Original Article - (2017) Volume 18, Issue 1
Balakumaran Sathyamoorthy1, Sugaprakash Sankareshwaran1, Rajendran Vellaisamy1, Perungo Thirumaraiselvan1, Jeyasudhakar Jesudasan1, John Grifson John Rose1, Heber Anandan2, Kannan Devy Gounder1
Institute of 1Surgical Gastroenterology, Government Rajiv Gandhi General Hospital, Madras Medical College and 2Dr. Agarwal’s Health care Limited, Tamilnadu, India
Received July 10th, 2016 - Accepted September 12th, 2016
Introduction Even though splenectomy is considered as treatment of choice for those with bleeding varices, no consensus has been arrived at regarding management of asymptomatic splenic vein thrombosis while undergoing surgical management for pain in chronic pancreatitis. Objective Whether adding splenectomy while performing surgical procedure for chronic pancreatitis influences the outcome of patients with asymptomatic splenic vein thrombosis is assessed in this retrospective study. Methods splenic vein thrombosis was found in 39 cases among a total of 365 patients (10.7%) operated for chronic pancreatitis between 2009 and 2015. 21 patients underwent splenectomy and 11 underwent only pancreatic procedures and 7 patients are treated with non-surgical management. Bleeding manifestations prior to the surgery were found only in 17 patients. On follow up reduction in size of varices and restoration of flow in splenic vein, rate of rebleeding and morbidity and mortality were analyzed. Median follow-up period was 36 months (Range 10-88 months). Results None of them in the splenctomised patients bleed in the follow up. 4 patients in the non spleenctomised patients developed bleeding in the follow up. 3 patients expired after admission with bleeding manifestations. Another patient developed features of hyperspleenism and required splenectomy in the follow up. None of the factors significantly predicted the risk of bleeding. Conclusion The rate of bleeding is high in surgical population of chronic pancreatitis hence we strongly advise splenectomy as a single stage treatment while performing surgical management of chronic pancreatitis especially in patients with remote access to health care facilities.
Budd-Chiari Syndrome; Hypertension, Portal; Spleenic vein obstruction; Splenectomy
CP chronic pancreatitis; SVO splenic vein thrombosis
Sinestral portal hypertension is a localized form of portal hypertension may complicate chronic pancreatitis as a result of splenic vein thrombosis or obstruction. Splenic vein thrombosis occurs in 10-40% of patients having pancreatitis [1]. The pathogenesis varies with the etiology. Intimal injury and Inflammatory edema in Chronic Calcified Pancreatitis [2, 3, 4] and compression in enlarged pancreatic inflammatory mass or pseudocyst especially in tail region [1] and intimal damage in acute or recurrent episodes of pancreatitis. This obstruction of splenic vein leads to segmental hypertension with diversion of blood flow along Gastroepiploic veins and azygos veins to form gastric varices or esophago gastric varices respectively [5]. It may be silent and asymptomatic [6, 7]. The usual clinical presentations are abdominal pain according to the severity of CP, bleeding manifestations like, anemia, hematemesis, malena or hematochezia or sometimes with splenomegaly and thrombocytopenia [7, 8, 9, 10].
The controversial aspect is the high rate of bleeding in the olden day’s reports contradicted by the recent studies. Rate of bleeding is almost up to 100% in older reports with a rate of 4% bleeding in recent studies [6].
Splenectomy is the standard curative treatment for SVO with varices and bleeding [1, 11]. Doing splenectomy in patients having tail predominant disease with Spleenic vein thrombosis is well accepted [11, 12]. Conservative management is advised in asymptomatic patients who do not deserve surgery for pancreatic procedures and with or without varices [13]. Is it justified to do splenectomy in symptomatic CP patients who needs surgery but with asymptomatic SVO? This controversy still exists [1, 6, 7].
In the present era as the concept of early surgery is growing to improve the QOL in CP patients [14] there is a need for operative intervention in almost 80% of the patients. Long term results are best achieved by surgical procedures compared to endoscopic procedures [15, 16]. Hence to resolve the issue of whether to do splenectomy in the surgical candidates of CP with asymptomatic SVO is analyzed in this study.
