International Exchange - (2003) Volume 11, Issue 4
Public Health Surveillance Officer, NSWCorrections Health Service, Long Bay Correctional Complex, Matraville and School of Public Health and CommunityMedicine, University of New SouthWales, Australia.
Accepted date: August 2003
This paper discusses a model for optimising the screening of prison inmates, and vaccinating them against hepatitis B infection. Hepatitis B and other blood borne infections are common in prison populations worldwide because of previous or current intravenous drug use and unprotected sexual intercourse. Preliminary Ž findings from the implementation of the model described in New SouthWales prison settings highlight its signiŽficant potential for enhancing clinical accountability, as well as improving systems for vaccinating prison inmates. It is however inadequate for optimising sero-conversion, or vaccination follow-up, rates.Such aspects require concurrent adoption of complementary models.
communicable disease, hepatitis B, prison, screening, vaccination
Although the general population of Australia has consistently recorded a low prevalence for hepatitis B carriage (i.e. less than 2%), Australian (and other western) prison settings have a relatively higher carriage.[1] For instance, a 1994 study of 408 New South Wales (NSW) prison inmates reported a prevalence of 31% for hepatitis B core antibody and 3.2% for hepatitis B virus (HBV) surface antigen, comparable to 32% and 2.5%, respectively in a study of 1991/1992 prison entrants to Pentridge Prison, Victoria (Australia). [2,3] In the Victorian cohort, of the 72% (2611/ 3269) for whom immunisation data were available, only 5% (180) reported having ever been immunised. Other Australian groups with similarly high levels of hepatitis B infection are the Aboriginal and Torries Strait Island communities.[4]
Prisons are high-risk environments for the transmission of hepatitis B infection, mainly because of high prevalence of drug use and unsafe sex practices. [5,6] Although published studies on hepatitis B transmission in prisons highlight the need to accord hepatitis B vaccination among prisoners high priority, most correctional centres do not routinely offer vaccination to their incarcerated populations.[7] A reason for this low enthusiasm among custodial authorities might be that there are no major economic incentives accruing to custodial authorities from inmates’ immunisation against hepatitis B.[8]
Fortunately in NSW, there is strong political commitment for inmates to be vaccinated against hepatitis B infection. There are currently 29 NSW prisons in 24 geographically separate sites. According to a recent presentation by the Chief Executive Officer of the NSW Corrections Health Service, the population of inmates in these prisons varies from 50 to about 800, and 94% of the prison population is male. The median age of NSW prisoners is 33, and about 60% have a recent history of injecting drug use. While there were about 7800 prisoners incarcerated at any point in time in 2002, about 21 000 individuals were received into NSWprisons in that year. At 30 June 2002, a total of 19 inmates were serving aggregate sentences of less than 30 days, and 406 were serving aggregate sentences of less than six months.
As at 30 June 2002, NSW had 7793 prison inmates incarcerated, an adult imprisonment rate of 154/ 100 000 (Corben, 2003, personal communication), a 39% increase over figures for 1990.9 In 2002, there were 11 433 persons, and 14 245 receptions into NSW prisons. Of the total number of receptions, only 8501 (60%) were incarcerated for more than 30 days. Such short sentences create additional challenges for effective implementation of hepatitis B vaccination programmes in prison settings.
As with most prison systems, socio-economically marginal individuals are over-represented in the NSW prison population, resulting in a high number of inmates with inferior health status, especially with regard to blood borne viruses.[10,11] Furthermore, a significant proportion of prisoners are engaged in intravenous drug use or unsafe sex practices, thereby increasing their risk of contracting hepatitis B and other blood borne or sexually transmissible infections. Thus, effective hepatitis B vaccination is an important public health intervention for this group. This article describes a model for optimising hepatitis B immunisation programmes in prison settings.
Two policies developed by the NSW Corrections Health Service to address the issues of inmates’ screening and vaccination are the Targeted Screening Programme Policy for Blood Borne and Sexually Transmissible Infections (CHS policy 5.158, June 2002), and the Hepatitis B Screening and Vaccination Policy (CHS policy 1.232, September 2001). These two policies are intertwined since one of the outcomes of the Targeted Screening Programme (TSP) is to determine the number of prison inmates eligible for hepatitis B vaccination.
