- (2006) Volume 7, Issue 1
Raffaele Pezzilli, Lorenzo Fantini, Antonio Maria Morselli-Labate
Department of Internal Medicine and Gastroenterology, Alma Mater Studiorum - University of Bologna, Sant'Orsola-Malpighi Hospital. Bologna, Italy
Received: 31 October 2005 Accepted: 21 November 2005
Drug Evaluation, Preclinical; Nutrition Therapy; Pancreatitis; Pancreatitis, Acute Necrotizing; Pancreatitis, Alcoholic; Pharmacological Actions Category; Practice Guidelines

This slide presentation took place at the Meeting of the European Societies of Pancreatology held in Lisbon in October 2005.
In the last few years, several new therapeutic options have changed the management of acute pancreatitis; for example, the therapeutic ERCP with endoscopic sphincterotomy in severe biliary pancreatitis, the use of early antibiotic treatment in necrotizing pancreatitis and the demonstration that enteral feeding is able to decrease the inflammatory response. In this paper we describe the therapeutic news which could modify the current approach to acute pancreatitis in the near future. This is possible only because we have new information in order to better understand the pathophysiological processes of the disease.
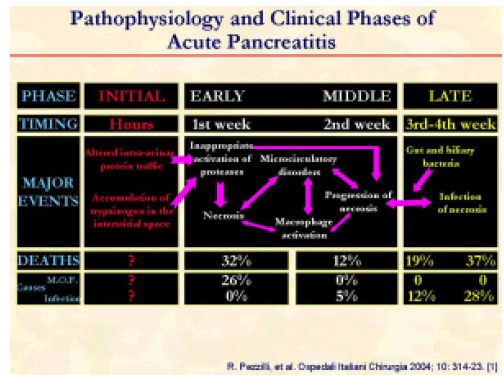
We can distinguish three clinical phases regarding the pathophysiology of acute pancreatitis. There is not very much information on the initial phase of the disease in humans and, for the most part, it comes from experimental studies [1]. Of course, it is apparent that we can obtain good therapeutic results only if we treat the pancreatitis as soon as possible.
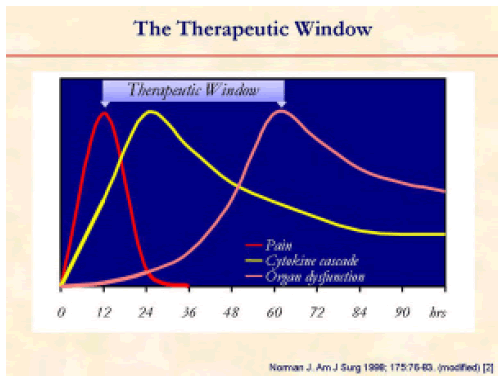
The time limit for efficacious medical treatment is of no more than 60 hours from the onset of symptoms of acute pancreatitis [2].
Another important aspect as to the correct approach to the management of acute pancreatitis is the correct clinical classification of acute pancreatitis. We should thank Dr. Bradley for his efforts in changing the classification of the disease from a pathological to a clinical point of view [3].
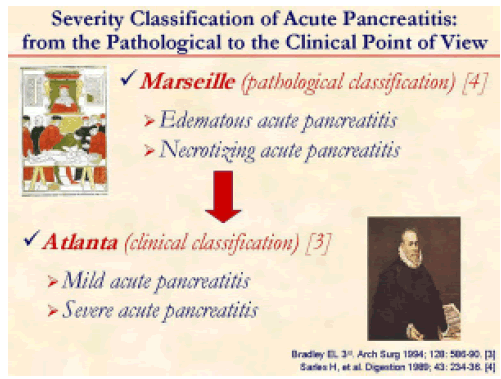
The work of Bradley can be summarized in the evolution from the Marseille [4] to the Atlanta [3] classification system.
As in other diseases, also in acute pancreatitis, the pathophysiological aspects of the disease should guide our therapeutic approach. On the other hand, we should also consider that the treatment needs to be tailored to each individual patient and we also should take into account the available resources of each Institution.
In the last few years, the need has emerged to treat patients with acute pancreatitis according to new knowledge accumulated from clinical research in order to improve the morbidity and the mortality of the disease.