Our study is one of the largest series of unique patient group of chronic pancreatitis with SVO. This study is a prospective follow up of both retrospectively and prospectively collected data. Written informed consent was obtained from each patient and the study is approved by the institutional ethical committee. Total of 365 consecutive chronic pancreatitis (CP) patients admitted in our surgical gastroenterology institute between 2009 and 2015 were analyzed. Among them 39 patients having SVO were included in the study. SVO was diagnosed after confirming normal liver function with non opacification or thrombosis of Spleenic vein and collaterals in Spleenic hilum in MRI/MDCT or endoscopic evidence of gastric fundal varices and confirmed with color Doppler study and by reviewing their intraoperative records. Sarin classification system was used to classify the varices [17]. Patients presented with acute exacerbation of chronic pancreatitis are classified according to the revised Atlanta classification system.
Symptomatic SVO is defined as those having hematemesis, malena, and anemia along with classical features of CP. Others who do not have symptomatic bleeding are defined as asymptomatic SVO.
Surgical candidates are those who present with Symptomatic SVO and those with severe pancreatic pain who needs surgery for pancreatic procedures. These patients were offered splenectomy with or without pancreatic procedures depending upon the symptomatology of CP. Polyvalent pneumococcal vaccine was given 14 days prior to surgery in all patients who underwent elective splenectomy and 10 days after those who underwent emergency splenectomy(n=2).
Non-surgical candidates are those who with present only milder degree of pancreatic pain or acute exacerbation of CP with or without extension of thrombus into the portomesenteric axis. These patients underwent only medical management (Anticoagulants and treatment for pain and pancreatitis) and radiological interventions like PCD and angio embolisation for aneurysm.
Follow up protocol with every 6 months OGD scopy and Doppler study was followed in our institution. Reduction in size of varices and restoration of flow in splenic vein, rate of rebleeding and morbidity and mortality were noted. Data were collected at outpatient setup if necessary telephonic enquiry was made regarding symptom improvement.
Statistical analysis was performed with the help of statistical package SPSS (Statistical Package for the Social Sciences) version 11. Baseline characteristics of both the groups were tabulated by descriptive statistics (mean , standard deviation) and frequency table. They were matched by unpaired student 't' test and Pearson's chi - square test. The categorical variables between two groups were compared by Chi - square test and Fishers Exact test. The p values less than 0.05 (p<0.05) was considered as significant in two tailed condition.
These 39 patients were grouped in to 2 based on whether splenectomy was done (Group 1) or not (Group 2).After grouping these patients all the parameters were almost equally distributed equally in both groups except the severity of pain which was significantly less (p= 0.012) in group 2 (Table 1).

Mean age of presentation was 36.89 years. Males were more commonly affected than females. Mean symptomatic duration of disease is 3.52 years. As with previous studies alcoholic pancreatitis is the most common etiology (82.05%) causing SVO. Pseudocyst being the most common complication (64.1%) associated with SVO, followed by biliary stricture (17.94%), ascitis (17.94%) and fistula (7.7%). The tail location of pseudocyst was most commonly (82.4%) associated with SVO. All patients presented were having standard pancreatic type of pain.
Asymptomatic SVO was found in 21 cases (56.4%). Bleeding manifestations prior to the surgery were found only in 17 (43.6%) patients. Out of these 17 patients 6 patients presented with emergency bleed, 5 of them underwent urgent surgery after stabilization 1 patient underwent angio embolisation only for aneurysm. Remaining 11 patients presented with malena and anemia only.
Compression by pseudocyst (43.6%) and peri portal fibrosis in 7.7% (n=3) of patients rather than the thrombus (n=36) was the cause for SVO, producing the non-visualization of splenic flow. Thrombus was confined to the splenic vein in 88.9% (n=32) and extending in to portomesentic axis in 11.1% (n=4) of cases. Spleeno renal collaterals are more common (48.7%) followed by perigastric and other sites like inter costal vessels, retroperitoneal region, and preiportal area by the MDCT. Angiogram which is considered as the gold standard for diagnosis [18] was done only in those with associated pseudo aneurism and bleeding and in those with nonvisualization of flow in splenic vein, as a good MDCT (128 slice) with vascular and 3D reconstruction and MRV identifies collaterals in all cases. Color Doppler study identifies collaterals in only 41% of patients. Endoscopic evidence of Varices was identified in only 46.2% of cases. Type 1 gastric varices (IGV-1) were the predominantly found varices in our study followed by esophago gastric varices (OGV-2) in 2 cases.
