Keywords
Partograph; Knowledge; Utilization; Obstetric care givers; Sidama zone; Ethiopia
Abbreviations
AOR: Adjusted Odds Ratio; B.Sc.: Bachelor of Science; EDHS: Ethiopia Demographic and Health Survey; HEWs: Health Extension Workers; HSDP: Health Sector Development Program; MCH: Maternal and Child Health; RHB: Regional Health Bureau; SNNPR: Southern Nations Nationalities and Peoples Region; SPSS: Statistical Package For Social Science
Background
According to World Health Organization (WHO) reports, globally there were an estimated 303,000 maternal deaths occurred in 2015 yielding overall maternal deaths 216 per 100,000 live births. Developing countries accounts the vast majority (99%) of total maternal death; more than one third (66%) of global maternal death occurred in sub-Saharan Africa alone which become 546 per 100,000 live births [1]. In Ethiopia, maternal death is still high it is estimated 412 per 100,000 live births [2].
Eighty-five percent of deaths can be prevented with skilled delivery care before, during, and after childbirth. Because, these deaths are due to five major complications of pregnancy such as: hemorrhage, infection, unsafe abortion, hypertensive disorders of pregnancy, and obstructed labor. Besides, prolonged labor is a most important cause of death among mothers and new-borns in developing countries that in turn, leads the woman to face serious complication related to obstructed labor, dehydration, exhaustion, or rupture of the uterus and infection. Obstructed labor also other most common cause of maternal death in developing world.
Partograph is an economical tool designed to provide a continuous pictorial overview of labour and has been shown to improve outcomes when used to monitor and manage labour. Because, it includes all important information about progress of labour, fetal condition and maternal condition. Also it helps anticipate deviation from normal progress of labour, and supports timely and proven intervention; and facilitates responsibility to the person who is conducting labour; prevent prolonged labour, obstructed labor and related complications, contribute in reduction of majority of maternal and neonatal deaths [1]. Besides, it promotes reduction of prolonged labour by 41%, oxytocin augmentation by 54%, emergency caesarean sections by 3% and rate of vaginal examinations which led to reduced rates of sepsis. Thus, significant number of the study participants reported that the partograph is useful to monitor labor and make timely decision [3]. Despite its huge benefit and the WHO’s recommendation that the partograph should be used to monitor all laboring mothers; it is still not widely used in in the developing world, especially Africa due to different factors [4].
A study conduct elsewhere showed that only 8.4% respondents were utilizing partograph for monitoring labour [5]. In contrast, in a study conducted on knowledge and utilization of partograph among obstetric care givers in public health institutions of Addis Ababa more than 50% of the obstetric care givers utilized partograph for monitoring of labour [6]. Another, Study conducted in Amhara region on utilization of partograph revealed only 29% of the paragraph papers reviewed was properly filled to monitor the progress of labor [3].
In addition, Ugandan Study conducted on assessment of partograph during labour identified that among 1674 deliveries across all the health facility not more than 2% fetal heart beat were recorded on the partograph according to the protocol. In addition, 43.9% of the cervical dilation and 23.6% of uterine contractions monitored were plotted on the partograph as recommended to standard. Eighteen percent of blood pressures were monitored to standard [7]. Another study done in Addis Ababa shows completion of the partograph was very low. Only 30.7% fetal heartbeat, 32.9% of cervical dilatation and 20.70% of uterine contractions plots according to the protocol and only18.6% of maternal blood pressure was recorded based on the standard. The utilization of the partograph was significantly higher among obstetric care givers working in health centers compared to those working in hospitals [6].
Poor knowledge about partograph and its use is one of major factors. Study of Amhara region showed that level of knowledge of birth care providers about the partograph and its components was generally poor [3]. Besides, practitioners’ inadequate or no knowledge on the partograph, inaccessibility of the instrument in labor ward, and shortage of staff have negative influence on utilization of partograph [5]. In study conduct elsewhere, only 16.0%, 7.6% and 10.9% know at least one component of partograph, correctly, explained about function of the alert line and the function of the action line respectively [5].
In study conducted in Addis Ababa however, almost all (96.6%) of respondent were correctly mentioned at least one component of the partograph, 53.3% correctly give explanation about function of alert line and 82.6% correctly explained the function of action line [6].
Besides, shortage of the tool has its own contribution, study of south western Nigeria, conducted on utilization of the partograph in different level of health care facilities shows that only 9.1% of care providers reported that, they have an access to partograph in labour ward [5].
In SNNPR, the proportion of health care workers who are using the partograph as well as their knowledge and other factors are not yet studied very well. So this study conducted to provide a starting point and baseline for the region in order to study the utilization of partograph.
Materials and Methods
Study area
A facility based cross-sectional study was conducted from May, 2016 in Sidama zone, Southern Nations Nationalities and Peoples Region. The zone is located in the North-East part of Ethiopia and bordered with Oromiya in North-east, Wolayita in the West, Gedeo in the south. The zone is one of the most populous areas of the region with population density of 497 persons/km2. It is divided into 19 woredas and 4 city administrations. There are 127 government health centers, 7 primary hospitals and 1 general hospital, 524 health posts, 83 private clinics and 8 NGOs clinic. Recently, the number of health professionals working in public health facilities is estimated to be, 51 medical doctors (general practitioners and specialists), 258 health officers, 1858 nurses, 277 midwives and 1095 health extension workers.