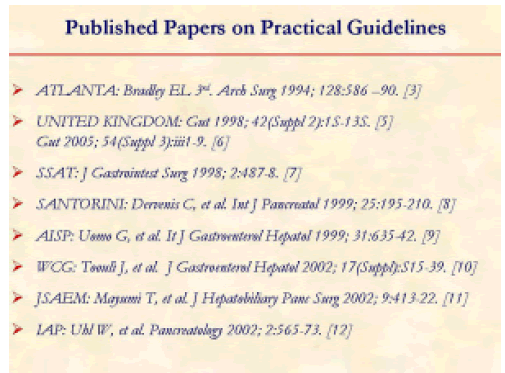
Since 1994, many papers have been published suggesting the good medical practice to be followed in the treatment of acute pancreatitis [3, 5, 6, 7, 8, 9, 10, 11, 12].
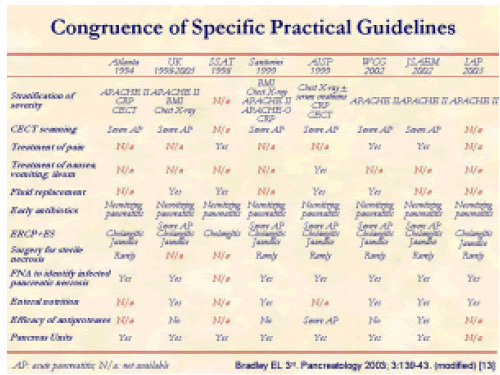
There is no congruence in the various guidelines regarding stratification of severity, diagnosis, treatment and presence of Pancreas Units [13].
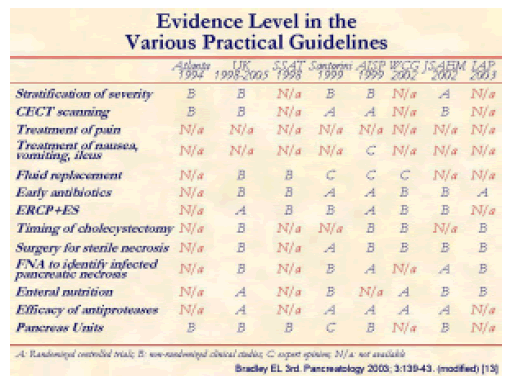
In the same way, there are no homogeneous evidence levels in the various guidelines [13].
These differences are quite surprising because most of the participants are the same experts who decide on the various guidelines.
In addition to the suggestion of Bradley about the need of guiding the reluctants [13], there is also the need to unify the various guidelines.
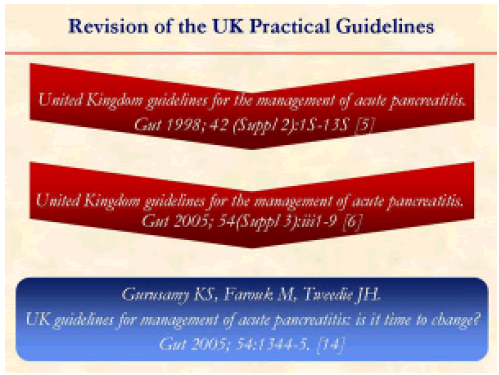
One example of rapid evolution of the knowledge of acute pancreatitis is the following: the UK guidelines were released in 1998 [5], revised in 2005 [6] and, after just a few weeks, some researchers asked to change the new 2005 UK guidelines [14].
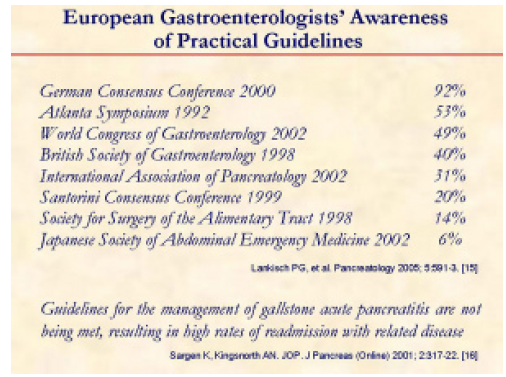
Another problem with the guidelines is that many clinical practitioners in the same country follow different guidelines [15] and others do not fully apply them in clinical practice [16].