Procedures Performed
Total of 39 patients with SVO with CP 21 patients underwent splenectomy (Group 1) and in the remaining 17 patients 11 underwent only pancreatic procedures and 7 patients are treated with non-surgical management (Group 2) (Table 2).
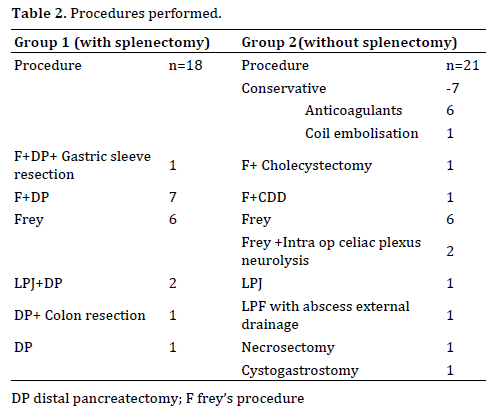
Surgical candidates are those who present with Symptomatic SVO and those with severe pancreatic pain who needs surgery for pancreatic procedures. Nonsurgical candidates are those who with present only milder degree of pancreatic pain or acute exacerbation of CP with or without extension of thrombus into the portomesenteric axis. These patients underwent only medical management (Anticoagulants and treatment for pain and pancreatitis) and radiological interventions like PCD and angio embolisation for aneurysm.
In group 1 the indication for surgery was bleeding manifestations (anemia, malena, frank bleeding like hematemesis) in 9 patients & in 13 patients the tail predominant disease. Two of them underwent emergency surgery after failed endotherapy. In group 2, 10 patients underwent only pancreatic procedure in those without OGD evidence of varices. 6 patients with mild disease and with acute exacerbations on CP are treated only with supportive management. Anticoagulants are prescribed when there is extension of thrombus in to portomesenteric axis.1 patient underwent angio embolisation of splenic artery aneurism under antibiotic coverage and doesn’t required splenectomy on follow up.
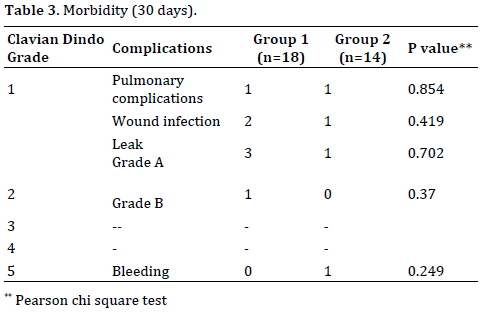
Postoperative Complications (30 days)
The post-surgical complications are graded according to Clavian Dindo classification system. Pulmonary infection was found equally in both groups. Grade A and B leaks are more in those who underwent distal resectional procedures and those who underwent Necrosectomy. One patient in group 2 who underwent only Frey’s procedure was admitted with bleeding after 28 days from the pancreatico jejunal anastamosis but expired after surgical exploration (Table 3).
Follow-up Assessment
Resolution of varices as evidenced in OGD scopy was seen in all patients in group 1 but with only 37.5% in group2 patients especially with compressive etiology. In group 2, 7 had resolution of venous thrombosis was evidenced in MDCT and Doppler 15 had persistence or nonvisualization on MDCT hence close follow up is necessary in these group of patients (Table 4).
