Keywords
Waste collectors; Sharp injury; Blood and body fluids; Health facility; Ethiopia.
Background
Health facilities generate different types of wastes which are characterized as hazardous wastes, most of which are toxic, harmful, carcinogenic, and infectious materials [1]. Wastes containing sharp materials may affect not only health workers who produce them, but also waste collectors and laundry personnel who handle and collect them [2].
Medical Waste Collectors (MWCs) faced massive exposure to hazardous wastes and occupational accidents as a result of manual handling of waste and working under unfavorable conditions. These accidents include injuries caused by sharp materials such as hypodermic needles, broken glasses, and hard plastics. This type of injury could represent an infectious pathway for many infectious microorganisms such as hepatitis and HIV [3]. At the same time, these injuries create an unequal burden on the workers in rate greater than those who are working in similar work settings and from the general public. The long term psychological and psychosocial burden due to fear of acquiring infection can also have major impacts on the lives of affected individuals [2].
Waste collectors are at high risk of acquiring disease resulting from exposure to various work hazards [4, 5]. There are studies showing different health complaints such as respiratory problems [6-8], increased risk of hepatitis A and B [9, 10] and skin diseases [11] for people working in waste handling. In addition, self-reported risks including musculoskeletal, fatigue, gastrointestinal, and hearing complaints were also identified [12].
Professional related risk assessment reports showed that waste collectors had the third highest needlestick injury rate (18.4 per 1000 p-y) and the second highest other sharps injury rate (7.1 per 1000 p-y) comparing with healthcare workers [13]. One study showed, each year waste collectors reported 50-100 puncture wounds as a result of collecting medical wastes from private medical practitioners and from the disposal of needles by drug addicts [14]. Waste collectors in Hawasa city of south Ethiopia have reported that they had experienced needle-stick injuries at least once in their life at the different healthcare facilities ranged from 25-100% [15].
Unavailability or shortage of personal protective devices aggravates the risk of acquiring infection while exposed to hazardous wastes. Waste handlers usually do not wear sufficient protective clothing [1, 16] and heavy protective gloves [17, 18] during waste handling which increases the potential risk of accidents. A study in Bangladesh capital Dhaka showed that 73% of waste collectors working in health facilities studied did not regularly wear sufficient Personal Protective Equipments (PPE) during waste handling [19].
Even though the impact of healthcare wastes on healthcare workers is well described globally [20], less attention is given for waste collectors and countrywide official statistical data do not address the health and working condition of waste handlers [13, 21]. In Ethiopia, studies [22, 23] were done in some parts of the country were mainly focused in identifying blood borne pathogens such as hepatitis B and C. As a result, less attention was given to see the overall working conditions and factors exposing waste collectors for possible injuries and accidents.
The impact of improper medical waste management on the health of MWCs is however assumed to be very high because of organizational and personal challenges. At the health facility level, policies, laws and regulations about medical waste management are absent or implicit. At the same time, there is very low attention by health administrators and resource such as budget, material and qualified human resource are poorly allocated. At the individual level, waste collectors are people who are employed without proper trainings for the job had a low level of education and many do not wear personal protective equipment (PPE) [24]. Many did not receive on-job training, did not take any vaccinations before work, had no regular health checks in the workplace and not aware of the hazardousness of the work [20]. Their income is low and living conditions are also very poor, thus further increasing the risk of disease [25].
Though it is known that improperly managed healthcare waste has a direct effect on the health of people in and around the health facilities, quantifying the level of the effect is vital in order for the concerned body to put remedial actions. This study has therefore assessed the working condition and level exposure of waste collectors to sharp injuries and blood and body fluids.