In most of the guidelines, the basic management of acute pancreatitis is not reported: some examples are the control of pain and the control of the nausea, vomiting and ileus.
First of all, what about the control of pain?
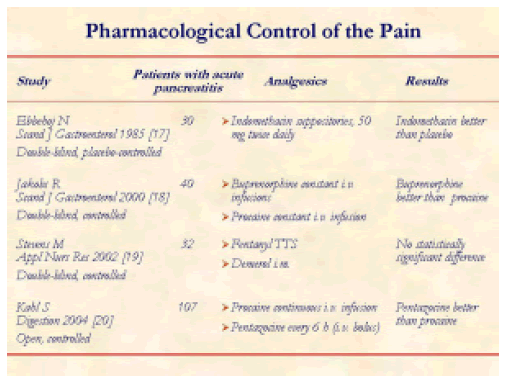
There are no extensive studies on the pharmacological control of pain in acute pancreatitis [17, 18, 19, 20]; this is quite surprising due to importance of this symptom.
Second, what about the control of nausea, vomiting, and ileus?
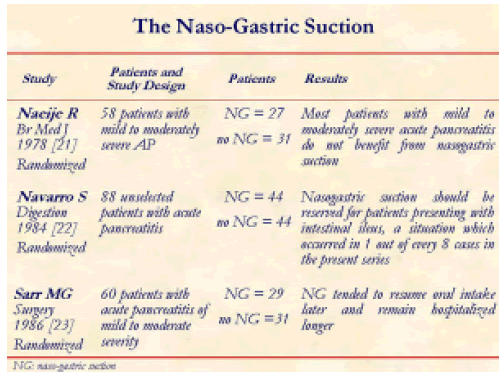
Naso-gastric suction is often used in patients with acute pancreatitis, even if most of the published studies limit this approach only to the patients with severe disease [21, 22, 23].
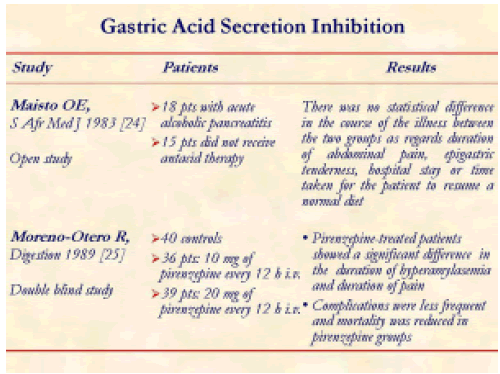
Gastric acid secretion inhibition is largely used in patients with acute pancreatitis, even if there are very few studies on this issue and the results are not conclusive [24, 25].
Even if many studies have been carried out, only a few of the substances tested have been applied in clinical practice.
This is the first experimental study exploring the usefulness of Infliximab in the treatment of severe acute pancreatitis [26].
Antioxidant treatment for acute pancreatitis is a neverending story; this is one of the most recent studies exploring the usefulness of a new antioxidative drug in experimental acute pancreatitis [27].
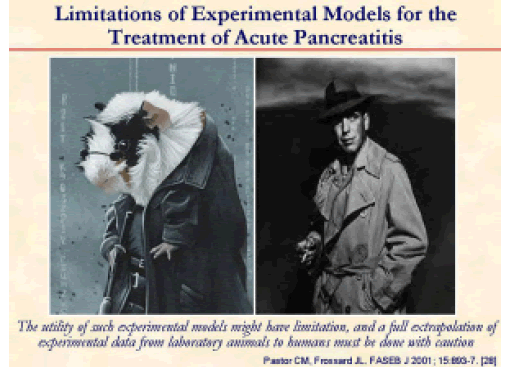
A paper published in 2001 highlighted the limitations of experimental models in acute pancreatitis [28].
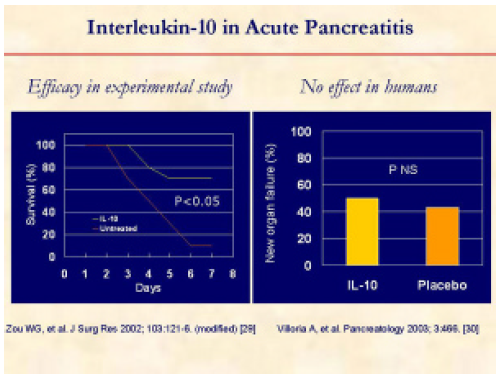
Interleukin-10 represents a case of limitation of experimental research. In fact, this molecule was unable to prevent new organ failures in clinical practice [29, 30].
