- (2007) Volume 8, Issue 2
Maruti Govindappa Raghu1, Jai Dev Wig1, Rakesh Kochhar2, Dheeraj Gupta3, Rajesh Gupta1, Thakur Deen Yadav1, Ritesh Agarwal3, Ashwini Kumar Kudari1, Rudra Prasad Doley1, Amit Javed1
Departments of 1General Surgery, 2Gastroenterology and 3Pulmonary Medicine, Postgraduate Institute of Medical Education and Research, Sector 12. Chandigarh, India
Received November 15th, 2006 - Accepted December 20th, 2006
Context Severe acute pancreatitis has long been known to be a cause of pulmonary dysfunction and multisystem organ failure. Objective We evaluated the spectrum of pulmonary dysfunction in acute pancreatitis. Methods Over a period of one year, 60 patients referred to us with a diagnosis of acute pancreatitis on the basis of clinical findings, CT and elevated serum amylase level were studied prospectively. The computed tomography severe index (CTSI) was used to assess the severity of the pancreatitis. Arterial blood gas analysis and chest X-rays were performed in all patients at admission and at intervals, when clinically indicated. Results The mean age was 42.9±15.9 years (range: 18-80 years) and the etiology of the pancreatitis was gallstones in 29 patients, alcohol in 22 patients while no cause could be ascertained in 9. At presentation to our hospital, 48.3% had mild hypoxemia while 18.3% had moderate to severe hypoxemia (PaO2 less than 60 mmHg). The patients who were hypoxemic at presentation had a higher incidence of organ failure during the course of the disease. Pleural effusion at admission was noticed in 50%, atelectasis in 25%, and pulmonary infiltrates in 6.7%. Respiratory failure developed in 48.3% and the mean±SD CTSI in these patients was 8.20±2.29. Patients with more than 50% necrosis had more pulmonary dysfunction and needed ventilatory support. The development of consolidation during the course of the disease correlated with the occurrence of respiratory failure (P=0.068) but not with mortality (P=0.193). Similarly, the onset of adult respiratory distress syndrome also correlated with respiratory failure (P
Lung; Multiple Organ Failure; Pancreatitis /complications; Pancreatitis, Acute Necrotizing; Pleural Effusion
AP: acute pancreatitis; ARDS: adult respiratory distress syndrome; CTSI: CT severity index; MSOF multisystem organ failure; PaO2: partial pressure of oxygen; SAP: severe acute pancreatitis
Severe acute pancreatitis (SAP) occurs in up to 20% of patients with acute pancreatitis (AP) and it has a high mortality rate. High mortality in early stages is attributed to multisystem organ failure (MSOF) [1, 2, 3, 4]. Early severe acute pancreatitis has been defined as the presence of at least one organ failure on admission and, once organ failure is noted on admission, MSOF develops or progresses despite intensive care treatment in nearly 80% of patients [4]. The mortality rate in this group is 42% as compared to 12% in patients with SAP without organ failure [5]. Progressive organ dysfunction carries a mortality rate of 35 to 55% [4].
Pulmonary dysfunction ranging from hypoxemia to acute respiratory distress syndrome (ARDS) is one of the most important systemic manifestations of SAP occurring in 30-50% of patients [3, 6, 7, 8, 9]. Pulmonary dysfunction is the major factor of mortality in 22-25% and a contributing factor in an additional 30% of patients with AP [7]. Respiratory dysfunction precedes heart, liver and kidney failure and is responsible for early deaths in SAP [7]. In an autopsy study, it was reported that 60% of patients with acute pancreatitis died within 7 days of admission predominantly from respiratory failure [10]. Oxygen saturation of 92% or below is reported to be an independent predictor of the severity of AP and is reported in 44% of patients with SAP [11]. Pulmonary infiltrates, pleural effusion and hypoxemia are markers of SAP [12, 13, 14]. A logistic regression analysis showed that radiological abnormalities of the chest were associated with a 15-fold increase in the mortality rate [15].
The objectives of the present study were to identify the spectrum of pulmonary complications at base line in patients with acute pancreatitis, correlate these with the outcome and define the significance of respiratory complications developing during the course of hospitalization.