Methods
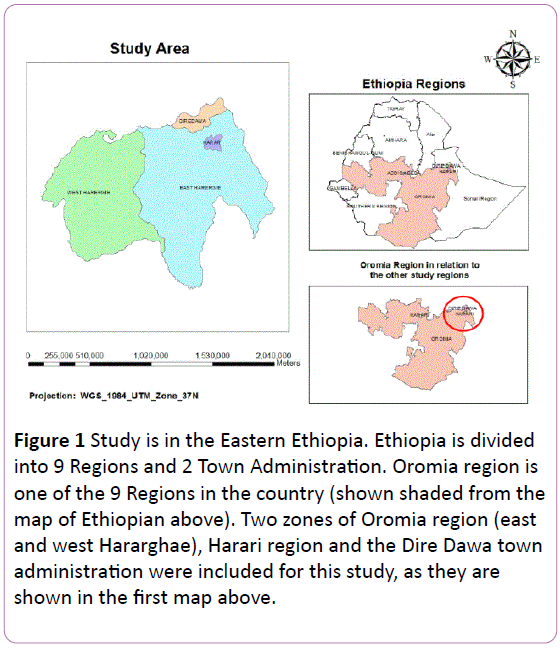
Institutional based cross-sectional study was conducted in Harari Region, Dire Dawa Administration, and east and west Hararghea zones of eastern Ethiopia (Figure 1), from August 2013 to February 2014. According to the data obtained from the respective health offices, there were a total of 195 public health facilities (hospitals and health centers) in the study area and the study was done on 65 (9 hospital and 56 health centers) of them. All the public hospitals in the area were included. For the selection of health centers, a two stage sampling was considered. First, 30% (n=56) of the health centres were considered sufficient to evaluate the impacts of healthcare wastes on waste collectors [26-28]). Second, by probability proportional to population size sampling method, data were taken from 253 MWCs.
After a questionnaire was developed, it was pretested and administered by face-to-face interview method. Ethical clearance was secured from IRB of the College of Health and Medical Sciences of Haramaya University. MWCs were also asked for their willingness to participate to this study and those who refused to participate, their choice was respected. MWCs that reported having exposed to SI and BBF and did nothing were advised to seek medical care.
The dependent variable was either injury by sharp materials or exposure to blood and body fluids. One variable was then created from both exposure statuses and dichotomized into two (yes or no). Data from the questionnaires was stored and coded in a database for subsequent analysis. Data were checked for consistency and completeness, and then analysed using STATA version 12 software. First descriptive statistics was carried out to see the nature of the collected data and factors associated with exposure status of SI and BBF were identified by using multivariable analysis. Clustering effect of the health facilities were controlled during analysis using Generalized Estimating Equations (GEE).
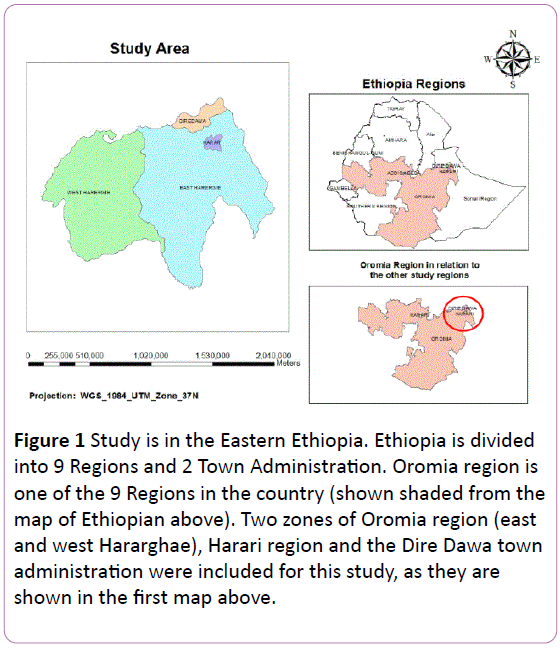
Figure 1: Study is in the Eastern Ethiopia. Ethiopia is divided into 9 Regions and 2 Town Administration. Oromia region is one of the 9 Regions in the country (shown shaded from the map of Ethiopian above). Two zones of Oromia region (east and west Hararghae), Harari region and the Dire Dawa town administration were included for this study, as they are shown in the first map above.