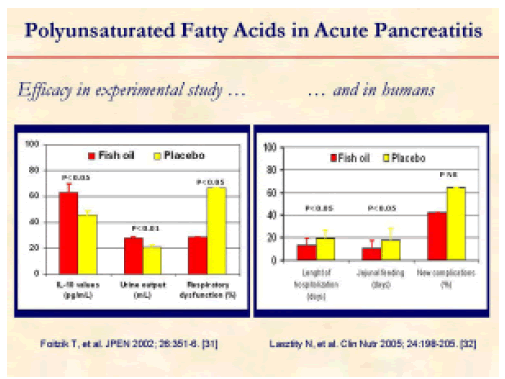
On the other hand, polyunsaturated fatty acids were able to decrease the length of hospitalization and the duration of jejunal feeding in humans, even if they were not able to decrease the number of new complications [31, 32].
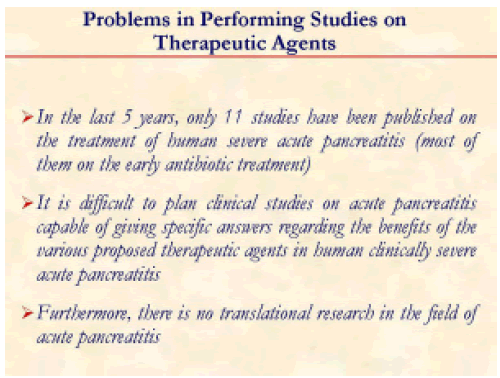
What are the problems in carrying out studies on therapeutic agents in acute pancreatitis?
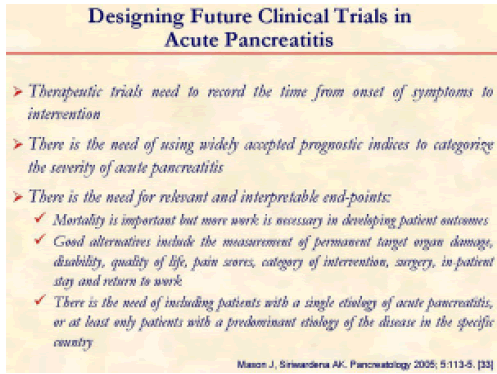
There is the need to better design future clinical trials in acute pancreatitis [33].
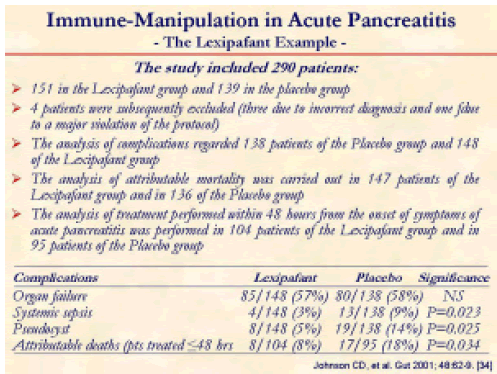
The high incidence of organ failure within 72 hours after the onset of symptoms has undermined the primary hypothesis, and power calculations for future studies on severe acute pancreatitis will need to allow for this. Lexipafant had no effect on new organ failure during treatment. This study - performed with an adequately sized sample - has shown that antagonism of the PAF activity on its own is not sufficient to ameliorate SIRS in severe acute pancreatitis: However, if we look at the data reported, we cannot exclude that Lexipafant may have some effect, especially in patients treated within 48 hours from the onset of symptoms [34].
The restoration of homeostasis with a single intervention belies the complex and coordinated nature of the inflammatory response. In clinical practice there is necessity of not using “magic” drugs alone: there is the need for more drugs capable of involving the different aspects of the disease [35].
