- (2012) Volume 13, Issue 2
John Ng, Chi Zhang, Daniela Gidea-Addeo*, Muhammad Wasif Saif
Columbia University College of Physicians and Surgeons, New York Presbyterian Hospital. New York, NY, USA
Pancreatic cancer, the 4th leading cause of cancer death in the U.S., remains a challenging disease for the oncology community. Less than 20% of all cases are potentially cured by surgical resection, while the large majority of cases are deemed either unresectable or metastatic upon diagnosis. Advances in treating locally advanced pancreatic cancer have been few and modest. In this year’s American Society of Clinical Oncology (ASCO) Gastrointestinal Cancers Symposium, three abstracts (#252, #254, #313) were presented with novel approaches towards treating locally advanced pancreatic cancer. Surgery for recurrent disease, a promising new chemoradiation regimen, and the application of an exciting multi-agent regimen (FOLFIRINOX: oxaliplatin, irinotecan, leucovorin, 5-fluorouracil) in a non-clinical trial setting, highlight the novel approaches focused on the management of this difficult disease.
Combined Modality Therapy; erlotinib; Fluorouracil; gemcitabine; Pancreatic Neoplasms; Radiation; Radiotherapy
ASCO: American Society of Clinical Oncol ogy; ECOG: Eastern Cooperative Oncol ogy Group; FFCD-SFRO: Federation Francophone de Cancerologie Digestive and Societe Francaise de Radiotherapie Oncol ogique; FOLFIRINOX: 5- fluorouracil, oxaliplatin, irinotecan, leucovorin; GITSG: Gastrointestinal Tumor Study Group; GTV: gross tumor volume; PRODIGE: Partenarait de Recherche en Oncol ogie Digestive
In 2012, there will be an estimated 43,920 new cases and 37,390 deaths attributed to pancreatic cancer in the United States [1]. The prognosis of pancreatic cancer, regardless of stage, is extremely poor, with a 1-year survival rate of 25% and a 5-year survival rate of less than 5%. Only a small percentage of patients are able to undergo complete surgical resection with potential curative intent. The large majority of patients with pancreatic cancer present either with locally advanced or metastatic disease upon diagnosis. For patients at these advanced, surgically unresectable stages, median survival ranges from 8 to 12 months [2].
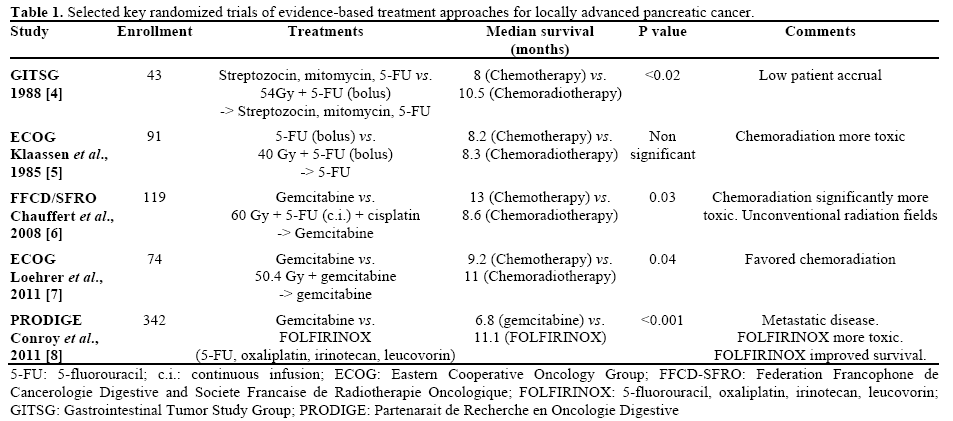
There are different treatment approaches to locally advanced pancreatic cancer management, including single or multi-agent chemotherapy, chemotherapy followed by chemoradiation, or immediate concurrent chemoradiation [3]. A summary of several key randomized trials on locally advanced pancreatic cancer treatment which led to these different approaches is shown in Table 1 [2].
As each of varied approaches are limited in their efficacy, much attention and resources have been devoted to finding novel approaches towards treating locally advanced staged pancreatic cancer. These novel approaches seek to improve overall survival, distal or regional disease control, and/or quality of life. This highlight article will review three key abstracts published at the 2012 American Society of Clinical Oncol ogy (ASCO) Gastrointestinal Cancers Symposium, focusing on several new treatment options to treat locally advanced pancreatic cancer.