While these policies detail what should be done with regard to the screening and vaccination of inmates, there is no stated clinical guidance with regard to targets for screening and vaccination. However, such clinical guidance has significant potential for both promoting accountability by vaccination nurses and health managers, and stimulating improvements in systems for hepatitis B vaccination of prisoners. Modelling estimates provide a feasible framework for developing and implementing such clinical guidance. The modelling estimates described in this article are based on a combination of historical trends in reporting of TSP and vaccination activities from prison clinics, trends in inmates’ reception into NSW prisons, and author’s surveys of inmates’ medical records. Table 1 shows the trends in inmates’ enrolment into the TSP and hepatitis B vaccination programme for 2002.
Although data in the table suggest that about 7% of inmates’ daily population count are introduced to the TSP programme monthly (i.e. 544/7793), this proportion is lower than the 11.2% average recorded for 2001, 2000, and 1999. During this preceding period, screening was undertaken under the Voluntary Blood Borne Communicable Diseases Screening Programme, which the more narrowly focused TSP superseded. Hence, the model described is based on the assumption that about 10% of the daily inmate population statewide needs to be introduced to the TSP monthly. As shown in Table 1, about 60% of inmates introduced to the programme monthly are tested for hepatitis B status, as well as other priority diseases; this is similar to the proportion in the previous years.
Based on data from recent monthly reports, as well as surveys in the literature which were recently corroborated by the author through surveys of inmates’ medical records, for every 100 inmates tested, about 35 would have had prior exposure to hepatitis B infection and developed either immunity or a carrier state, while about 40 would not be commenced on vaccination mainly because of short sentences and/or prior vaccination.2,3 Thus, this model estimates that about 25% of inmates tested would be started on the first dose of vaccination. Since the primary course of hepatitis B vaccination consists of three doses over four months, about twoand- a-half times the number of inmates commenced on the initial dose would expectedly be vaccinated monthly.
If this model were applied to trends in screening and hepatitis B vaccination documented for April and May 2003 (figures in parentheses), and using the 30 June 2003 NSW prison census figure of 7904 as baseline, it may be surmised that about 790 inmates would expectedly be introduced to TSP monthly (596, 629). About 60% of those introduced, i.e. 474 (345, 410) would be tested for exposure to blood borne viruses. About 25% of those tested, i.e. 118 (56, 59) would be expected to start on hepatitis B vaccination. About two-and-a-half times the total number of vaccine recipients commenced on vaccination would be vaccinated monthly, using the 0–13 month vaccination regimen, i.e. 296 (161, 172). This model indicates significant performance shortfalls with regard to inmates’ screening and hepatitis B vaccination that need to be addressed statewide.