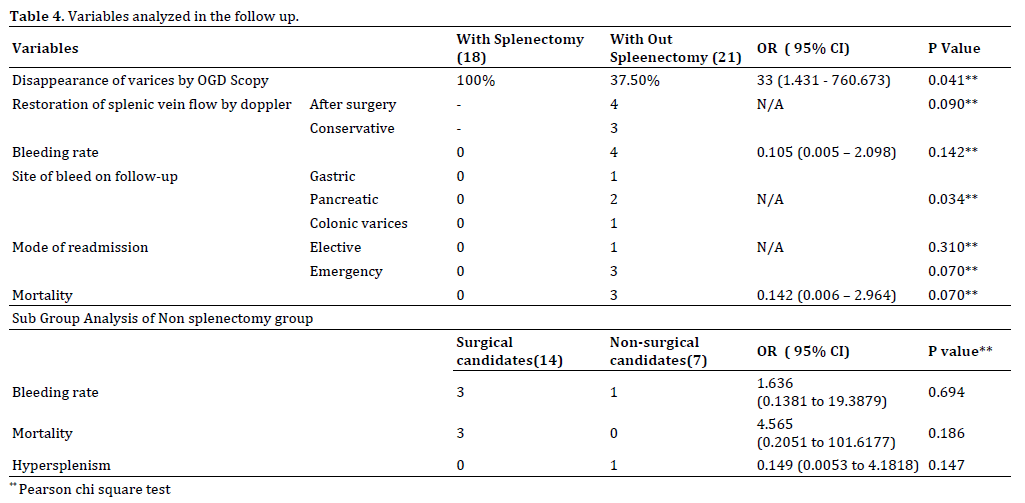
None of them in the spleenctomised patients bleed in the follow up period. But 4 patients (19.04%) in the non spleenctomised patients developed varices in the follow up. Off these 3 patients died. One patient treated by conservative method that was under anticoagulants developed bleeding from the gastric varices and required endoscopic management of glue injection but developed features of hyperspleenism and required splenectomy in the follow up period after 2.2 years after primary diagnosis.
The mortality rate of bleeding is 75% in the postoperative patients. All 3 patients were admitted with bleeding manifestations. 1 patient died in the emergency department itself with massive bleeding per rectum from the colonic varices. Second patient admitted 30 days after the Frey’s procedure with malena and shock. After resuscitation CT angiogram was done. Bleeding source could not be identified. On exploration he was found to have bleeding from the pancreatico jejunal anastamosis both intra& extraluminaly. Even though bleeding was arrested with reinforcing sutures with distal pancreatectomy and splenectomy, patient required 8 units of blood transfusion, but developed MODS and shock and expired on the next post-operative day. Third patient admitted 2 years after surgery with malena on evaluation with endoscopy he had hemosuccus pancreaticus. Patient expired on the same day. Autopsy studies confirmed the presence of small ruptured splenic artery pseudo aneurism with varices at pancreatico jejunal anastamotic site and retro peritoneal varices. Figure 1 showing the survival curve which is better for the cohort of patients who underwent splenectomy along with pancreatic procedures.
Factors Affecting Rate of Bleeding
Bleeding manifestations like anemia, hematemesis, and malena were observed in 43.6% of patients in our study. Those patients with bleeding are compared with the nonbleeders to find out the factors associated with bleeding, manifestations. Even though clinically not significant, patients with alcoholic etiology and normal range of amylase levels are more prone for bleeding. There is no difference found with disease duration and severity. Location and number of pseudocyst and extend of thrombus does not predict the bleeding in these patients. The mean platelet value in those with bleeding was 2.44 lakhs ±0.986, and 2.14 ±1.26 in non-bleeders. Neither platelet count nor did splenic size and platelet count /splenic size ratio predicted the risk of bleeding. Presence of associated aneurysm and spleno renal collaterals appears to have more chances of bleeding (p=0.058) compared to other sites (Table 5).
