Case Report - (2022) Volume 8, Issue 4
Management of a Rare Complication after Tension-free Vaginal Tape Surgery: A Case Report
Vivien Szanto* and
Peter M. Fehr
Departement of Gynaecology and Obestetrics, Frauenklinik Fontana, Chur, Switzerland
*Correspondence:
Vivien Szanto, Departement of Gynaecology and Obestetrics, Frauenklinik Fontana,
Lürlibadstrasse 118., 7000 Chur,
Switzerland,
Tel: +41812548125,
Email:
Received: 17-Apr-2022, Manuscript No. IPGOCR-22-12998;
Editor assigned: 19-Apr-2022, Pre QC No. IPGOCR-22-12998 (PQ);
Reviewed: 30-Apr-2022, QC No. IPGOCR-22-12998 (Q);
Revised: 04-May-2022, Manuscript No. IPGOCR-22-12998 (R);
Published:
11-May-2022, DOI: 10.21767/2471-8165.1000017
Abstract
Introduction: Stress urinary incontinence surgery is a common procedure currently using mostly mesh materials,
that is performed around the world. Lately, the debate concerning complications and safety issues began
transforming the landscape of available treatment options worldwide. In our case study, we present a rare longterm
complication, diagnosis and management of transobturator tape surgery.
Case presentation: A 62-year-old caucasian woman underwent transoburator tension free vaginal tape surgery
for stress urinary incontinence 3 months prior in our clinic. She presented with a recurrence of her stress urinary
incontinence after initially being asymptomatic after surgery. We suspected a urethral tape erosion in the perineal
ultrasound and performed a diagnostic cysto-urethroscopy, which confirmed this finding. A transvaginal resection
of the tape was performed with urethroplasty of the posterior urethral wall. After a convalescence period a
retropubic tension free vaginal tape surgery was performed according to the patients wishes. Follow up after 8
months showed correct tape placement and no further stress urinary incontinence.
Conclusion: Transobturator tape surgery remains an effective treatment for stress urinary incontinence with few
intraoperative risks; although in rare cases severe complications can be encountered. A correct diagnosis and
treatment are key in the successful management of displaced mesh material and can lead to long-term patient
satisfaction.
Keywords
Transobturator tape surgery; Stress incontinence; Uro-gynecology; Tape erosion; Case report
Introduction
Stress Urinary Incontinence (SUI) is a very common condition,
affecting up to 50% of women [1] in their lifetime. After failure
of conservative treatment options (physical therapy, pessary) a
mid-urethral sling procedure has been the gold standard surgical
option since its introduction in 1996 [2,3]. In 2008 the US Food and Drug Administration declared complications as common
after surgical mesh implantation in SUI or prolaps surgery [4].
This triggered an international debate which resulted in the
reevaluation of current standards in many countries [5]. It is
therefore important to report on possible complications and
their treatment options.
Case Presentation
Initial referral of our 62-year old patient with Stress Urinary
Incontinence (SUI) through her gynecologist. The patient
was in good health with a body mass index (BMI) of 25.2 kg/
m2, without any prior vaginal or pelvic operations or prolaps.
No history of diabetes mellitus. Urodynamic testing was
performed and the suggested course of treatment was a
transobturator tension-free vaginal tape which was carried
out afterwards. An intraoperative cysto-urethroscopy showed
no signs of intrauretral or intracystic position of the mesh.
The postoperative period was uneventfull without short term
complications and the patient was discharged the same day.
The patient was satisfied and had no urine leakage or other
symptoms for approximately one month after surgery. 3
months later she was referred to our hospital with a gradual
recurrence of the SUI symptoms with leakage during most
physical activities. She didn`t mention any urgency symptoms
or recurring urinary tract infections. She also described a light,
stabbing pain in the distal part of the anterior vaginal wall on
physical exertion. Initial findings showed slightly decreased
vaginal estrogenisation without the presence of a cystocele
or other descensus, no mesh-protrusion into the vagina, the
tape barely palpable on examination. The perineal ultrasound
showed erosion of the mesh into the urethra in the middle
section (Figure 1). Hereafter, a cysto-urethroscopy was
performed under general anaesthesia, which confirmed the
findings of the initial examination with sling material crossing
the posterior urethral wall from 5 to 7 o`clock (Figure 2). The
patient consented to the resection of the tape via transvaginal
approach. We performed a re-incision of the vaginal wall 1
cm below the external urethral orifice and dissection of the
paraurethral space to the left. We located the sling material
and resected it moving from lateral to medial. The posterior
urethral wall was opened in the process, as was to be
expected. We perfomed a complete excision of the tape up
until the paraurethral space on the right side. After removal
of the sling material, the posterior urethral wall was adapted using single sutures and a transurethral catheter was placed.