Result
Basic demographic characteristics
The employment profile of the health system showed that the duty for waste collection is reserved for females. As a result, all participants of this study were females. The mean age of respondents was 29.7 ± 11.5 years. Majority, 140 (55.3%), of them were from grade 9-12 and 12 (4.7%) reported they are not educated. Those who are married accounted for 56.9% and Orthodox religion followers were 124 (49.0%). Majority of the waste collectors have less than 10 years’ work experience whereas only 8 (3.3%) served for more than 30 years (Table 1).
| Educational status |
Frequency |
Percent |
| Not educated |
12 |
4.7 |
| Read and write |
4 |
1.6 |
| Grade 1-8 |
77 |
30.4 |
| Grade 9-12 |
140 |
55.3 |
| Diploma and above |
20 |
7.9 |
| Age |
|
|
| 15-24 |
85 |
35.6 |
| 25-34 |
93 |
38.9 |
| 35-44 |
36 |
15.1 |
| 45-54 |
17 |
7.1 |
| 55-64 |
8 |
3.3 |
| Religion |
|
|
| Islam |
108 |
42.7 |
| Orthodox |
124 |
49 |
| Protestant |
19 |
7.5 |
| Others |
2 |
0.8 |
| Marital status |
|
|
| Single |
64 |
25.3 |
| Married |
144 |
56.9 |
| Divorced |
24 |
9.5 |
| Widowed |
21 |
8.3 |
| Service year |
|
|
| 1-9 |
197 |
80.4 |
| 10-19 |
26 |
10.6 |
| 20-29 |
14 |
5.7 |
| 30-39 |
8 |
3.3 |
Table 1: Socio demographic data for healthcare waste collectors in the eastern part of Ethiopia, 2014.
Self-reported health problems
Medical waste collectors were asked to report whether they have a known health problem or not. Though most of them were seen very reluctant in reporting their health problem, as seen during data collection, there were 62 (24.5%) waste collectors complained having a known health problem. Out of these, 17 (27.4%) have frequent headache and 12 (19.4%) have back pain.
Knowledge on the production of wastes on the health facilities and HWM
MWCs in this study were asked to list the type of wastes produced in their work area. It was discovered that out of 249 respondents, only 65 (26.1%) and 18 (7.2%) have reported they knew the production of infectious and sharp wastes respectively. Again, 132 (53.7%) out of 246 knew that there is a law regarding HWM in the country. Where half (50.4%) reported that their health facility practiced waste segregation, 241 (97.6%) believed that there should be wastes separation at the generation point. Regarding the question who should they thought segregate the waste, majority, 172 (68.8%), responded that they themselves should do it (Table 2).
| Questions |
|
Frequency |
Percent |
| Type of wastes |
|
|
|
| General |
Yes |
219 |
87.9 |
| |
No |
30 |
12.1 |
| Infectious |
Yes |
65 |
26.1 |
| |
No |
184 |
73.9 |
| Sharps |
Yes |
18 |
7.2 |
| |
No |
231 |
92.8 |
| Chemical/pharmaceutical |
Yes |
14 |
5.6 |
| |
No |
235 |
94.4 |
| Whom do you believe should do the segregation? |
|
|
|
| |
Myself |
172 |
60.1 |
| |
The nurse |
92 |
32.2 |
| |
Other health personnel |
14 |
4.9 |
| |
I do not know |
8 |
2.8 |
Table 2: Respondents knowledge on the type of healthcare wastes produced and about HWM in the health facilities by medical waste collectors in the eastern Ethiopia, 2014.
Regarding waste containers, 154 (64.4%) replied that there is a distinct color-coded container for storing different type of wastes. Accordingly, MWCs were asked to match wastes and their appropriate coloured container. Accordingly, 174 (72.8%), 204 (85.7%) and 182 (76.8%) have responded yellow bag for infectious waste, yellow box for sharps and brown bag for general wastes respectively.