Selective Reoperation for Locally Recurrent or Metastatic Pancreatic Ductal Adenocarcinoma Following Primary Pancreatic Resection (Abstract #252 [9])
Thomas et al. presented a single-institutional retrospective study examining the potential for selective reoperation for patients with recurrent disease, a stage which has traditionally been viewed as surgically futile. In their study, they reviewed all patients from 1992-2010 identified in their database who developed recurrent pancreatic adenocarcinoma after intended surgical cure. Of 700 patients who underwent resection for pancreatic adenocarcinoma, 426 patients developed recurrent disease. Twenty-one (5%) of the recurrent patients were then selected for a second, potentially curative operation.
Their results were notable in that patients who were able to undergo a second resection (single technically resectable lesion, good performance status) had a significantly longer disease free interval relative to patients who were not selected. Furthermore, patients who had a surgically resectable lung metastasis had a longer interval between re-operation and second recurrence vs. patients with a liver or locoregional recurrence (no recurrence vs. 7.5 months; P=0.02). Four of the seven patients with resected lung metastasis were still alive after 30 months of follow-up from the reoperation.
The authors concluded that patient who develop a solitary lung recurrence of pancreatic adenocarcinoma to the lung after a long disease-free interval should be considered for reoperation. Other sites of recurrence did not appear to benefit as much from reoperation.
Phase I Trial of Radiotherapy with Concurrent Bevacizumab, Erlotinib, and Capecitabine for Locally Advanced Pancreatic Cancer (LAPC) (Abstract #254 [10])
Skinner et al. presented the results of their phase I study looking at the multiagent regimen of bevacizumab, erlotinib, and capecitabine given concurrently with 50.4 Gy (gross tumor volume (GTV) only) in 28 fractions. The study enrolled 17 patients with biopsy-proven non-metastatic unresectable locally advanced pancreatic cancer. All of these cases had CT staging and had been deemed either borderline resectable or unresectable. All patients received 50.4 Gy (GTV only) in 28 fractions with concurrent capecitabine, bevacizumab and erlotinib, with prior chemotherapy permitted. The dose escalations of agents are shown in Table 2.
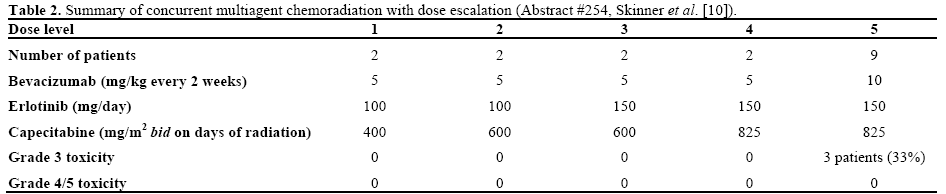
After reassessment for resectability 6-8 weeks later after treatment, 5 patients (4 were originally deemed unresectable and 1 was borderline) achieved marginnegative resections, of whom 4 were treated at dose levels 4 or 5; 3 patients had excellent pathological responses including one complete response at pancreatectomy and are alive up to 22 months with no local or distant failures, comparing to median survival of 24 months for patients treated at dose levels 4 and 5, and median survival of 19.4 months for all patients enrolled.
The authors concluded that concurrent radiotherapy with combination of erlotinib, bevacizumab and capecitabine for locally advanced pancreatic cancer is safe which may achieve promising survival and high rate of resectability at the higher dose levels. A role of dual inhibition of growth factor receptor pathways during chemoradiation is suggested and future evaluations are warranted.
FOLFIRINOX in Locally Advanced or Metastatic Pancreatic Cancer (Abstract #313 [11])
Faris et al. presented with their retrospective study examining the efficacy and toxicity of 5-fluorouracil, leucovorin, irinotecan, and oxaliplatin (FOLFIRINOX) at their institution for both metastatic and locally advanced disease in the non-clinical trial setting. FOLFIRINOX has garnered a great deal of recent interest as it has been demonstrated in a phase III trial that FOLFIRINOX improved survival compared to gemcitabine in good performance status patients with metastatic pancreatic cancer [8]. The authors followed up on this trial by a retrospective study in their institutional experience on the efficacy and tolerability of FOLFIRINOX. A summary of their results with clinical characteristics and gradable toxicities is shown in Table 3. Formal radiographic reviews were performed to determine best overall response rates.