Population
All obstetric care givers of public health institutions in Sidama Zone were considered as source population, and all obstetric care givers of public health institutions in the selected Woredas were study population.
Sampling method
The required sample size of eligible participants for the study were determined using a single population proportion formula n0= (Z1-α* P (1-P)/d2), with assumptions of 95% probability of obtaining the population proportion of staffs who had good knowledge of the partograph, that is 29.3% Amhara region and a 5% margin of error. We used correction formula nf=ni/ (1+ni/N) for finite population (N<10,000) and added 5% of nonrespondent rate and obtained a total of 300 study subjects.
Sampling technique/procedure
The required sample size of eligible participants for the study was determined using WHO research guideline 2013 that allows using 30% of the study area. Based on this we used simple random sampling technique, to select 6 districts including: Aleta wondo, Bensa, Hawassa Zuria, Dale and Chire and Yirgalem city administration from 19 woredas and 2 city administrations in the zones. We compromised all birth care providers working in all health facilities (health centers and hospitals) of the selected woredas. Thus, all professionals who are providing obstetric care in public health facilities of all selected woredas were interviewed. The study includes midwives, nurses and public health officers.
Data collection procedure
A pre-tested and structured, interviewer administered questionnaire was adapted from previous studies and reviewing relevant literature to the problem under study to include all the possible variables that address the objective of the study. Socio demographic factors, update training, years of experience, Professional qualification, and the presence of partograph chart, presence of supervision, number of staffs and number of deliveries per day were variables of the study. The questionnaire was designed to obtain information on the characteristics of staff awareness on partograph, main source of knowledge of the partograph, its benefit and whether or not they routinely utilized it in labour management and proper utilization. The data collected by 10 senior midwives who are working out of selected woredas after intensive training by principal investigators. The respondents’ level of knowledge of the partograph was rated as having minimum score: 0; maximum score: 34 and Scores, 0-10, poor level of Knowledge; 11-20, fair level of knowledge; 21-34: good level of knowledge.
Data quality control
The questionnaire was structured. Close supervision was carried out by the investigators through day to day during data collection, and all incomplete data were identified and corrections was made immediately. Every data was cleaned, coded before entrance into SPSS version 20 computer program.
Data analysis
Raw data was entered and cleaned in SPSS version 20. Frequency distributions and cross tabulations were used to describe the variables of the study. The relationship between independent variables and the respondents ‘utilization of partograph and level of knowledge was explored using bivariate and multivariate logistic regression analysis. Observed differences between samples were considered statistically significant where the confidence limits did not embrace unity or p<0.05.
Ethical consideration
The proposal was submitted to Regional health bureau for Ethical Approval Permission. To conduct the study consent were obtained from Sidama zone Health Department and selected health institutions. The objective of the study was explained and informed oral consent were obtained from each study subject. Participation was entirely voluntary; the participant was given the right to refuse the study. Confidentiality of the information was assured and privacy of the respondent was maintained. Questioners were coded and kept anonymous. Finally, the participants were thanked for their participation.
Results
Characteristics of the interviewed obstetric care givers
Among 300 participants involved in study, 280 were correctly responded the questionnaires making response rate of 93.3%. The majority of the respondents were in the age range of 20-29 years 253 (90.3%) followed by 30-39 years of age 23 (8.2%). The respondents comprised of 81(28.9%) midwives, 168 (60%) nurses, 31 (11.1%) public health officers. 265 (94.6%) of the respondents were from health centers and only 15 (5.4%) were from hospitals. In hospitals majority of the MCH staffs were midwives 12 (80%) while the majority of health center staffs were nurses 168 (63.4%). Most of the participants were diploma 229 (81.8%) and 51 (18.2%) of them were B.Sc. The years of experience of the participants shows majority 173 (61.8%) serves for 3 and more years and 33 (11.8%) serves for less than a year (Tables 1 and 2).
| Variables |
No |
% |
| Age in years |
|
|
| 20-29 |
253 |
90.3 |
| 30-39 |
23 |
8.2 |
| >= 40 |
4 |
2.0 |
| Sex |
|
|
| Female |
152 |
54.3 |
| Male |
128 |
45.7 |
| Education |
|
|
| Diploma |
229 |
81.8 |
| BSc and above |
51 |
18.2 |
| Profession |
|
|
| Nurse |
168 |
60
28.9 |
| Midwife |
81 |
28.9 |
| Public health officer |
31 |
11.1 |
Table 1: Socio-demographic characteristics of study participants, Sidama zone, SNNPR, Ethiopia 2017.
| Variables |
Number |
% |
| Total year of service |
|
|
| <1year |
33 |
11.8 |
| years |
74 |
26.4 |
| >=3 years |
173 |
61.8 |
| Type of facility currently working in |
|
|
| Health center |
265 |
94.6 |
| Hospital |
15 |
5.4 |
| Adequacy of staff explained by the respondents |
|
|
| Yes |
199 |
71.1 |
| No |
81 |
28.9 |
| No of Midwives working in MCH |
|
|
| 0-2 |
156 |
55.7 |
| 3-6 |
117 |
41.8 |
| 15-18 |
7 |
2.5 |
Table 2: Background factors of the respondents in Sidama zone, SNNPR, Ethiopia 2017.