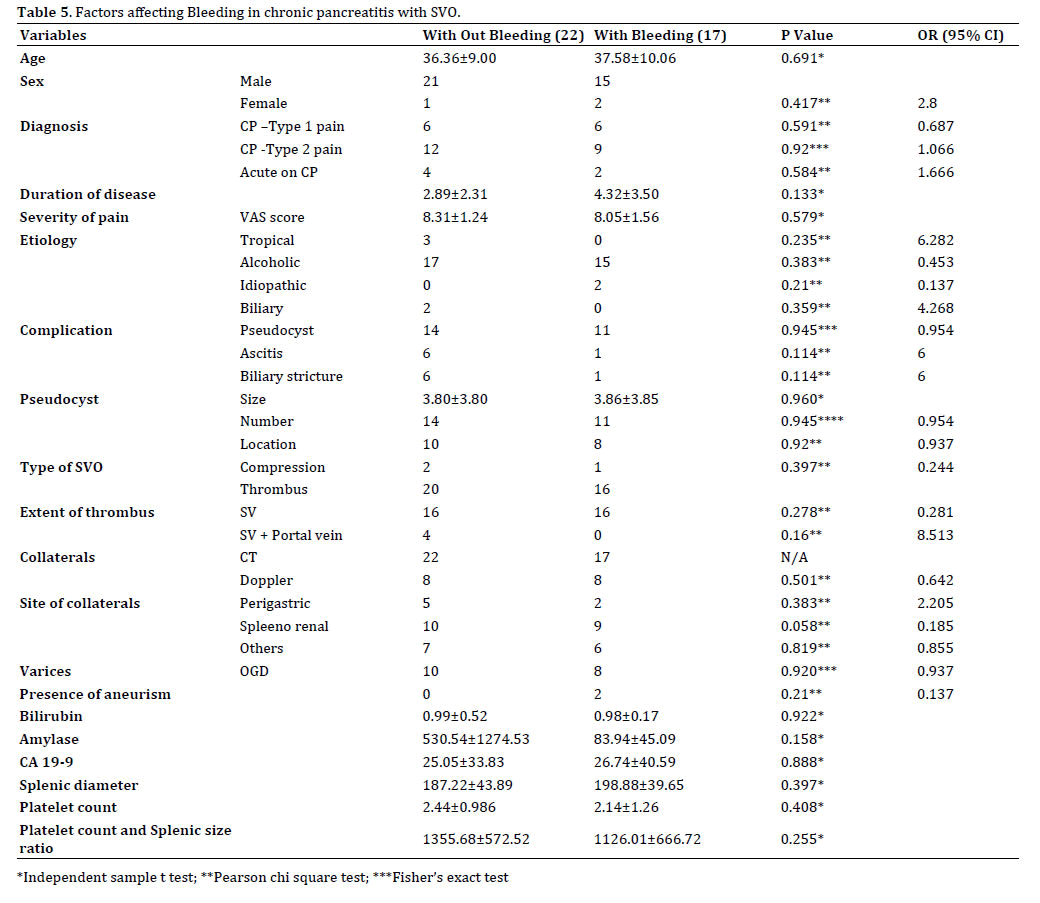
These factors along with the endoscopic signs of larger varices should be carefully followed up because there are no warning symptoms except the pancreatic pain until the onset of hemorrhage. To be mentioned, there is no accurate way of predicting this complication especially in the post-operative patient in whom splenectomy was not performed and the site of dangerous bleeding may not be always from the gastric varices but also from the anastamotic site or from the colonic varices.
Treatment of choice for bleeding gastric varices from splenic vein thrombosis is splenectomy [19]. Splenectomy at time of distal pancreatic resection is an accepted modality of treatment. But in patients without tail disease prophylactic splenectomy while undergoing pancreatic procedure is still remains as an unresolved issue. This issue is addressed by answering the following questions like the natural course of the disease of patients on conservative management and the rate of bleeding after doing surgical procedure without splenectomy and morbidity after adding splenectomy in these patients.
The frequency of gastrointestinal bleeding in previous studies [3, 6, 7, 20, 21, 22] ranged from 4 to 100%. A 1985 review by Moosa and Gadd [23] found that nearly half of all patients with splenic vein thrombosis, presented with bleeding. Largest metaanalysis by Butler et al. reported a rate of 12.3% GI bleeding [24]. In these analysis both acute and chronic pancreatitis are included. This gross difference is not only due to increased detection of asymptomatic SVO with modern diagnostic modalities but may also be due to selection bias of surgical cohort of patients [6, 25]. This may be because in the symptomatic pancreatitis patients who need surgical management obviously will have the severe involvement of adjacent organs also which might have caused the high rate of bleeding as in the older reports.
In a study by Heider et al. in 2004 [6] concluded that gastric variceal bleeding from pancreatitis-induced splenic vein thrombosis occurs in only 4% of patients; therefore, routine splenectomy is not recommended. In his study 60.4% are non-surgical candidates and acute pancreatitis (25%) patients also were included like in the study by Bernades et al. [1]. This may not be representative of surgical candidates of chronic pancreatitis patients [24] (Table 6).