MATERIAL AND METHODS
Patients
The study included all the consecutive patients presenting with their first attack of AP admitted to the First Unit of the Department of General Surgery in a 1,300- bed tertiary care hospital during a one year period (from July 2004 to June 2005). All the patients were referred to our unit from primary and secondary level hospitals of Northern India with a diagnosis of acute pancreatitis. The primary reason for referral was the severity of the disease and the need for intensive care. Patients with underlying respiratory diseases were excluded. The diagnosis of AP was made on the basis of clinical symptoms and signs, and confirmed by an elevated amylase level, ultrasound, computed tomography and/or surgical findings. Sixty patients were enrolled in the study (44 males, 16 females; mean±SD age: 42.8±15.9 years; range: 18-80 years).
The following laboratory measurements were obtained in all patients at admission: serum amylase levels, white blood cell counts, hematocrit, electrolytes, blood glucose, serum creatinine, liver function tests (AST, ALT, and bilirubin) and coagulation profile. Baseline arterial blood gas analysis was recorded at room temperature and all patients had a routine chest X-ray at admission. Arterial oxygen pressure was monitored daily when respiratory insufficiency occurred. AQ chest X-ray was repeated periodically as per clinical observations. A contrast-enhanced CT (CECT) was performed on 56 patients, and the severity of the pancreatitis was established as per criteria suggested by Balthazar based upon the CT severity index (CTSI) [16]. Four patients were too sick to be transported to the radiology facility.
Interventions
All the patients were treated with a consistent treatment strategy in a critical care unit using intravenous fluid, nasogastric suction, analgesics and antibiotics for the severe pancreatitis. Nasojejunal feeding was initiated in 21 patients while 17 received parenteral nutrition. Monitoring of respiratory failure, renal failure, shock and coagulation parameters was carried out during the hospital stay (mean±SD: 20±16 days). Patients were transferred to the ICU for ventilatory support if they had respiratory distress, severe hypoxia or ARDS. Patients with infected necrosis and clinical deterioration despite aggressive management underwent necrosectomy
Informed consent was obtained from each patient and the study protocol was approved by the Institute Ethics Committee.
Data are reported as means, standard deviations (SD) and frequencies. Statistical analyses were performed using the statistical software SPSS® version 10.0 for MSWindows ® (SPSS Inc., Chicago, IL, USA). Continuous variables were compared using the Mann-Whitney U test while the Fisher’s exact and the liner-by-linear association chisquared tests were used for categorical variables. In addition, the variables were analyzed using univariate logistic regression to derive a crude odds ratio and, if the P values found were less than 0.1, these variables were then entered into a multivariate logistic regression model to arrive at an adjusted odds ratio. The 95% confidence intervals (95% CI) were also computed.
The etiology of AP was: gallstones in 29 patients (48.3%), alcohol in 22 (36.7%) and no cause was detected in 9 (15.0%) patients. The patients had presented at our hospital from 2 to 25 days (mean 11.1 days) after the onset of symptoms. A CECT was performed on 56 (93.3%) patients and the CTSI calculated: 11 (19.6%) patients had a CTSI between 1 and 3, 15 (26.8%) had a CTSI between 4 and 6, and 30 (53.6%) had a CTSI greater than 6. Twenty-seven (48.2%) patients had more than 50% necrosis, 3 (5.4%) had 30-50% necrosis and 13 (23.2%) had less than 30% necrosis while 13 (23.2%) had no necrosis.
Hypoxemia at presentation was seen in 40 (66.6%) patients: 29 (48.3%) had a PaO2 between 60 and 80 mmHg while 11 (18.3%) had a PaO2 less than 60 mmHg. Three patients with hypoxemia did not undergo CECT at presentation. A significant positive correlation was observed between hypoxemia and the extent of the necrosis (P<0.001) (Table 1). In addition, the presence of pleural effusion, pneumonia, ARDS, and respiratory failure, but not atelectasis, were positively correlated with the extent of the necrosis. As shown in Table 2, the hypoxemia was significantly associated with the need for mechanical ventilation, cardiovascular failure, renal failure and mortality, but not with coagulopathy (Table 2).