Awareness and knowledge of the partograph among obstetric care givers
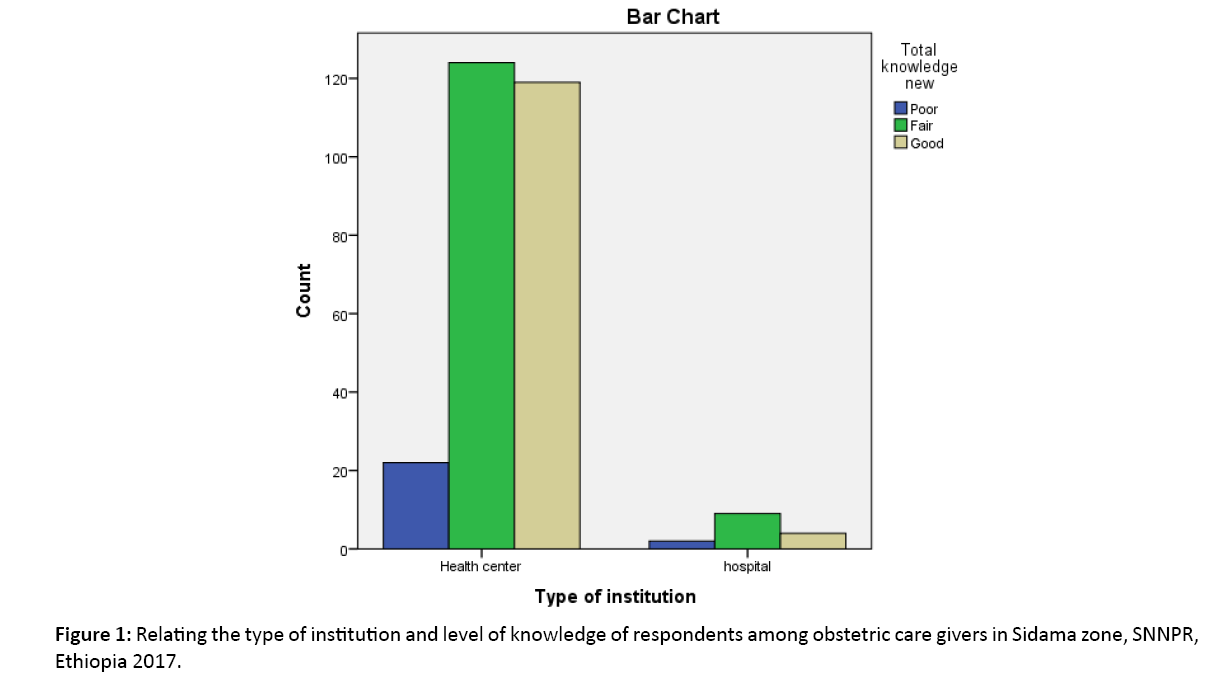
To assess the level of knowledge and utilization of partograph 34 questions were asked and computed. The respondent’s level of knowledge of the partograph was rated as if, 0-11=poor level of Knowledge; 12-22=fair level of knowledge; and 23- 34 good level of knowledge. One hundred thirty three (47.5%) of respondents had fair knowledge, while 123 (43.9%) of them had good knowledge of it and 24 (8.6%) had poor knowledge of partograph. Nearly half of respondents (46.8%) from health centers have fair level of knowledge compared with (60%) respondents from hospitals. From the health centers 8.3% had poor level of knowledge and in hospitals there 13.3% respondent observed with poor knowledge (Figure 1).