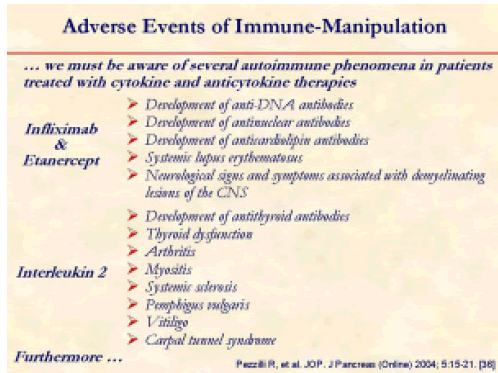
Furthermore, we must be aware of several autoimmune phenomena in patients treated with cytokine and anticytokine therapies [36].
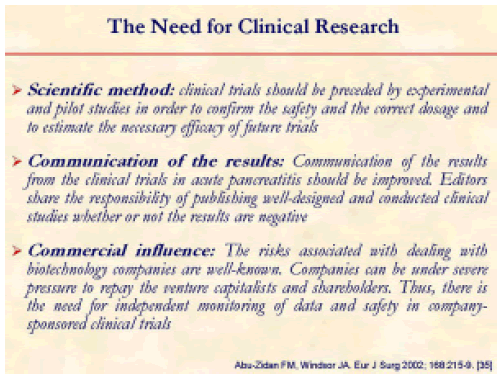
We also need to change the way results of drug trials are communicated to the medical world [35].
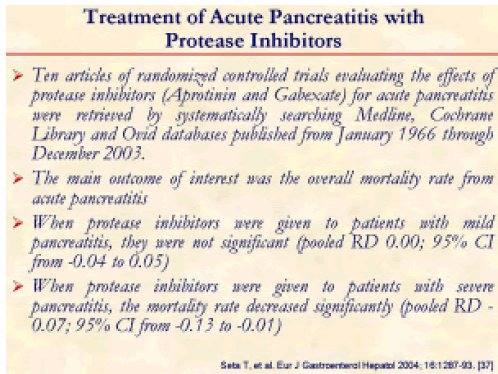
One example may be the highly debated efficacy of protease inhibitors in human acute pancreatitis [37].
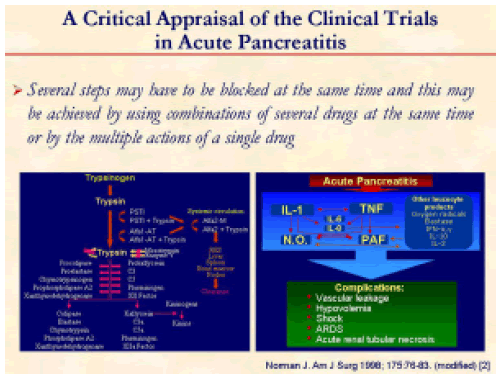
Several steps may have to be blocked at the same time and this might be achieved by using several drug combinations at the same time or by the multiple action of a single drug in order to block the protease cascade as well as the cytokine cascade [2].
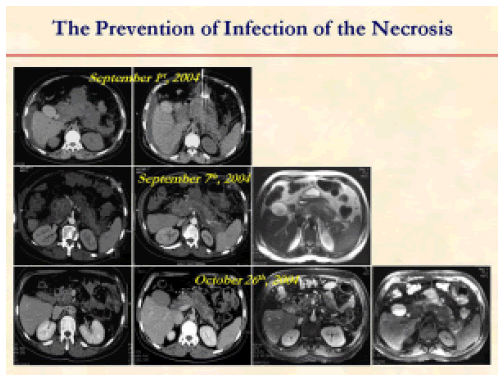
Another important aspect for the treatment of acute pancreatitis is the prevention of the infection of pancreatic necrosis.
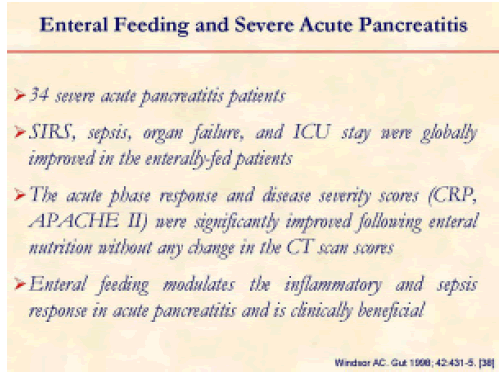
This is the first clinical study demonstrating the beneficial effect of enteral nutrition in decreasing the inflammatory and sepsis response in severe pancreatitis [38].