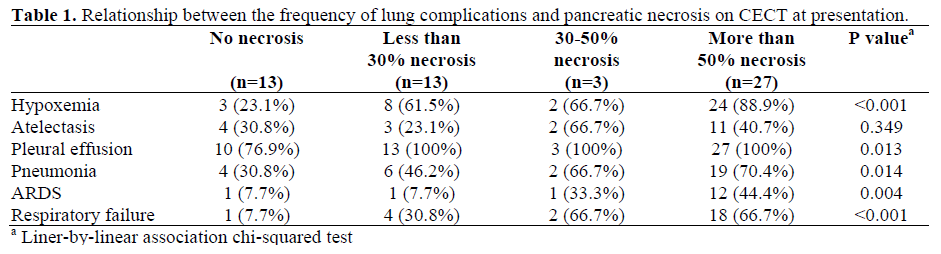
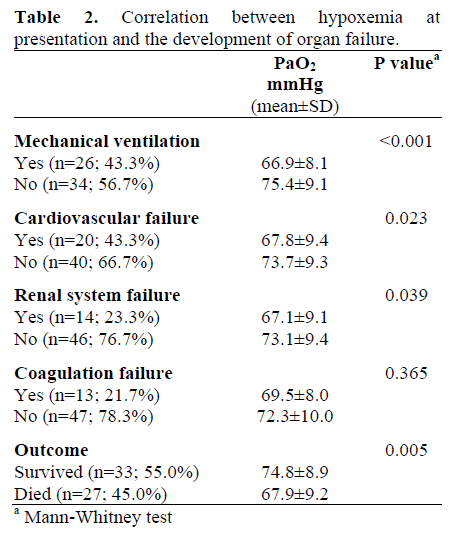
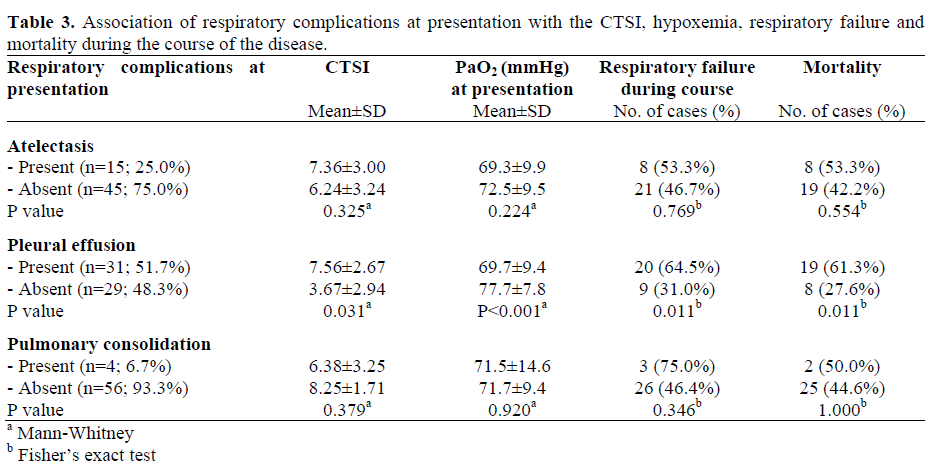
Table 3 shows the correlation between atelectasis, pleural effusion, and pulmonary consolidation, and CTSI, PaO2, respiratory failure and outcome. Pleural effusion was significantly associated with CTSI (P=0.031), hypoxemia at presentation (P<0.001), occurrence of respiratory failure (P=0.011) and mortality (P=0.011). The presence of atelectasis and consolidation, however, were not significantly associated with CTSI, hypoxemia at presentation, respiratory failure or mortality (Table 3).