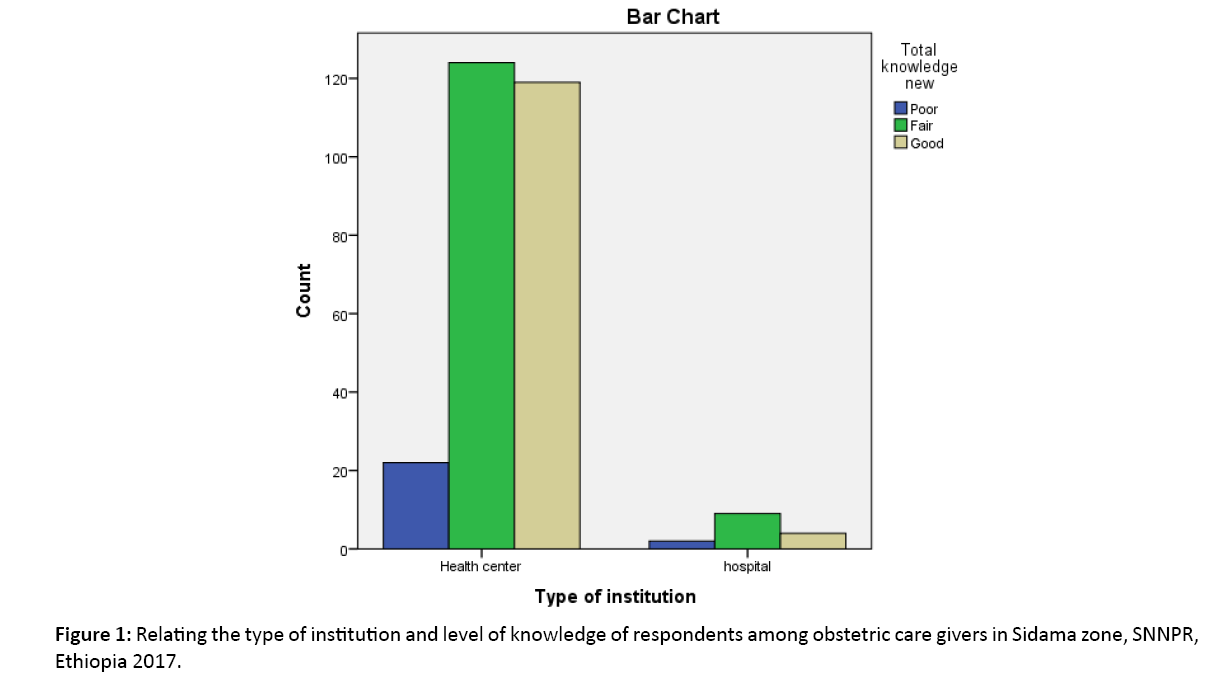
Figure 1: Relating the type of institution and level of knowledge of respondents among obstetric care givers in Sidama zone, SNNPR, Ethiopia 2017.
Majority 264 (94.3%) respondents knew what a parthograph is. Of those who knew what a parthograph is 164 (58.6%) respondents knew its correct definition. Knowledge of respondents on function of both alert line and action line was poor. Only 120 (42.9%) and 154 (55%) respondents could correctly explain the function of alert line and action line, respectively.
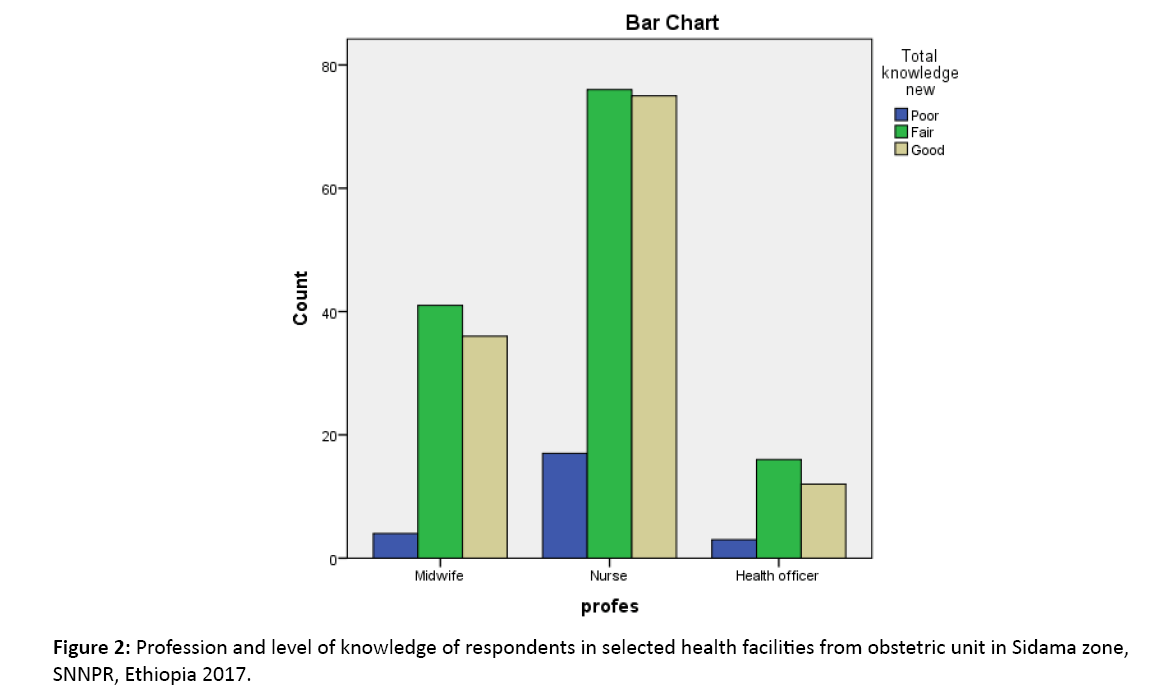
Only 9.7% of the public health officers had good level of knowledge while (29.3%) of the midwives were rated as having good level of knowledge and the majority (60.9%) of the nurses were rated as having good level of knowledge (Figure 2).