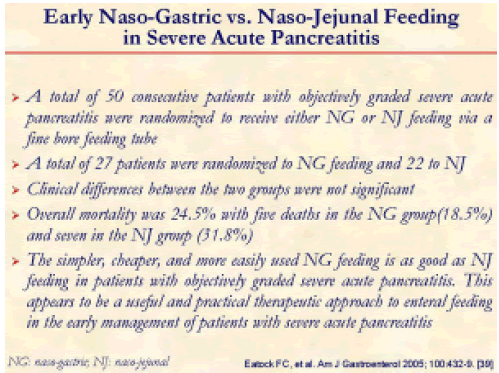
There is no doubt that it is better to administer enteral feeding via a naso-gastric tube than via a naso-jejunal tube [39].
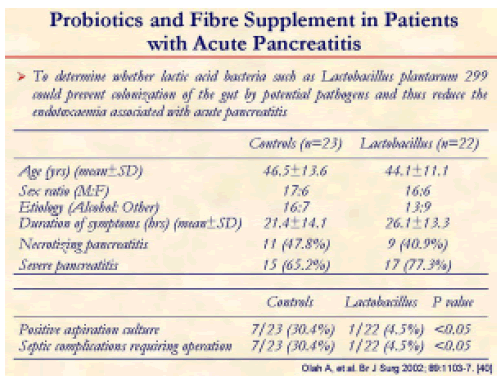
There is also no doubt that probiotics associated with enteral feeding may become an alternative therapy replacing early antibiotic use to prevent infection in severe pancreatitis [40].
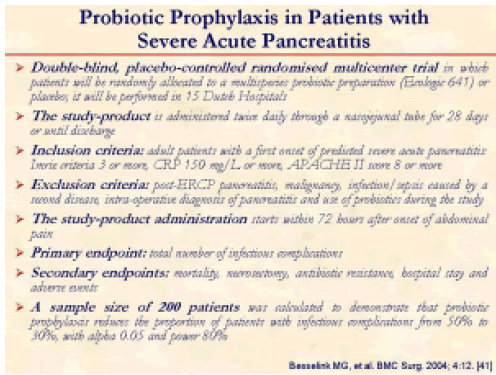
We are awaiting the results of this study in order to draw the final conclusion on the effectiveness of probiotic prophylaxis in preventing septic complications in severe acute pancreatitis [41].
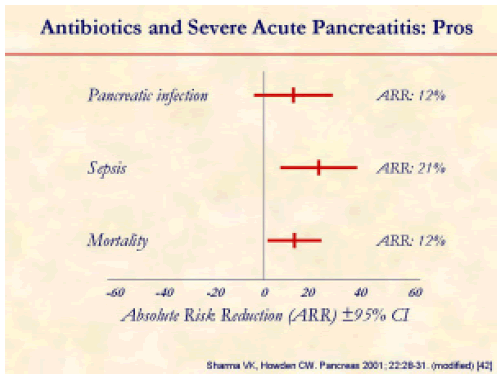
This meta-analysis shows the need for using early antibiotic therapy in order to prevent sepsis and mortality in severe acute pancreatitis [42].
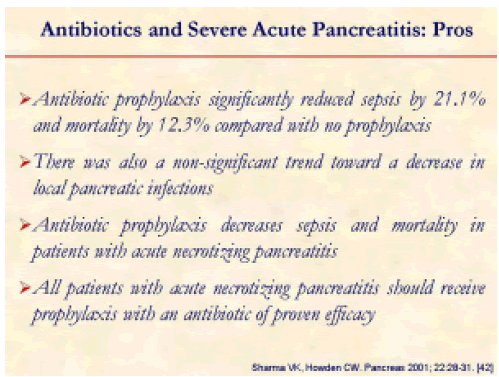
The authors concluded that all patients with acute necrotizing pancreatitis should receive early antibiotic treatment [42].
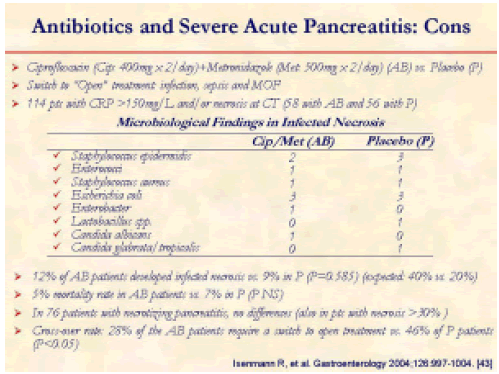
However, not all researchers agree that severe acute pancreatitis should be treated with early antibiotic administration [43].