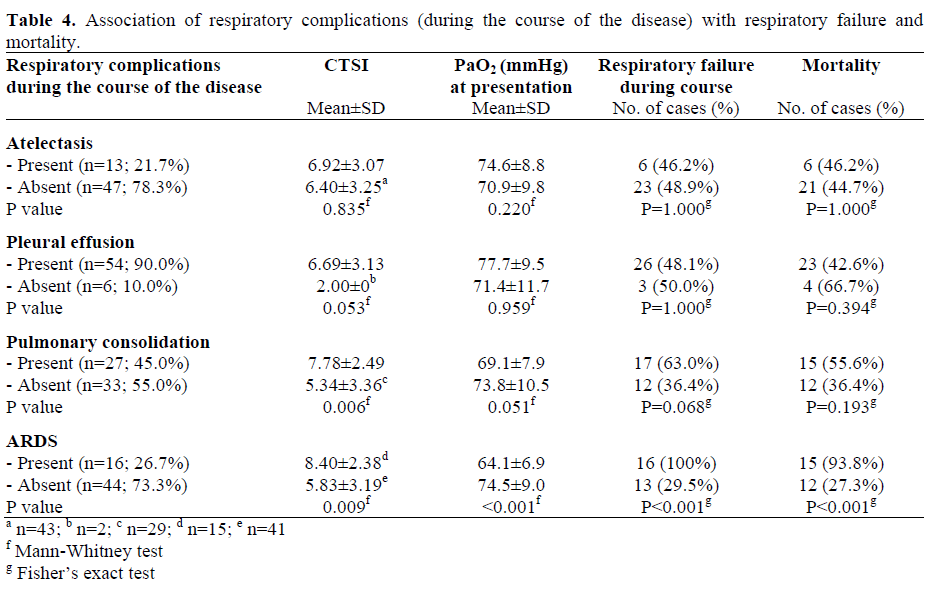
hypoxemia at presentation, respiratory failure or mortality (Table 3). Table 4 gives the number of patients who had atelectasis, pleural effusion, pulmonary consolidation and ARDS during the course of hospitalization as well as the correlation of these complications with the CTSI, hypoxemia at presentation, respiratory failure, and mortality. The occurrence of pleural effusion and atelectasis during hospitalization did not have any significant correlation with any of the four parameters studied. The development of pulmonary consolidation significantly correlated with the CTSI, (P=0.006) but not with mortality (P=0.193). Correlation of the development of pulmonary consolidation with hypoxemia and the development of respiratory failure did not reach statistical significance (P=0.051 and P=0.068, respectively). The presence of ARDS, however, had a significant association with the CTSI (P=0.009), hypoxemia at presentation (P<0.001), the development of respiratory failure (P<0.001), and mortality (P<0.001).
A total of 26 (43.3%) patients needed ventilatory support (mean 7 days; range: 1 to 35 days). Fourteen patients were put on mechanical ventilation for severe hypoxia or ARDS. Twelve patients required postoperative ventilation.
A total of 27 patients died; 15 of them had necrosectomy while 12 were being managed conservatively. ARDS was the sole cause of death in 9 patients while in another 9, it was a part of the MSOF. The other 9 patients died from the failure of other organs.
Pulmonary dysfunction is a major component of MSOF and contributes to early mortality in patients with SAP [8, 16, 17, 18, 19]. Knowledge of these manifestations may aid in identifying of high risk groups so that supportive measures are instituted early in the course of the illness. Talamini et al. [13] have confirmed that a serum creatinine level greater than 2 mg/dL and pathological chest radiograph findings (for the presence of pleural effusion and/or pulmonary parenchymal densification) are two simple tests capable of identifying, within 24 hours of admission to hospital, subgroups of patients with more severe disease or adverse clinical outcome. Bracey et al. [10] have shown that an oxygen saturation of less than 92% appears to be an independent predictor of severity, 44% of patients with oxygen saturation of less than 92% had severe disease; in comparison, by using the Glasgow score, 40% of patients with predicted severe disease developed complications.
The spectrum of pulmonary sequelae range from subclinical reductions of arterial oxygen tension to ARDS. Mild hypoxemia (PaO2 60- 80 mmHg) at presentation was present in 48.3% of our patients while 18.3% had moderate to severe hypoxemia (PaO2 less than 60 mmHg). Hypoxemia at presentation was significantly associated with the development of ARDS during the course of the disease and was a significant risk factor for mortality; in fact, patients with increasing PaO2 levels had a decrease in mortality of 92% for every 1 mm Hg increase in PaO2 levels (OR: 0.92; 95% CI: 0.87-0.98; P=0.008) i.e. an 8% decrease of the probability of mortality. Hypoxemia at presentation was not related to the development of atelectasis, pleural effusion or pulmonary consolidation during the course of the disease. A recent study has shown that a baseline hypoxemia of less than 60 mmHg was a significant risk factor for pulmonary consolidation and ARDS, and can be used as a marker of poor outcome [6]. Our observation and derivations are based on data recorded at presentation to our specialized unit in a tertiary care center. All 60 patients were referred, and they arrived at our hospital after a mean of 11 days (range: 2-25 days) from the onset of the pancreatitis. Thus, the hypoxia noted in our patients may actually be hypoxia after the disease has progressed.