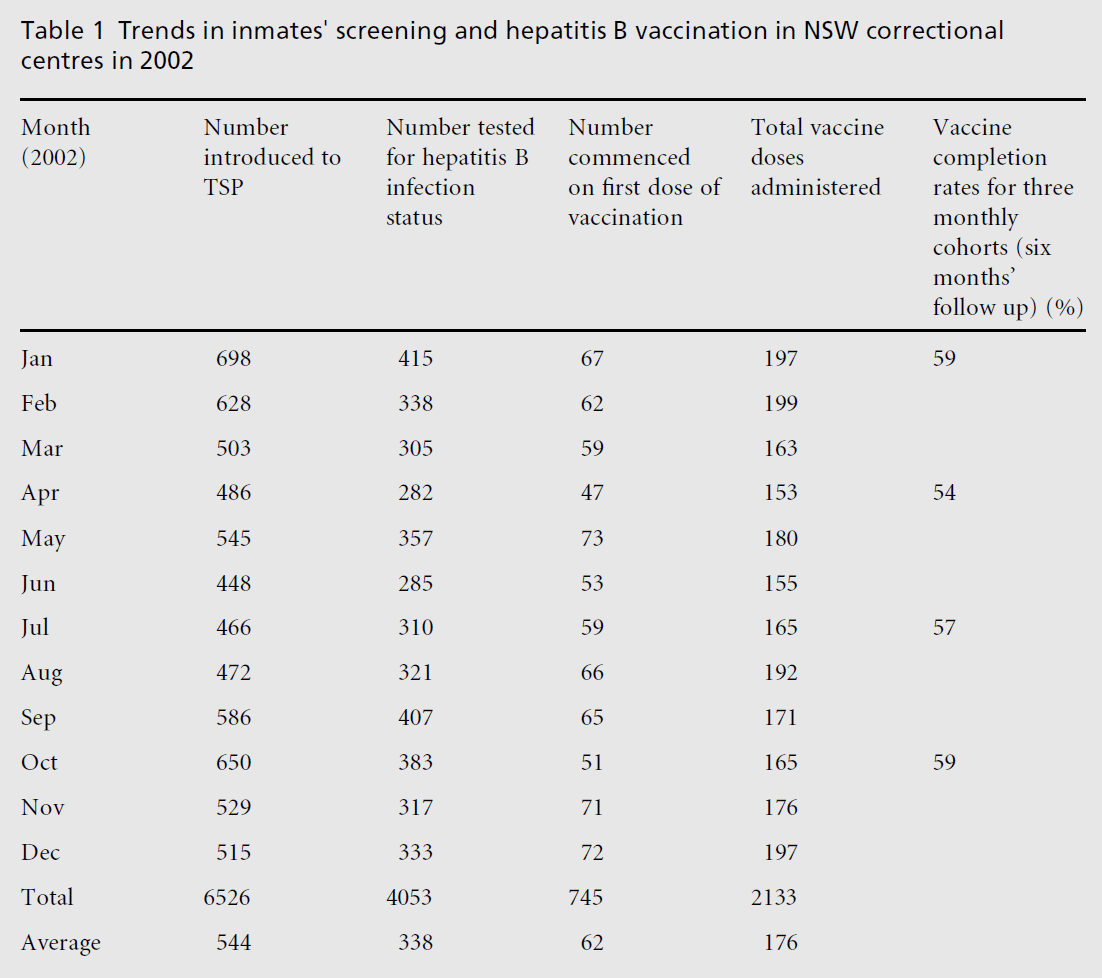
Table 1 :Trends in inmates©screening and hepatitis B vaccination in NSW correctional centres in 2002
This model is currently being applied to trends in each of the 24 NSW prison settings, and has facilitated efforts to address some structural factors impeding vaccination systems at prison clinics, such as improved access to inmates and allocation of adequate nursing hours for screening and vaccination activities. Such efforts have included meetings with custodial authorities to secure regular posting of staff who would escort inmates to clinics for screening and vaccination activities, and advocating for the nursing unit managers to allocate adequate hours for screening and vaccination. A consistent positive feedback received from vaccination staff following the application of the model is that it provides a benchmark by which managers can measure their efforts vis-a‘ -vis the number of inmates vaccinated. Thus, this approach has a potential to promote clinical accountability without being perceived as unduly intrusive.
Clinical governance models such as the one described above have both representational and assessment purposes, providing clinicians and health services managers with insights into inadequacies in programme management, and a picture of possible solutions. The role of modelling in clinical governance and planning includes ideation, prediction, identification, integration, systemisation, and coordination. [12] In prison settings in particular, such a model facilitates clinical accountability among staff in an environment where laxity is rife due to limited avenues for ascertaining clinical accountability by funding agencies and prisoners. The model presents a ‘line of best fit’, around which each prison screening and vaccination trend is expected to coalesce. The ultimate goal, however, should be to obtain aggregate screening and vaccination figures that approximate the model estimates.
Given the potential for significant changes in the variables on which this model is based, its medium to long-term usefulness would be enhanced if it is reviewed yearly, and the variables on which it is based adjusted in response to changing prison policies and/or demographic trends. For instance, given a recidivist rate of about 33% per year among NSW prisoners, effective implementation of this model should significantly reduce the number of inmates eligible for vaccination over the next three years, thus necessitating a change in the estimates of number of prisoners expected to be vaccinated monthly. Also, a proposed (post-election) NSW government policy to minimise the number of inmates incarcerated for less than six months would have a significant impact on the number of inmates introduced to the TSP.
Finally, while this model has been shown to be useful in facilitating improved systems of vaccination, it is inadequate, on its own, for improving vaccination follow-up rates, or facilitating optimal sero-conversion following vaccination. Such aspects of hepatitis B vaccination require additional, complementary, schemas and modelling estimates.[13]
I am indebted to the anonymous referee who reviewed this article for the insightful and constructive comments provided, and to Ms Azar Kariminia for her critique.