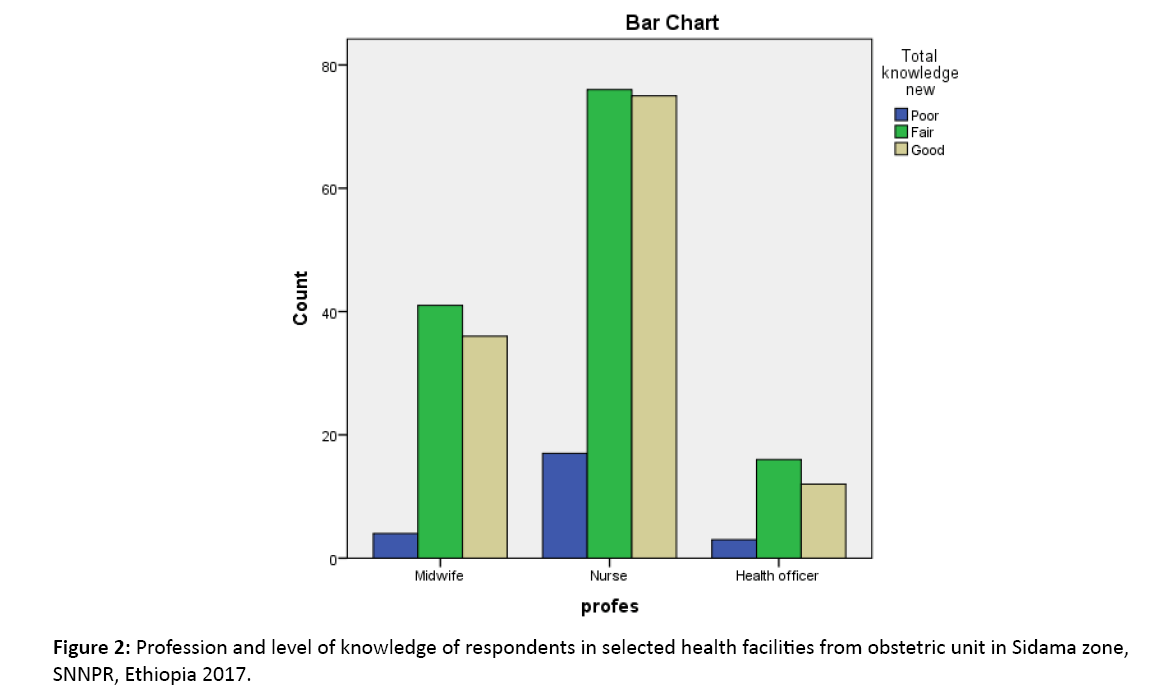
Figure 2: Profession and level of knowledge of respondents in selected health facilities from obstetric unit in Sidama zone, SNNPR, Ethiopia 2017.
Knowledge of respondents on frequency of recording observation on the parthograph shows: 213 (76%) for cervical dilatation, 197 (70.35%) for fetal heartbeat, 175 (62.5%) for molding, 160 (57%) for contraction, 177 (63.2%) for descent, 136 (48.57%) for maternal BP, 180 (64.2%) for amniotic fluid, 102 (36.4%) for urinalysis, 145 (51.78%) for temperature and 177 (43.2%) correctly mentioned the frequency of recording the observations.
Utilization of partograph
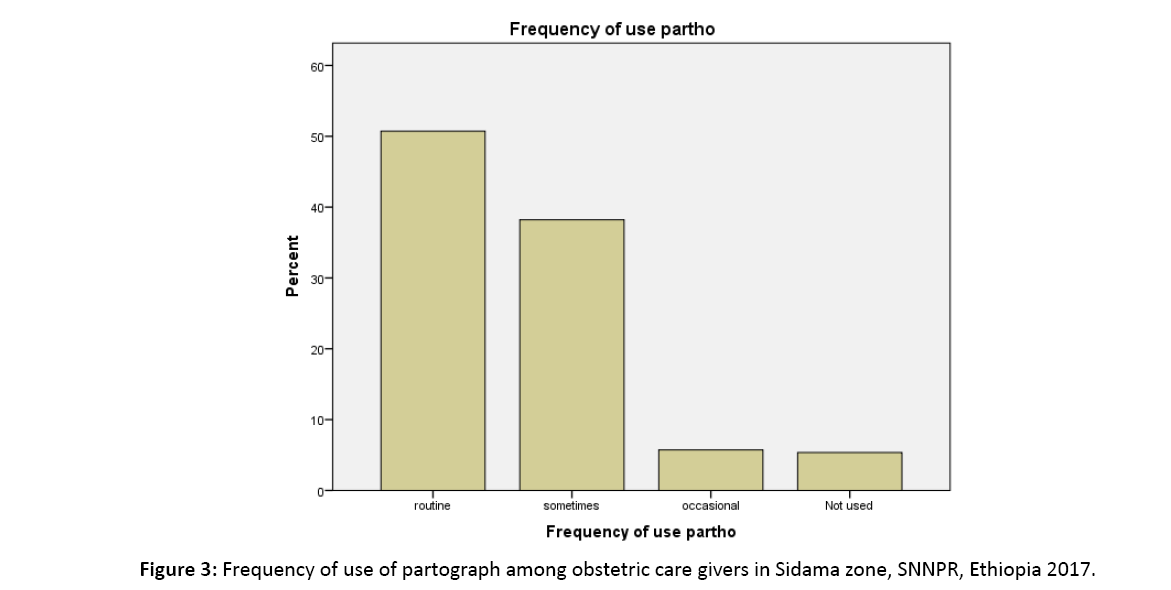
However, most 275 (98.2%) of the respondents said partograph is available in their health facility, nearly half of them 142 (50.7%) uses it routinely, 107 (38.2%) used sometimes and 16 (5.7%) used partograph occasionally (Figure 3). Almost all of the staffs from hospitals were used partograph and 63.9% of respondents were using it in health centers. The presence of training in the use of partograph was assessed. Hundred one (38.1%) of participants had training on use of partograph while the majority 164 (61.8%) used partograph without training. Fifty eight percent of midwives and only 43.4% of the nurses’ used partograph routinely.