It has been suggested that hypoxemia may precede radiological findings and it is an independent early predictor of pulmonary pathological derangements [6]. Impaired alveolar gas exchange has been documented in acute pancreatitis and is correlated with the severity of the disease [20]. The main mechanism of lung injury in acute pancreatitis is increased microvascular permeability [21]. Approximately 30% of cases overall develop acute lung injury while ARDS accounts for a significant proportion of deaths [7].
Abnormal chest radiographic findings can be seen in up to 55% of patients with acute pancreatitis and include pleural effusion, pulmonary infiltrates, and pulmonary edema related to ARDS. Pleural effusion has been reported in 4 to 20% of patients [6, 8, 12, 22], though Lankisch et al. [23] demonstrated pleural effusion in 50% of their patients. Fifty percent of our patients had pleural effusion at admission. This high incidence could be due to a high proportion of severe pancreatitis and late presentation (mean 11 days). Pleural effusion has been found to be associated with severe pancreatitis and poor outcome [13, 22, 23]. In one study, pleural effusion was seen in 84.2% of severe pancreatitis patients and only in 8.6% of mild pancreatitis patients [12]. Lankisch et al. showed a correlation of pleural effusion with severe morphological changes and necrosis, and concluded that it is a negative prognostic marker of the disease [23]. Heller et al. [12] similarly reported that pleural effusion has a sensitivity of 84.2% and specificity of 91.4% for severe disease as manifested by pancreatic necrosis or organ failure. We also observed that the presence of pleural effusion at presentation was significantly associated with the severity of the pancreatitis (as evidenced by a CTSI equal to or greater than 7), occurrence of respiratory failure and poor outcome. A correlation between pleural effusion at admission and severe disease has been well documented and, in fact, it has been recommended that search for pleural effusion by ultrasound be carried out in all patients [22]. Some studies have found a higher incidence of pleural effusion in alcoholic pancreatitis patients than in gallstone pancreatitis patients [17] while others have not found this correlation [22]. We also did not observe any association between the etiology of the acute pancreatitis and the presence of pleural effusion (data not shown).
We found pleural effusion at presentation to be bilateral in about a half of the patients and left sided in about 25%. Other authors have reported bilateral effusion in up to 77% of patients [12, 23]. All 22 patients who underwent aspiration of the pleural effusion had a pleural fluid protein/serum protein ratio greater than 0.5. Pleural fluid amylase was elevated more than serum amylase in 8 patients (36.4%), suggesting a disruption of the pancreatic duct.
Atelectasis was seen in 15 (25.0%) patients and pulmonary consolidation in 4 (6.7%) patients at admission, and neither of the two had any significant correlation with the CTSI, respiratory failure or outcome (Table 3). Lankisch et al. [14] have observed that 26% of their patients had pulmonary infiltrates and that there was a positive correlation between pulmonary infiltrates and the CTSI, Ranson’s score and mortality
Not many studies have looked at the development of additional pulmonary changes during hospitalization for acute pancreatitis. In one study, 15% of the patients had radiological abnormalities at admission and an additional 71% of patients developed abnormalities during hospitalization [24]. In our study, the number of patients with pleural effusion increased from 31 (51.7%) to 54 (90.0%) and those with consolidation from 4 (6.7%) to 27 (45.0%) while there was a marginal decrease in patients having atelectasis, from 15 to 13. In the natural history of acute pancreatitis, one third of deaths occur during the early phase, a majority of them due to severe lung injury [25]. The second phase is related to the development of complications of the injured pancreas [15]. These complications include fat necrosis, pseudocyst formation and pancreatic abscess, and systemic complications including pulmonary complications [15]. The timing of the development of the pulmonary complications from the onset of acute pancreatitis has been reported to be around 4.2 days for pleural effusion, 5 days for atelectasis and 12.2 days for ARDS [6]. The development of consolidation during hospitalization correlated with the occurrence of respiratory failure for obvious reasons. Adequate treatment of consolidation was able to prevent fatality in our study.