Attitude of MWCs on the management of healthcare wastes
In order to elucidate further about the healthcare waste management practices at health facilities, the attitude of MWCs was assessed. Their attitude was assessed with six Likert-type questions. As depicted, the attitude questions were analyzed by calculating the mean for each question and then the overall mean (Table 3).
| |
Responses |
Mean |
| Attitude questions |
Strongly agree |
Agree |
Undecided |
Disagree |
Strongly disagree |
|
| wastes management is not the responsibility of the HF |
32 |
42 |
17 |
145 |
|
|
| Waste Management is the duty of all workers |
138 |
86 |
20 |
3 |
1 |
1.56 |
| waste management is the Governments duty |
65 |
130 |
17 |
30 |
7 |
2.13 |
| waste management is a team work |
139 |
80 |
20 |
9 |
0 |
1.59 |
| waste management incur additional budget for HFs |
23 |
114 |
37 |
65 |
12 |
2.72 |
| waste management has additional burden |
10 |
58 |
32 |
137 |
13 |
3.72 |
| Total mean |
|
|
|
|
|
2.5 |
Table 3: Attitudes of medical waste collectors regarding HWM in their health facilities in the eastern Ethiopia, 2014.
Exposure history of MWCs on SI and BBF
In the last one year prior to data collection, there were 75 (30%) waste collector who were exposed to any sharp material while handling medical wastes. The number of waste collectors who were exposed to blood and body fluid were also 121 (43.8%) (Figure 2). Out of those who experienced sharp injury, 69 (85.2%) had needle stick injury whereas lancet and broken glasses were responsible for 4 (5.3%) and 3 (4%) injuries respectively. During observation, data collectors have saw many situations which are liable for the causes of exposure. Wastes are not effectively segregated at the source and used sharp objects including needles are stored with other type of wastes. Needles with syringe were sometimes left in any places including patient side chairs and tables and even on the bed. On the other hand, both hands are the major body parts exposed to sharp injury and blood and body fluids.

Figure 2: Exposure to SI and BBF for MWCs in the last one year preceding the data collection in the eastern Ethiopia, 2014. A bar graph depicts the number of medical waste collectors who were exposed to Sharp Injury (SI) and Blood and Body Fluids (BBF) in one year period. The numbers at the top of the shaded (black) bars indicate the number of MWCs corresponding to their exposure status.
The numbers of MWCs who seek advice from health personnel after injury by sharp objects were 45 (57.7%). On the other hand, only 13 (17.6) of them seek advice after exposed to BBF. During the observation in most health facilities, exposure reports were not found and such event reporting is not practiced. Reporting formats were not found in many of the health facilities. After the incidence, 51 (68%) and 79 (65.2%) medical waste collectors reported taking treatment for the sharp injury and BBF exposure respectively.
Training regarding HWM and personal protective equipments (PPE)
Out of the 248 medical waste collectors, 135 (54.4%) took some kind of training in relation to waste management. However when asked if they need additional training in the future, almost all, 248 (98.8%), replied yes. Regarding personal protective equipments, only 75 (30.1%) reported wearing gown than 235 (95.7%) claiming wearing masks. During observation, however, many waste collectors do not wear gloves and some wore surgical and other types of gloves which do not protect them from injury. Regarding taking vaccines, 144 (59%) have taken at least one type of vaccination and 165 (66.5%) took health check-ups while at work.
Factors affecting exposure to SI and BBF for MWCs
A number of variables were found to be associated with exposure to SI and BBF in a bivariate analysis. Running a final regression with GEE model fitting, variables such as study region, wearing glove, educational status and taking training were remained a predictor for SI and BBF exposure status. Those who are working in Harari and east Hararghae, the odds of having SI and BBF was 0.22 (AOR=0.22, CI=0.1-0.51, p=0.000) and 0.35 (AOR=0.35, CI=0.16-0.78, p=0.01) times lower than those who are working in west Hararghae respectively. And waste collectors who do not wear glove has the odd of getting SI and BBF increases by 3.5 (AOR=3.5, CI=1.17-4.92, p=0.003) than those who are wearing gloves. At the same time, for uneducated waste collector the odd of having SI and BBF exposure increases by 1.5 times higher than the educated ones (AOR=1.55, CI=1.18-2.65, p=0.03). Meanwhile, not taking training about HWM increases the odd of getting SI and BBF by 1.4 times than those who do take training (AOR=1.39, CI=1.27-2.48, p=0.01) (Table 4).