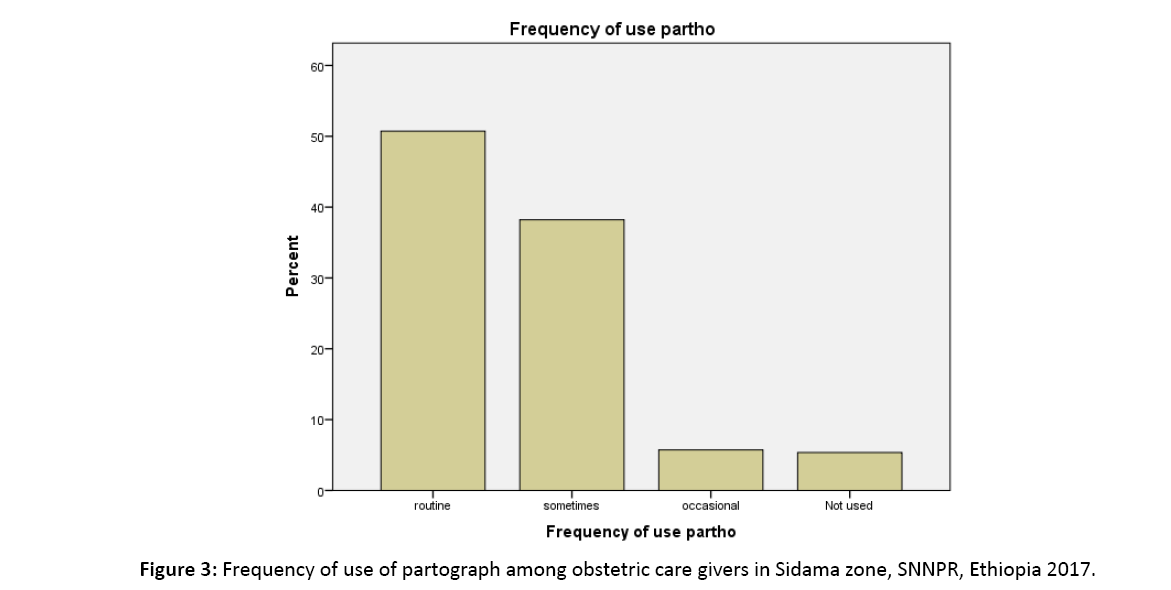
Figure 3: Frequency of use of partograph among obstetric care givers in Sidama zone, SNNPR, Ethiopia 2017.
Reasons for non-using partograph
We considered that respondents who used partograph routinely as users. The rest 138 (49.3%) not used it for monitoring of labour with the reasons for not using it were cited as little or no knowledge and skill of the partograph 93 (67.4%), 33 (23.9%) reasoned absence of partograph, and the rest (8.7%) said due to heavy work load.
On bivariate analysis level of education, years of experience and availability of partograph found to be significantly associated with over all knowledge of partograph. This association also remained significant in the multivariate analysis. When the years of experience increased knowledge of the respondents reduced (AOR= 0.25 (0.11-0.6)) with p-value of 0.02. Level of education also significantly associated. Diploma graduated have 3.7 times have good level of knowledge compared with B.Sc. with (AOR=3.7 (1.23-11.33)). The other variable with significant association was availability of partograph in the specific health facility. Respondents who said they have adequate partograph in their health institution 2.8 times had good level of knowledge compared with inadequate availability of partograph with (AOR=2.8 (1.4-5.5)).
Even if sex, profession, type of institution, training on partograph, use of partograph, and frequency of use of partograph seen no significantly associated with over all knowledge of partograph found in the study (Table 3).
