more prospective studies.
The authors have no potential conflicts of interest