| Parameter |
AOR |
95% Confidence Interval |
P-value |
| |
|
Lower |
Upper |
|
| Working area (region) |
|
|
|
|
| Harari |
0.22 |
0.1 |
0.51 |
0 |
| East Hararghae |
0.35 |
0.16 |
0.78 |
0.01 |
| Dire Dawa |
0.5 |
0.2 |
1.26 |
0.142 |
| West Hararghae |
1 |
|
|
|
| Glove |
|
|
|
|
| Yes |
1 |
|
|
|
| No |
3.54 |
1.17 |
2.92 |
0.003 |
| Educational level |
|
|
|
|
| Educated |
1 |
|
|
|
| Uneducated |
1.55 |
1.18 |
2.65 |
0.03 |
| Training taken |
|
|
|
|
| Yes |
1 |
|
|
|
| No |
1.39 |
1.27 |
2.48 |
0.01 |
| Health problem |
|
|
|
|
| Yes |
2.316 |
1.069 |
5.015 |
0.03 |
| No |
1 |
|
|
|
| Age |
|
|
|
|
| 15-24 |
0.68 |
0.05 |
9.18 |
0.774 |
| 25-34 |
0.76 |
0.06 |
9.81 |
0.83 |
| 35-44 |
0.88 |
0.07 |
10.75 |
0.92 |
| 45-54 |
2.22 |
0.2 |
24.58 |
0.515 |
| 55-60 |
1 |
|
|
|
| Service year |
|
|
|
|
| 1-9 |
0.91 |
0.08 |
10.58 |
0.939 |
| 10-19 |
1.14 |
0.1 |
13.29 |
0.915 |
| 20-29 |
0.82 |
0.09 |
7.72 |
0.859 |
| 30-39 |
1 |
|
|
|
Table 4: Factors predicting the occurrence of SI and BBF among MWCs in eastern Ethiopia, 2014.
Discussion
In the past one year prior to this study, 30% and 43.8% waste collectors were exposed to sharp injury and blood and body fluids respectively. WHO studies showed that up to 5% of all HIV infections in Africa are due to unsafe injections including exposure to sharp injuries during unsafe handling of medical wastes [29, 30]. On the other hand, data from two decades’ studies in Africa estimated that contaminated needles and syringes used for medical treatments led to 48% of the HIV infections and sexual transmission though unprotected sex causes only 30% of the infections [31]. Study in Hawassa city of south Ethiopia showed that MCWs had experienced needle-stick injuries at least once in their life at the different HCFs ranged from 25-100% [15]. Exposure to both SI and BBF will results to acquire blood borne pathogens such as Hepatitis B and C and HIV [32]. Especially this time where Ebola epidemic is becoming a number one public health threat in Africa, medical waste collectors are at a very high risk in such working conditions and there is a need for immediate interventions and critical follow-up by each level of health organizations.
Handling healthcare wastes is a demanding and difficult job that involves working manually without the aid of technologically advanced equipments. There is extraneous physical activity (such as manual lifting of heavy objects like bins and containers with no carts) and exposure to strong weather conditions such as rain, cold, sun light, etc., [14]. Manual handling of heavy containers further expose waste collectors to different musculoskeletal disorder as back bending and unnecessary twisting which are partly attributed by not handling objects firmly because of fear of contamination. In this study, there were several self-reported health problems including respiratory problems, severe headache, repeated common cold and joint, back and abdominal pains. There were also similar reports by waste collectors elsewhere [6, 9-12, 33, 34].
The effectiveness of healthcare waste management (HWM) of any health facility depends on the proper handling of such wastes by health workers, wastes collectors, patients and their relatives. The role of waste collectors is however enormous. Primarily, they should have adequate knowledge about the type of waste produced in the health facility they are working. In this study, medical waste collectors’ knowledge on the production of the types of wastes in their health facilities was low. Though during observation, all type of wastes (general, infectious, sharps and chemical/pharmaceutical) are produced, they have a very poor knowledge on the production of infectious and sharp wastes. On the contrary, their knowledge regarding the type and colour of container used for storing wastes was good. While the National Code [35] clearly stipulates different colour-coded containers for use, only two (yellow for infectious and black for general) are currently used in many health facilities.