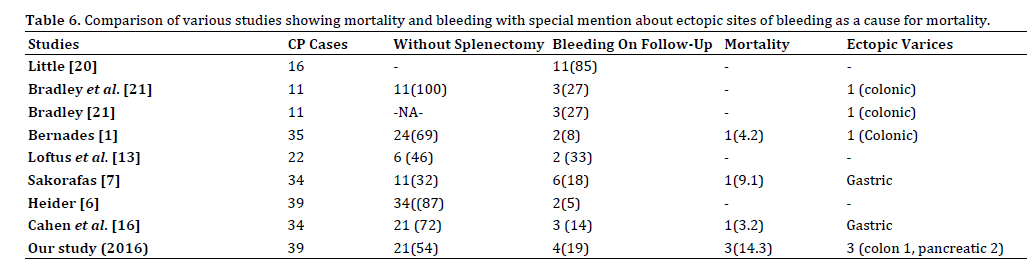
Like previous reports [24, 26] patients undergone only pancreatic procedures experienced bleeding even though there is resolution of thrombus noted in few cases (<40%). Concomitant splenectomy may be considered in patients undergoing operative treatment of symptomatic chronic pancreatitis if sinistral portal hypertension and gastroesophageal varices are present [7, 24]. Even though it was proved that presence of varices on endoscopy increased this risk nearly 4-fold [6] absence of gastric varices does not always rules out bleeding risk from other sites. Loftus et al. suggested observation in patients without prior bleeding episodes, anemia, or severe hemorrhage [13].
It is often a daunting task to follow up and treat the patients with fundal varices. Although most patients remain totally asymptomatic until the onset of hemorrhage [12], variceal bleeding may be life threatening [8, 9, 10]. Often the patients with recurrent bleeding were presented at the emergency department with severe bleeding. Timing of bleed and factors predicting bleeding and the long term results of endoscopic gastric variceal injection therapy [7] are still unclear. Sudden massive bleeding from the varices is the most common cause for mortality. This is very critical to consider that most of the patients were brought very late to the hospital and often leading to poor prognosis. Two of the 3 patients who had bleeding in the follow up were from remote areas away from tertiary care center where the interventional endoscopic procedures are available.
Not only patients with bleeding symptoms but also who develops, hyperspleenism features on follow up like anemia, tiredness, mass abdomen (splenomegaly) requires splenectomy in an elective setting.
The blood flow direction is either way through the path of least resistance when there is obstruction to the natural venous drainage pathway. As noted in previous reports (Table 6) it is not only gastric and/or esophageal varices as source of bleeding but also from the previous surgical anastamotic site like choledocho jejunostomy and pancreatico jejunostomy and also from the colonic varices [1, 10, 21, 27, 28, 29, 30]. As the pancreas itself will act as a siphon with high pressure intra and peripancreatic collaterals in SVO there is increased risk of early and delayed bleeding not only from the gland and suture lines, but also from the pancreatico jejunal anastomosis. The formation of ectopic colonic varices may be due to alternative pathways of blood flow from the splenic vein especially after surgical procedures. Ectopic sites are very difficult to be assessed and treated by endoscopic measures [21, 31] and often the cause for mortality.
Doing surgery in portal hypertensive patient is always a difficult task for surgeons because of the presence of collaterals [19]. Presence of perigastric, retroperitoneal and diaphragmatic varices not only increases the bleeding but also makes the dissection and control of splenic artey difficult due to a chronic inflammatory reaction that obliterates the lesser sac. In this situation initial supragastric ligation of splenic artery helps to reduce the bleeding and we also feel this as an effective strategy [7].
Some advocates preoperative splenic artery embolisation to do a safe splenectomy [32]. This modality may be utilized before doing pancreatic surgery and splenectomy. As using this technique routinely before doing pancreatic procedures increases the cost of the procedure in our set we selectively perform this procedure only in those presenting with aneurysm and bleeding.
Finally, adding splenectomy almost never lead to any major morbidity or mortality in most of the series but there are reports of mortality when splenectomy was not added during surgical procedures and those on conservative management [21, 33]. There are case reports and studies to show that previous pancreatic surgery without splenectomy itself induces SVO after a period of 6 months to 3 years [7, 31]. Hence adding splenectomy should be strongly considered in surgical candidates of chronic pancreatitis with SVO even though asymptomatic [7, 24, 34, 35]. Conservative management may be advised for mild chronic pancreatitis and those in close reach for advanced care centers with strict adherence to follow up.
We strongly advise routine splenectomy while performing surgical management of chronic pancreatitis even in non-bleeders especially in patients with remote access to health care facilities as a single stage treatment. Because it not only obviates the need for the long-term follow up for varices but also reduces the mortality without increasing the morbidity of surgical procedure.
The authors have no conflicts of interest.