Case Report - (2021) Volume 22, Issue 4
1Endoscopy Unit, 9 de Julho Hospital, São Paulo, Brazil
2Department of Gastrointestinal Endoscopy, Hospital Universitario PresidenteDutra , Sao Luiz, Maranhão, Brazil
Received Date: May 02nd, 2021; Accepted Date: May 20th, 2021
Autoimmune pancreatitis (AIP) is a recurrent, infiltrative, inflammatory disease, which is not limited to pancreatic involvement and has a multiform clinical presentation.Morphological changes lead to irreversible destruction of the exocrine and endocrine glands with consequent pancreatic insufficiency. Interest in AIP has increased due to the recognition of radiological features such as irregular narrowing of the main pancreatic duct (MPD), pancreatic parenchyma alterations, IgG4 elevation, and lymphoplasmacytic infiltrate with abundant plasma cells. The diagnosis is made in patients with painless obstructive jaundice secondary to an inflammatory mass involving the biliary tract, accompanied by abdominal pain, weight loss, and increased levels of carbohydrate antigen 19-9 (CA19-9), mimicking pancreatic carcinoma. Tissue procurement is considered the “gold standard” for the diagnosis of AIP5. We report a case of IgG4 syndrome with a significant increase in CA19-9 level, acute pancreatitis, and enlargement of the pancreatic gland mimicking pancreatic carcinoma. An accurate diagnosis was obtained by EUS-FNA, and steroid treatment avoided unnecessary surgery.
Autoimmune pancreatitis; Endoscopic ultrasound; Fine needle biopsy; Immunoglobulin G4-Related Diseases; Follow-Up
Autoimmune pancreatitis (AIP) is a recurrent, infiltrative, inflammatory disease, which is not limited to pancreatic involvement and has a multiform clinical presentation [1]. Morphological changes lead to irreversible destruction of the exocrine and endocrine glands with consequent pancreatic insufficiency [2]. Interest in AIP has increased due to the recognition of radiological features such as irregular narrowing of the main pancreatic duct (MPD), pancreatic parenchyma alterations, IgG4 elevation, and lymphoplasmacytic infiltrate with abundant plasma cells [3]. The diagnosis is made in patients with painless obstructive jaundice secondary to an inflammatory mass involving the biliary tract, accompanied by abdominal pain, weight loss, and increased levels of carbohydrate antigen 19-9 (CA19-9), mimicking pancreatic carcinoma [4]. Tissue procurement is considered the “gold standard” for the diagnosis of AIP [5]. We report a case of IgG4 syndrome with a significant increase in CA19-9 level, acute pancreatitis, and enlargement of the pancreatic gland mimicking pancreatic carcinoma. An accurate diagnosis was obtained by EUS-FNA, and steroid treatment avoided unnecessary surgery
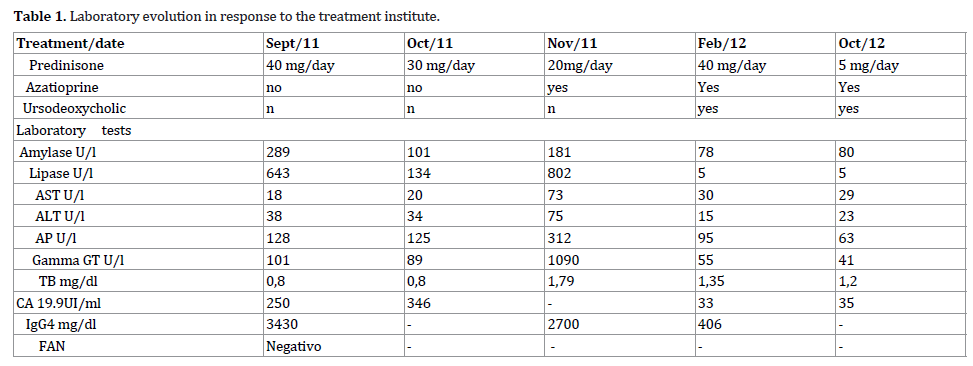
A 65-year-old man presented with recurrent upper abdominal pain and back irradiation for 30 days. The symptoms improved with oral analgesia and fasting. He reported unmeasured weight loss and asthenia and denied alcoholism. There was a history of type 2 diabetes mellitus 1 year previously, hypothyroidism, and dyslipidemia. Additional findings were CA19- 9 250 mg/dL; carcinoembryonic antigen (CEA), normal; antinuclear factor negative; and IgG4 3430 IU/L. Computed tomography (CT) showed diffuse and uncharacteristic enlargement of the pancreatic head. Magnetic resonance cholangiopancreatography (MRCP) detected a heterogeneous, enlarged, "sausage" pancreas (Figures 1). The main pancreatic duct (MPD) was irregular, with dilated and stenosed areas. Endoscopic ultrasound showed a diffusely enlarged, heterogeneous pancreas, with