The catheter was left in place for 14 days. After removal the
patient experienced no voiding dysfunction and the incision
site was healing properly. The patient was still experiencing
stress urinary incontinence and felt her quality of life greatly
compromised. We discussed the possibility of placing another
transoburator or retropubic tape, as well as the use of bulking
agents. According to our patients wishes and her active lifestyle
we opted for a retropubic tape placement and performed the
operation in the usual manor. The intraoperative urethrocystoscopy
showed no irregularities of the urethral mucosa.
There were no further complications after the surgery and
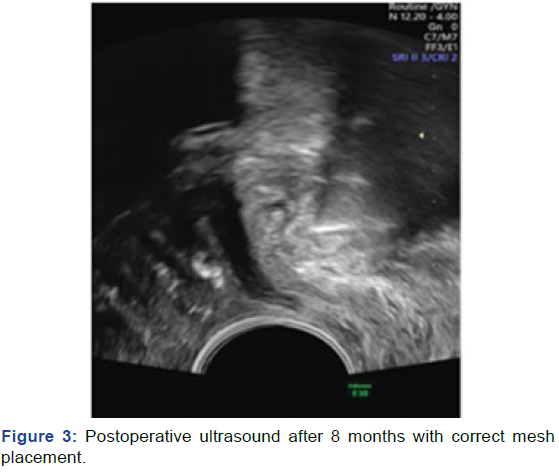
the patient described good continence after 8 months. The
last ultrasound after 8 months (Figure 3) showed perfect tape
placement and the urethral wall intact.

Figure 1: Tape material visible in the urethra in the perineal ultrasound.

Figure 2: Cystoscopic image of displaced tape material in the urethra.
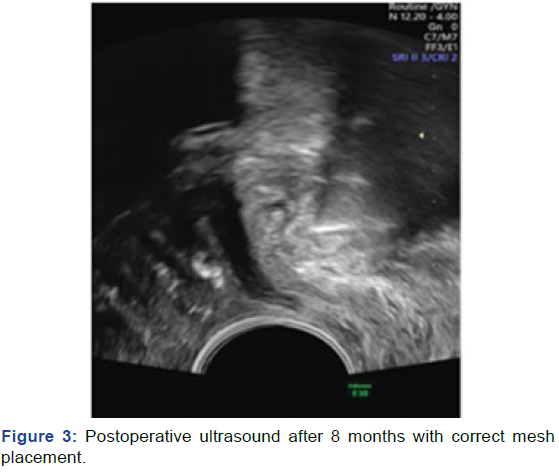
Figure 3: Postoperative ultrasound after 8 months with correct mesh placement.
Discussion
There are a lot of possible complications following the surgical
treatment of SUI, but the incidence rates reported in different
studies are controversial [6]. Among the most common seem to
be postoperative voiding dysfunctions, haematomas, do novo
urgency and persistent SUI [1]. The reported incidence rates
for tape exposure after transobturator tape surgery seem to range from 3.8% to 15% [7]. Urethral erosion of sling material is a rare and serious long term complication following TVT-O
surgery with few cases presented as of date. In literature, a
transurethral mesh excision is described as successful and
less damaging to the urethral tissue [8] than a transvaginal
approach. Sergouintis F, et al. [9] reported a series of 9 cases
with urethral mesh erosion where 5 out of 9 patients didn't
require further SUI surgery after mesh removal. In our case we
opted for a transvaginal resection and urethroplasty because
the patients main complaint was the recurring SUI. Treatment
using a bulking agent was discussed with the patient but
since she led a very active lifestyle and wanted a permanent
solution, we opted for a new mid urethral sling implantation.
In a prospective, randomised noninferiority trial Ikonen FAM,
et al. [10] found that patient satisfaction was significantly lower
1 year after bulking agent than after TVT surgery but the the
complication rate was significantly higher in the TVT group [10].
Our patient was willing to take the risk. Bulking agents seem
to be a feasable option for patients with relative or absolute
contraindications for a repeat TVT surgery, such as neuological
bladder voiding problems, history of oncologic gynaecological
surgery or radiation, as well as contraindications for local or
general anaesthesia [11]. This wasn´t the case with our patient.
Sabadell J, et al. [12] published a retrospective study in 2019 on
the long-term outcomes of retropubic TVT after TVT-O failure
and found it to be an effective alternative, although a more
frequent overall complication rate occured (tape erosions and
de novo urgency). The other main difficulty with tape erosions
seems to be the delay of diagnosis due to a wide range of
possible symptoms and a lack of clearly defined risk factors.
An inexperienced surgical team, presence of cystocele or pelvic
surgery prior to the procedure, as well as a low body mass
index or advanced patient age, diabetes mellitus or tobacco
smoking have been identified as possible predisposing factors
[13]. In our case, none of these were present. An intraoperative
cysto-urethroscopy is recommended, but can't completely rule
out intraurethral mesh material due to restricted visibility or
future displacement after surgery [13].