| Variables |
|
Overall Knowledge of parthograph |
Good |
Crude OR (95% CI) |
Crude OR (95% CI) |
| |
|
Poor |
Good |
|
|
| Sex |
Male |
76 |
52 |
Ref. |
|
| |
Female |
81 |
71 |
0.78 (0.48- 1.25) |
1.57 (0.84- 2.9) |
| Education |
BSc |
35 |
16 |
Ref. |
|
| |
Diploma |
122 |
107 |
0.52 (0.27- 0.99)* |
3.7 (1.23- 11.33)* |
| Profession |
Public health officer |
19 |
12 |
Ref. |
|
| |
Nurse |
93 |
75 |
0.66(0.5- 1.25) |
0.3 (0.07- 1.3) |
| |
Midwife |
45 |
36 |
0.9 (0.66- 1.36) |
0.4 (0.11- 1.48) |
| Institution |
Hospital |
11 |
4 |
Ref. |
|
| |
Health center |
146 |
119 |
0.44 (0.13- 1.44) |
0.9 (0.25- 3.9) |
| Experience |
<1 year |
|
|
|
|
| |
1-2 years |
45 |
29 |
0.66 (0.47- 0.94)* |
0.25 (0.11- 0.6)* |
| |
>2 years |
102 |
71 |
|
|
| |
No |
105 |
68 |
Ref. |
|
| |
Yes |
52 |
55 |
1.76 (0.98- 3.15) |
1.5 (0.85- 2.63) |
| |
No |
10 |
5 |
Ref. |
|
| |
Yes |
147 |
118 |
1.6 (0.53- 4.82) |
3.25 (0.62- 17.1) |
| |
Not used |
10 |
5 |
Ref. |
|
| |
Sometimes |
47 |
60 |
0.78 (0.36- 1.68) |
0.75 (0.23 – 2.46) |
| |
Occasionally |
9 |
7 |
|
|
| |
Routinely |
91 |
51 |
|
|
Adequate
availability of partograph |
No |
59 |
22 |
Ref. |
|
| |
Yes |
98 |
101 |
2.76 (1.57- 4.85)* |
2.8 (1.4- 5.5)* |
Note: * Statistically significant at P-value <0.05, 95% CI
Table 3: Bivariate and multivariate analysis of factors associated with overall knowledge of respondents in Sidama zone, SNNPR, Ethiopia 2017.
In contrast, in bivariate and multivariate analysis of routine use of partograph related with sex, level of education, profession, years of experience, availability of partograph, training of partograph and over all knowledge, but there is no statically significant association found.
Discussion
This study focused on magnitude of partograph use and its associated factors among obstetric care providers in public health institutions. Findings from the survey may therefore be regarded as a window that provides a glimpse into current obstetric care practice within the study area.
In this study, majority 264 (94.3%) respondents know what a partograph is and less than half of the respondents 133 (47.5%) had fair knowledge of the partograph and 123 (43.9%) of them had good knowledge of it. But use partograph needs complete knowledge how to identify abnormalities of labour, so respondents who had fair knowledge mean they do not have adequate knowledge to use it. So we can say majority 56.1% of respondents had poor level of knowledge. This finding is somewhat comparable with the study done in Nigeria, in which more than half of the respondents had fair knowledge of the parthograph, while less than one-third of them had a good knowledge [8]. High figure observed compared with the study from Port Said and Islamiyah cities in which most of the participants were nurses and physicians, where 97.1% had unsatisfactory score, while in our study midwifes and health officers were included and physicians excluded. Our finding is lower while compared with a study from Addis Ababa in which 96.6% had fair level of knowledge [6,9]. This result implies that knowledge of obstetric care givers on parthograph may be inadequate for better utilization.
In this study, not only a few respondents had fair knowledge of the partograph, but also there was poor utilization of it in labour monitoring considering the WHO recommendation for parthograph use in public health institutions. Several similar studies confirmed the low utilization of the partograph in Africa [3,5,10,11]. Skilled management of labor using a parthograph, a simple chart for recording information about the progress of labor and the condition of a woman and her baby during labor, is key to the appropriate prevention and treatment of prolonged labor and its complications. Following the recommendation of the World Health Organization (WHO), the Maternal and Neonatal Health (MNH) Program promotes the use of the partograph to improve the management of labor and to support decision-making regarding interventions [1]. When used appropriately, the parthograph helps providers identify prolonged labor and know when to take appropriate actions [8,12]. This necessitates the need for regular pre-service and on-job training of obstetric care givers on use of the parthograph for safety of women in labour [13].
In this study, over all knowledge of participants has statistically significant relationship to years of service of the study participants as obstetric caregivers (AOR=0.25 (0.11- 0.6)). This finding shows the more the participant’s year of experience increase, the knowledge of parthograph reduced. This points the need of periodic on job refresher trainings on the use of partograph because, training on parthograph reduced with increasing service year (32.2%) for those who serves 3 and more years where as the rest chance was given for those with less than two years of experience. This finding is contradicting from the study which had non-significant association between knowledge and years of experience with (AOR=0.87, CI (0.44, 1.74) [10]. On the other hand it can be due to fresh graduates may have in school knowledge and skill used after graduation for some time and utilization may be reduced because of absence of on-job training, burning out due to work overload and low incentives. This is also consistent with the study in Addis Ababa which University/college was reported as a primary source of knowledge by the majority 92 (53.2%) of those who were aware of the partograph and almost all of these individuals had fair and good level of knowledge [6]. In such endeavours, obstetric care givers with longer years of service should not be overlooked assuming that their accumulated experience would enable them to better make use of the partograph.