The numbers of waste collectors who wore gown and face shield were few. Accordingly, 8 (13.8%) of them experienced face splash with blood and body fluids. The number of waste collectors who reported using gloves (of any kind) was low, 40%. A study in Bangladeshi capital, Dhaka, showed that 73% of waste collector responded that they did not regularly wear personal protective equipment (EPE) during waste handling [19]. PPE such as gloves including puncture- and cut-resistant ballistic gloves for handling raw wastes are not adequately available [17-18, 24]. Further protection equipments such as safety boots or shoes, poly cotton trousers with cut-resistant ballistic pads to the lateral aspect of the lower leg and lower part of the thigh are not provided [24]. These types of protective clothing are highly required for safeguarding waste collectors as there is a high chance of sharp injuries because of indiscriminate disposal of used sharp objects including hypodermic needles by patients, and their relatives and health personnel themselves.
Both hands were the major body parts exposed to SI and BBF. In another study in UK, chest, arms and legs were the common sites for splash contamination and splashes to the face were also familiar [24]. Though sharp materials were stored on puncture-proof containers and this practice further reduces injuries related to handling of medical wastes [36], most of the injuries occurred mostly as a result of overflow of waste bins. In a walk-through survey (observation) it was observed that over flow was a common phenomenon, waste containers were full, they were also stored in corridors and waiting places where patients and their visitor are staying which might obstruct the free movement of patients and their relatives and even medical staff.
Nearly 55% of waste collectors reported they have taken some kind of on job trainings while almost all are still require additional training regarding their job. However, majority of them do not have enough knowledge of the job they are doing and the potential health hazards associated with healthcare waste [15]. The absence of appropriate training before employment might have resulted in improper waste management practices and put waste handlers at a higher health risks. Though 53.7% waste collectors knew the availability of laws regarding wastes management, it was however observed that no manuals and guidelines were found in the health facilities involved, which is similar to other areas in the county [15].
The common response waste collectors gave what they did after injury by sharps and exposure to BBF was seeking advice from health personnel. It was however seen during observation that there is no exposure reporting system and injury reporting formats were not found. Accordingly, there is no appropriate testing for potential blood borne infections such as hepatitis, tetanus and HIV. At the same time, in most health facilities there were no post exposure prophylaxes available [37]. In a similar study in Hawassa town of southern Ethiopia, workers with needlestick injuries didn’t report to the management, were not tested and got treatment for HIV, hepatitis or tetanus [15].
In this study, factors such as working region, utilization of PPE such as glove, taking training and being uneducated were found to be associated with having sharp injury and blood and body fluids exposure. In a similar study in southern Ethiopia, higher percentage of SIs and BBF exposures among MWCs was showed for those only reached to primary school level, recently employed (2-5 years) (p<0.05) [23]. Age of the workers is another important variable but didn’t show any relationship with having SI and BBF exposure in this study. In another study, it was however reported that younger waste collectors reported a higher rate of needle stick injuries whereas experienced ones reported significantly lower rate of needle-related accidents [13-14]. As a result, injury of waste collectors at a young age can have a lifelong negative impact on health, psychosocial and psychological aspects [38]. The difference result in service year may be due to inappropriate age categorization in the current study where majorities (80.4%) were in the age group of 1-9 years’ service year in this study.
One limitation of this study could be reporting exposure is a sensitive issue and because of the use of an interviewed administered questionnaire, wastes collectors might not properly report exposure status. This might underestimate the prevalence of SI and BBF among medical wastes collectors.
Conclusion and Recommendation
Medical waste collectors are working in poor and unfavorable work settings. They are not provided and used appropriate protective equipments such as gloves, aprons, boots, face shields and gown. Knowledge of waste collectors about their work setting starting from identifying the type of wastes produced and the way of protecting themselves from potential hazards is low. Accordingly, exposure to sharp injury and blood and body fluid is high on which they might be at risk of acquiring blood borne infections including hepatitis, tetanus and HIV. The risk will be more sever, if Ebola virus transmits to the country.
A number of measures are proposed in order to safeguard waste collectors from potential hazards. These include adequate training before employment and on job trainings, continuous professional support and supervision and enforcement of rules and regulations which equipped them on how to accomplish their duties in a safe and proper manner. Provision of personal protective devices is an “option less” choice. At last for those who have exposure history, there should be a reporting mechanism, testing, medication and post exposure prophylaxis and establishment of therapeutic centers.