hypoechogenic images on the head and tail. The MPD was irregular, and we detected the presence of inflammatory peripancreatic lymph nodes (Figures 2). Microhistological examination showed chronic AIP with marked acinar atrophy, plasmacytic epithelial permeation, eosinophilic exudate, and IgG4 positivity (Figures 3). Based on the diagnosis, corticosteroid therapy was initiated with prednisone 40 mg/day, systematically reduced by 5 mg every 2 weeks, resulting in significant clinical improvement, weight gain, disposition, and drop in laboratory test levels during the first 2 months. However, with the reduction of the medication dose, the patient developed new abdominal pain and altered laboratory test results. As the diabetes mellitus was difficult to control and was significantly altered in the bone densitometry examination, azathioprine 5 mg/kg was started in an attempt to maintain low doses of corticosteroids. The patient started with complaints of dry mouth, discomfort, and palpable lymph nodes in the cervical region and changes in urination. Specific examinations, such as submandibular gland scintigraphy, cervical ultrasound, and urological examination, detected submandibular gland insufficiency, autoimmune cervical lymphadenopathy, and prostatitis. In control laboratory tests, pancreatic enzyme levels were normal, but transaminases, cholestatic enzymes, and tumor markers increased (Table 1). Repeated MRCP revealed symmetrical dilatation of the intrahepatic biliary tract with reduction in caliber near the confluence of the main ducts. With the improvement, it was decided to adjust the doses of corticosteroids and azathioprine. After 3 months, the patient had a complete clinical and laboratory remission. With the complete action of the immunosuppressant, a slow and gradual reduction of corticosteroid dosage was achieved, resulting in 3 years of follow-up without relapse (Table 1). In the current follow-up, 8 years after diagnosis there is an evident sign of mild pancreatic insufficiency. MRCP shows MPD dilatation and tortuosity, associated with parenchymal atrophy, with a diagnosis of chronic calcifying pancreatitis.
In North America, about 2.5% of patients undergoing Whipple surgery for probable pancreatic carcinoma are later diagnosed with AIP, and 20% of cases of Whipple procedures for benign conditions can now be considered as AIP [6]. Before the diagnosis of AIP, our patient was indicated for surgical treatment due to a pancreatic head mass, weight loss, and elevated CA19-9. AIP is one of a group of diseases that are associated with high levels of IgG4 and are capable of being the etiology of acute or chronic pancreatitis of unknown cause. EUS-FNA was critical for the diagnosis and initiation of treatment in our patient. Examination showed either a diffusely enlarged, hypoechogenic pancreas or a solitary mass in the pancreas [7]. In these patients, fine-needle aspiration reveals IgG4- positive lymphoplasmacytic infiltrates, as occurred in our patient [8]. Because it is a relatively recently recognized condition, the diagnosis of AIP is often not made, which may result in delayed clinical treatment or unnecessary surgical procedures. We should investigate for the presence of AIP (IgG4 syndrome) in patients, mainly men over 50 years old, who have acute or chronic pancreatitis of unknown cause and a mass in the head of the pancreas. EUS-FNA avoided unnecessary Whipple surgery and determined the best treatment for the pancreatic mass identified by imaging methods.
All named authors hereby declare that they have no conflicts of interest to disclose.