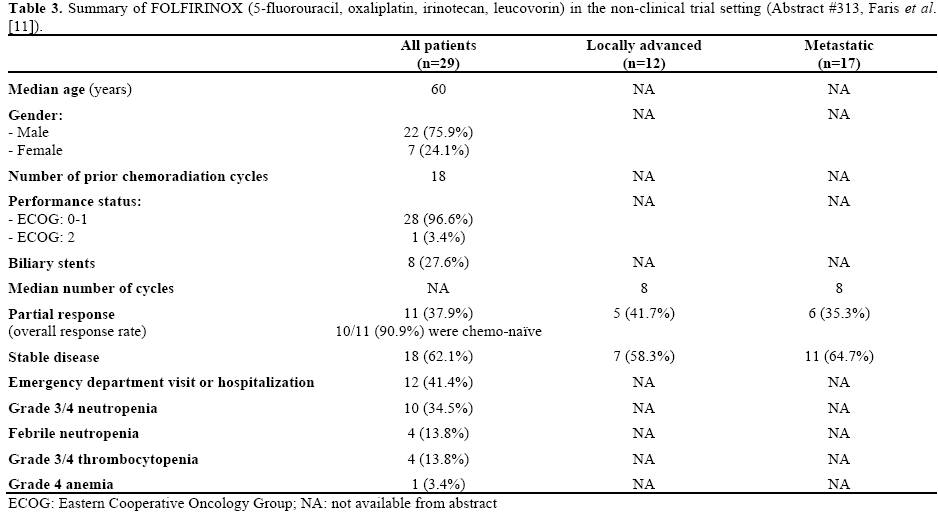
In the non-clinical trial setting, the authors concluded that FOLFIRINOX demonstrated activity in both the metastatic and locally-advanced settings with more than one of three patients showing partial response. However, this regimen is associated with manageable, but significant toxicities, with over 40% of patients requiring emergency department visit or hospitalization.
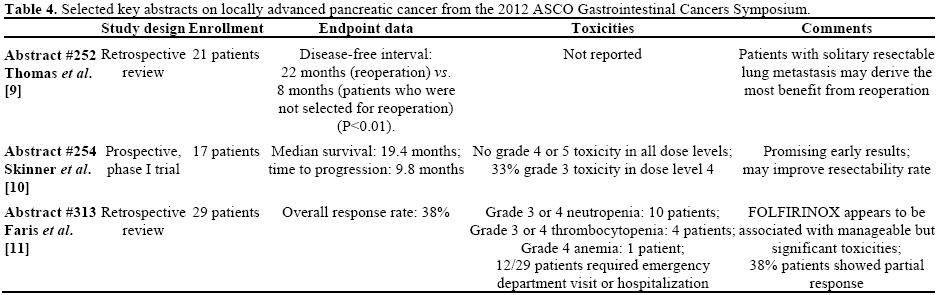
A summary of the three abstracts (#252, #254, and #313) on locally advanced pancreatic cancer from the 2012 ASCO Gastrointestinal Cancers Symposium is shown in Table 4.
The optimal therapy for patients with locally advanced pancreatic cancer remains unclear. There is data to support treatment with chemotherapy alone, chemoradiation, or induction chemotherapy followed by combined modality treatment. The choice of regimen can depend on patient age, comorbidities, and performance status and often varies amongst different institutions. To date, there has been no clear demonstration of a markedly superior treatment option for locally advanced pancreatic cancer, which carries a median survival of 10 to 13 months.
There appears to be several new approaches on the horizon that may add to the array of treatment strategies for this challenging disease. Gemcitabine has been an established standard with a reasonable toxicity profile and is often used either as a single agent or as an induction and maintenance regimen. The emergence of FOLFIRINOX in the metastatic setting has spurred interest in its use in the locally advanced setting [8]. From the work of Faris et al. (Abstract #313 [11]) there appears to be a role in FOLFIRINOX in both the metastatic and the locally advanced setting, and that while there are significant toxicities associated with this rigorous regimen, it can used effectively outside of a clinical trial setting. Erlotinib has also been shown to modestly improve survival when used in combination with gemcitabine in metastatic pancreatic cancer in comparison to gemcitabine monotherapy in a phase III trial [12]. These results have led to its addition with bevacizumab in a multi-agent combination to improve the therapeutic window in the chemoradiation setting. The results of Skinner et al. (Abstract #254 [10]) suggest that it may improve resectability rate, but as a phase I trial, that conclusion will require further studies to be validated. Finally, recurrent/metastatic pancreatic cancer traditionally has been considered a surgically futile disease. The surgical literature from cancers of other sites, most notably colorectal cancer, has suggested that surgical resection of solitary metastases can lead to substantial long term survival [13]. The study by Thomas et al. (Abstract #252 [9]) would indicate that there may be certain subsets of recurrent metastatic pancreatic cancer patients who may greatly benefit from a second resection.
At present time, the treatment options for locally advanced pancreatic cancer confer modest results. As illustrated by recent presentations at the 2012 ASCO Gastrointestinal Cancers Symposium, tremendous work is being done in an effort to improve the outcome of patients with locally advanced pancreatic cancer.
The authors have no potential conflicts of interest