Acknowledgement
Authors of this study would like to thank the respondents for their time and willingness to supply valuable information.
Source of Funding
Haramaya University has provided financial resources for conducting this research.
Ethical Approval
This research has got ethical clearance from IRB of the College of Health and Medical Sciences of Haramaya University.
Conflict of Interest
Authors declare they have no conflict of interest.
Authors’ Contribution
TA was involved during proposal writing, data collection, analysis and writing up. AW’s contribution was during data analysis and writing up whereas NA has participated during data collection, analysis and writing up. All authors read and approved the final manuscript.
References
- Mohamed Soliman S, Ibrahim Ahmed A (2007) Overview of biomedical waste management in selected Governorates in Egypt: A pilot study. Waste Manag 27: 1920-1923.
- Perry J, Jagger J, Parker G, Phillips EK, Gomaa A (2012) Disposal of sharps medical waste in the United States: Impact of recommendations and regulations 1987-2007. Am J Infect Control 40: 354-358.
- Moro PL, Moore A, Balcacer P, Montero A, Diaz D, et al. (2007) Epidemiology of needlesticks and other sharps injuries and injection safety practices in the Dominican Republic. Am J Infect Control 35: 552-559.
- Schibye B, Hansen AF, Søgaard K, Christensen H (2001) Aerobic power and muscle strength among young and elderly workers with and without physically demanding work tasks. Appl Ergon 32: 425-431.
- Wouters IM, Hilhorst SK, Kleppe P, Doekes G, Douwes J, et al. (2002) Upper airway inflammation and respiratory symptoms in domestic waste collectors. Occup Environ Med 59: 106-112.
- Heldal KK, Halstensen AS, Thorn J, Djupesland P, Wouters I, et al. (2003) Upper airway inflammation in waste handlers exposed to bioaerosols. Occup Environ Med 60: 444-450.
- Yang CY, Chang WT, Chuang HY, Tsai SS, Wu TN, et al. (2001) Adverse health effects among household waste collectors in Taiwan. Environ Res 85: 195-199.
- Allmers H, Huber H, Baur X (2000) Two year follow-up of a garbage collector with allergic bronchopulmonary aspergillosis (ABPA). Am J Ind Med 37: 438-442.
- Dounias G, Rachiotis G (2006) Prevalence of hepatitis A virus infection among municipal solid-waste workers. Int J Clin Pract 60: 1432-1436.
- Luksamijarulkul P, Sujirarat D, Charupoonphol P (2008) Risk behaviours, occupational risk and seroprevalence of hepatitis B and A infections among public cleansing workers of Bangkok Metropolis. Hepat Mon 8: 35-40.
- Kuusisto S, Lindroos O, Rantio T, Priha E, Tuhkanen T (2007) PCB contaminated dust on indoor surfaces – health risks and acceptable surface concentrations in residential and occupational settings. Chemosphere 67: 1194-1201.
- Kuijer PPFM (2002) Effectiveness of interventions to reduce workload in refuse collectors. PhD thesis. Coronel Institute for Occupational and Environmental Health, AmCOGG: Center for Research into Health and Health Care, Academic Medical Center/Universiteit van Amsterdam.
- Alamgir H, Cvitkovich Y, Astrakianakis G, Yu S, Yassi A (2008) Needlestick and other potential blood and body fluid exposures among health care workers in British Columbia, Canada. Am J Infect Control 36: 12-21.
- Rachiotis G, Papagiannis D, Markas D, Thanasias E, Dounias G, et al. (2012) Hepatitis B virus infection and waste collection: prevalence, risk factors, and infection pathway. Am J Ind Med 55: 650-655.
- Haylamicheal ID, Dalvie MA, Yirsaw BD, Zegeye HA (2011) Assessing the management of healthcare waste in Hawassa city, Ethiopia. Waste Manag Res 29: 854-862.
- da Silva MC, Fassa AG, Siqueira CE, Kriebel D (2005) World at work: Brazilian ragpickers. Occup Environ Med 62: 736-740.