ARDS occurred in 16 (26.7%) of our patients during the course of the disease and 15 (93.8%) of them died. ARDS developed significantly more often in those with a higher CTSI and it correlated with the development of respiratory failure and death (Table 4). ARDS is reported to occur in up to 15% of all patients with acute pancreatitis, those with severe disease which requires prolonged hospitalization being at greater risk [26]. Local and systemic infections can contribute to the worsening or the persistence of preexistent ARDS [15]. Polyzogopoalou et al. have reported that baseline hypoxemia is an independent risk factor for the development of ARDS [6] and this was also our observation.
Mechanical ventilation is an important adverse factor for outcome in acute pancreatitis [27]. Jacobs et al. [28] showed that 10% of their patients needed mechanical ventilation, and mortality in this group was 75%. Twenty-six (43.3%) out of the 60 patients required mechanical ventilation; of the 26 patients, 22 (84.6%) died. This would also explain the overall high mortality (45.0%) in our patients.
The present study suffers from referral bias on the part of the tertiary care referral center. All our patients had been referred to us from other hospitals with a diagnosis of severe pancreatitis which required intensive care. Moreover, a mean period of 11 days had already elapsed before the patients reported to us. Thus, the baseline evaluation carried out in our hospital was after an obvious progressive course of the disease. We have been unable to obtain the data from the referral hospitals in terms of actual baseline parameters. Nevertheless, our data reflects the clinical course and outcome in patients seen in a tertiary care center. Our results are in accordance with those of previous studies which suggest that the development of hypoxemia in patients with acute pancreatitis is associated with an adverse outcome.
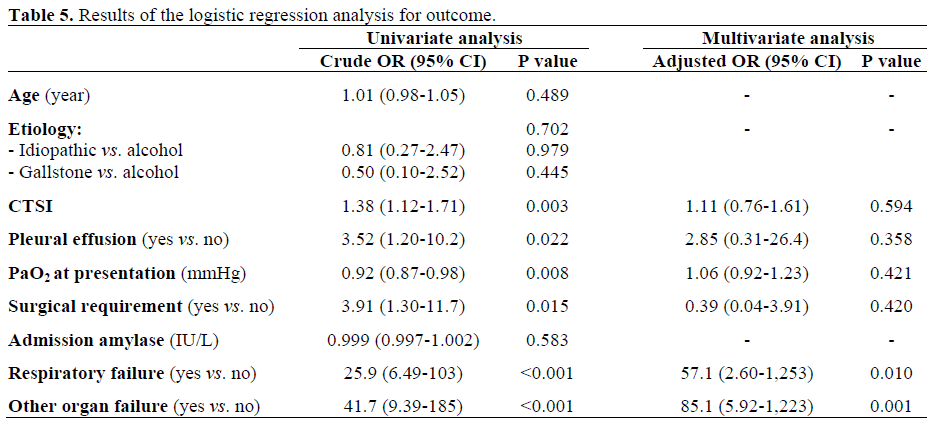
On logistic regression analysis for outcome, the development of respiratory failure and other organ dysfunctions were independent risk factors for mortality (Table 5). Baseline PaO2 did not emerge as a risk factor. The possible explanations for this could be: a) only 11 of the 60 patients had a PaO2 less than 60 mmHg and b) the mean duration of the disease before admission was 11 days. To conclude, our study points out that hypoxemia at presentation is associated with onset of cardiac and renal failure during the course of the illness and predicts a poor outcome. The presence of pleural effusion at admission, but not atelectasis and consolidation, correlates with the development of respiratory failure and mortality. Among the respiratory complications which develop during the course of acute pancreatitis, consolidation and ARDS correlates with respiratory failure while ARDS alone leads to poor survival.