Conclusion
Urethral mesh erosion after TVT-O surgery is a rare complication.
Displaced material can be resected transurethrally or
transvaginally and mostly resolves symptoms such as vaginal
pain or urgency. At the moment we don't have a universally
accepted treatment option for the recurring SUI. These patients,
as seen in our case, can still be very active and extremely limited
by SUI in their quality of life. Since they already underwent a
surgery for this issue, they are looking for a definitive solution,
which as of now doesn't exist. A de novo sling implantation
initially yields good results with elevated risk of complications
and reoperation and the use of bulking agents usually doesn’t
lead to long term patient satisfaction. With the rise of new and
old surgical procedures foregoing mesh material it is important
to compare long-term results and evaluate safety and patient
satisfaction in the future.
Declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Written informed consent was obtained from the patient for
publication of this case report and any accompanying images. A
copy of the written consent is available for review by the Editorin-
Chief of this journal.
Competing Interests
The authors report no competing interests.
Availability of Data and Materials
Not applicable.
Funding
There was no additional funding involved.
Author Contributions
All authors read and approved the final manuscript.
Acknowledgment
Not applicable.
REFERENCES
- Søgaard NB, Glavind K (2021) Complications and re-operations after tension-free-vaginal tape operation in women with stress urinary incontinence. Int Urogynecol J 32 (1): 159-166.
[Google Scholar], [Crossref], [Indexed at]
- Schimpf MO, Rahn DD, Wheeler TL, Patel M, White AB, et al. (2014) Sling surgery for stress urinary incontinence in women: A systematic review and metaanalysis. Am J Obstes Gynecol 211 (1): 71.e1-71.e27.
[Google Scholar], [Crossref], [Indexed at]
- Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anaesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7: 81-86.
[Google Scholar], [Crossref], [Indexed at]
- Food and drug administration (2008) FDA Public Health Notification: Serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. Public Heal Notiz.
- Chang J, Lee D (2017) Midurethral slings in the mesh litigation era. Trans Adnrol Urol 6 (S2): S68-S75.
[Google Scholar], [Crossref], [Indexed at]
- Barisiene M, Cerniauskiene A, Matulevicius A (2018) Complications and their treatment after midurethral tape implantation using retropubic and transobturator approaches for treatment of female stress urinary incontinence. Videosurg 13 (4): 501-506.
[Google Scholar], [Crossref], [Indexed at]
- Poren M, Constantin E, Frea B, Giannantoni A, Ranzoni S, et al. (2007) Tension-free vaginal tape vs. transobturator tape as surgery for stress urinary incontinence: Results of a multicentre randomized trial. Eur Erol 52 (5): 1481-1491.
[Google Scholar], [Crossref], [Indexed at]
- Wijffels SAM, Elzevier HW, Lycklama a Nijeholt AAB (2009) Transurethral mesh resection after urethral erosion of tension-free vaginal tape: Report of three cases and review of literature. Int Urogynecol J 20: 261-263.
[Google Scholar], [Crossref], [Indexed at]
- Sergouniotis F, Jarlshammar B, Larsson PG (2015) Urethral complications after tension-free vaginal tape procedures: A surgical management case series. World J Nephrol 4(3): 396-405.
[Google Scholar], [Crossref], [Indexed at]
- Ikonen FAM, Mental M, Rahkola-Soisalo P, Tulokas S, Mikkola TS (2020) Tension-free vaginal Tape surgery vs. polyacrylamide hydrogel injection for primary stress urinary incontinence: A Randomized Clinical Trial. J Urol 203: 372-378.
[Google Scholar], [Crossref], [Indexed at]
- Kowalik CR, Casteleijn FM, van Eijndhven HWF, Zwolsman SE, Roovers JWR (2018) Results of an innovative bulking agent in patients with stress urinary incontinence who are not optimal candidates for mid-urethral sling surgery. Neurourol Urodyn 37: 339-345.
[Google Scholar], [Crossref], [Indexed at]
- Sabadell J, Montero-Armengol A, Rodríguez-Mias N, Salicrú S, Gil-Moreno A, et al. (2020) Long-term outcomes of retropubic tension-free vaginal tape for stress urinary incontinence after a transobturator tape failure: A retrospective study. Int Urogynecol J 31: 755-760.
[Google Scholar], [Crossref], [Indexed at]
- Osborn DJ, Dmochowski RR, Harris CJ, Danford JJ, Kaufman MR, et al. (2014) Analysis of patient and technical factors associated with midurethral sling mesh exposure and perforation. Int J Urol 21 (11): 1167-1170.
[Google Scholar], [Crossref], [Indexed at]
Citation: Szanto V, Fehr PM, (2022) Management of a Rare Complication after Tension-free Vaginal Tape Surgery: A Case Report. Gynecol Obstet Case Rep. Vol.8 No.4:17. DOI: 10.21767/2471-8165.1000017
Copyright: © Szanto V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.