Level of education also associated where diploma graduates had good level of knowledge 3.7 times compared with B.Sc. with (AOR=3.7 (1.23-11.33)).This study is contradicts with the study in Addis Ababa, where nurses compared to medical doctors had a lesser likelihood of having a good level of knowledge about the partograph (AOR=0.07 (95% CI: 0.02, 0.31)).The difference may be resulted because of the composition of the respondents where nurses, midwifes and health officers are included in our study whereas nurses and physician compared in the study from Addis Ababa. But the study somewhat similar with the finding from South west Nigeria where the physicians had good level of knowledge about partograph compared with nurses [5]. The difference with the Nigerian study can be: physicians are compared but not health officers and there can be difference in the method of training about partograph.
This study also revealed that 94.8% of the respondents not received in-service training on the partograph of who utilized in monitoring of women in labour. Even if training has no statistical significant association other studies show its association which implies that the pre-service training alone is not enough to effectively make use of the partograph in practice (WHO, UNICEF, UNFPA and the World Bank, 2015). In this study only 61.3% filled the partograph and all of them were incomplete. The finding is somewhat consistent with study in Uganda in which 69.9% was used partograph in of deliveries but higher than that of South west Nigeria study, in which only 8.4% respondents were utilizing partograph for monitoring labour [1,5,6,14].
Conclusion
More than half of obstetric care givers in public health institutions of Sidama zone have poor level of knowledge on partograph which shows poor knowledge on the components of partograph and interpretation of the observations. More than half of the obstetric care givers reported that they used the partograph to monitor mothers in labour. The level of knowledge is significantly associated with level of education, years of experience and availability of partograph in their health institution. Over all knowledge of respondents were not associated with sex, profession, presence of training, number of staffs and type of institution and use of partograph. Routine use of partograph is observed in professional’s sex, education, profession, type of institution, years of experience, training of partograph and availability of partograph have no significant association with use of partograph and overall knowledge of respondents. We concluded that professionals worked in Sidama zone not use partograph to follow progress of labour despite their level of knowledge.
Recommendations
Strong supportive supervision, staff motivation, access to library and internet for the staffs, increase availability of partograph and in service training, assigning adequate midwifes (at least 2 per each) in the health facilities and further study (mixed) to identify barriers of utilization of partograph are recommended.
Acknowledgment
First of all we would like to thank Hawassa College of Health Sciences for funding to the study. We would like to extend our sincere gratitude to Mr. Telto Ando technical support throughout the study. We would also like to extend our respectful acknowledgment and gratitude to research internal review committee, all staff of RHB. Finally, special respectful thanks to the study participants, data collectors, and all others who helped us in data entry and analysis.
References
- World Health Organization (2015) Trends in Maternal Mortality?: 1990 to 2015. Geneva, Switzerland.
- Central Statistical Agency (2016) Federal Democratic Republic of Ethiopia - Demographic and Health Survey: Key Indicators Report. Addis Ababa, Ethiopia.
- Abebe F, Birhanu D, Awoke W, Ejigu T (2013) ‘Assessment of knowledge and utilization of the partograph among health professionals in Amhara region, Ethiopia’. SJCM. 2:26-41.
- Fawole AO, Adekanle DA, Hunyinbo KI (2010) Utilization of the partograph in primary health care facilities in south-western Nigeria. Niger J Clin Pract. 13:200-204.
- Fawole AO HK, DA A (2008) Knowledge and utilization of the partograph among obstetric care givers in South West Nigeria. Afr J Reprod Health.
- Yisma E, Dessalegn B, Astatkie A, Fesseha N (2013) Completion of the modified World Health Organization (WHO) partograph during labour in public health institutions of Addis Ababa, Ethiopia. Reprod Health. 10:1-7.
- Ogwang S, Karyabakabo ERZ (2009) Assessment of partogram use during labour in Rujumbura health sub district, Uganda. Afr Health Sci. 1:S27-S34.
- Orhue AAE, Aziken ME, Osemwenkha AP (2012) Partograph as a tool for team work management of spontaneous labor. Niger J Clin Pract. 15:1-8.
- Salama NS, Allah IMABD, Heeba MF (2010) The partograph?: Knowledge, attitude and utilization by professional birth attendances in Port-Said and Ismailia cities. Med J Cairo Univ. 78:165-174.
- Yisma E, Dessalegn B, Astatkie A, Fesseha N (2013) Knowledge and utilization of partograph among obstetric care givers in public health institutions. BMC Preg Childbirth. 13:1.
- Rakotonirina JE, Randrianantenainjatovo CH, Edwige BE, Dorasse R, De Dieu J, et al. (2013) Assessment of the use of partographs in the region of Analamanga. Int J Reprod Contracept Obstet Gynecol. 2:257-262.
- Kushwah B, Singh AP, Singh S (2015) The partograph: An essential yet underutilized tool. J Evol Med Dent Sci. 2:4373-4379.
- Mathibe-Neke JM (2009) Facilitation of midwifery students regarding utilisation of a partograph. Afr J Nurs Midwifery. 11:34-47.
- Ogwang S, Karyabakabo Z, Rutebemberwa E (2009) ‘Assessment of partogram use during labour in Rujumbura health sub district, Rukungiri district, Uganda’. Afr Health Sci. 9:27-34.