- Chowdhury AK, Roy T, Faroque AB, Bachar SC, Asaduzzaman M, et al. (2011) A comprehensive situation assessment of injection practices in primary health care hospitals in Bangladesh. BMC Public Health 11: 779.
- Lavoie MC, Yassi A, Bryce E, Fujii R, Logronio M, et al. (2010) International collaboration to protect health workers from infectious diseases in Ecuador. Rev Panam Salud Publica 27: 396-402.
- Patwary MA, O’Hare WT, Sarker MH. Assessment of occupational and environmental safety associated with medical waste disposal in developing countries: A qualitative approach. Safety Science. 2011;49:1200-1207.
- Ruoyan G, Lingzhong X, Huijuan L, Chengchao Z, Jiangjiang H, et al. (2010) Investigation of health care waste management in Binzhou District, China. Waste Manag 30: 246-250.
- Zierold KM, Garman S, Anderson H (2004) Summer work and injury among middle school students, aged 10-14 years. Occup Environ Med 61: 518-522.
- Anagaw B, Shiferaw Y, Anagaw B, Belyhun Y, Erku W, et al. (2012) Seroprevalence of hepatitis B and C viruses among medical waste handlers at Gondar town Health institutions, Northwest Ethiopia. BMC Res Notes 5: 55.
- Shiferaw Y, Abebe T, Mihret A (2011) Hepatitis B virus infection among medical aste handlers in Addis Ababa, Ethiopia. BMC Res Notes 4: 479.
- Blenkharn JI, Odd C (2008) Sharps injuries in healthcare waste handlers. Ann Occup Hyg 52: 281-286.
- Frings-Dresen M (2005) Protecting waste collectors all around the world. Occup Environ Med 62: 820-821.
- Debere MK, Gelaye KA, Alamdo AG, Trifa ZM (2013) Assessment of the health care waste generation rates and its management system in hospitals of Addis Ababa, Ethiopia, 2011. BMC Public Health 13: 28.
- Khajuria A, Kumar A (2007) Assessment of healthcare waste generated by government hospital in Agra city, India. Our Nature 5:25-30.
- Al-Khatib IA, Al-Qaroot YS, Ali-Shtayeh MS (2009) Management of healthcare waste in circumstances of limited resources: a case study in the hospitals of Nablus city, Palestine. Waste Manag Res 27: 305-312.
- Crabb C (2003) Researchers argue that unsafe injections spread HIV more than unsafe sex. Bull World Health Organ 81: 307.
- World Health Organization (2003) Aide memoire for a national strategy for safe and appropriate use of injections. Geneva: Department of Blood Safety and Clinical Technology.
- Gisselquist D, Potterat JJ, Brody S, Vachon F (2003) Let it be sexual: how health care transmission of AIDS in Africa was ignored. Int J STD AIDS 14: 148-161.
- Tarantola A, Abiteboul D, Rachline A (2006) Infection risks accidental exposure to blood or body fluids in health care workers: A review of pathogens transmitted in published cases. Am J Infect Control 34: 367-375.
- rto MA (2007) HIV and related infections in a sample of recyclable waste collectors of Brazil. Int J STD AIDS 18: 653-654.
- Gutberlet J, Baeder AM (2008) Informal recycling and occupational health in Santo André, Brazil. Int J Environ Health Res 18: 1-15.
- The Federal Environmental Protection Authority (2004) Technical Guidelines on the Environmentally Sound Management of Biomedical and Healthcare Wastes, Addis Ababa Ethiopia.
- Mbirimtengerenji N, Schaio J, YGuo L (2012) Association of the dominant hand and needle stick injuries for Healthcare Workers in Taiwan. Malawi Medical Journal 24: 56-60
- Jovic-Vranes A, Jankovic S, Vranes B (2006) Safety practice and professional exposure to blood and blood-containing materials in Serbian health care workers. J Occup Health 48: 377-382.
- Kassouf AL, McKee M, Mossialos E (2001) Early entrance to the job market and its effect on adult health: evidence from Brazil. Health Policy Plan 16: 21-28.