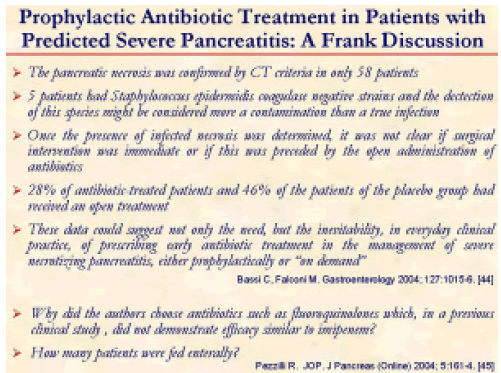
After the publication of the paper of Isenmann R, et al. [43], a discussion on its validity was opened [44, 45].
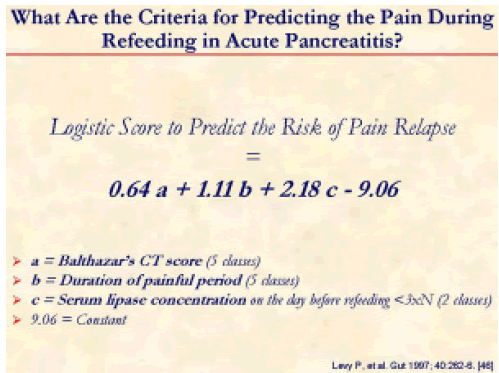
Refeeding is crucial in patients who have recovered from an acute episode of pancreatitis but there are very few studies on this issue [46].
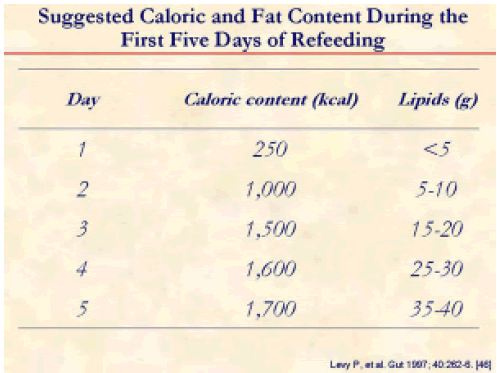
This is the suggested caloric intake for the refeeding of acute pancreatitis patients [46].
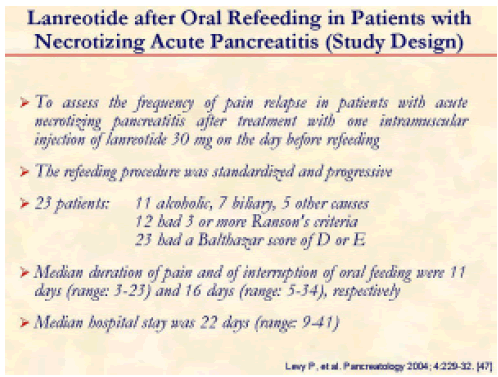
To prevent an acute relapse of acute pancreatitis, the use of lanreotide has been suggested [47].
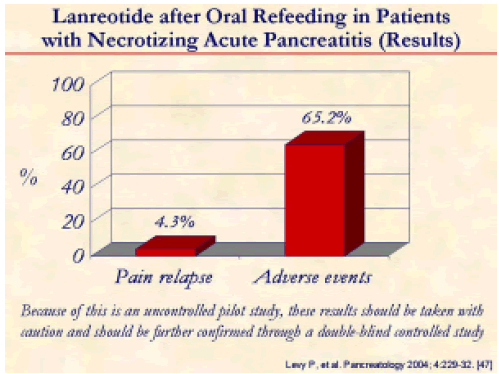
In this French study, only 4.3% of the patients treated with Lanreotide had relapse of pain from acute pancreatitis, but 65.2% experienced adverse effect using the drug [47].
There are very few studies evaluating the exocrine pancreatic function after an acute episode of pancreatitis [48, 49, 50, 51].
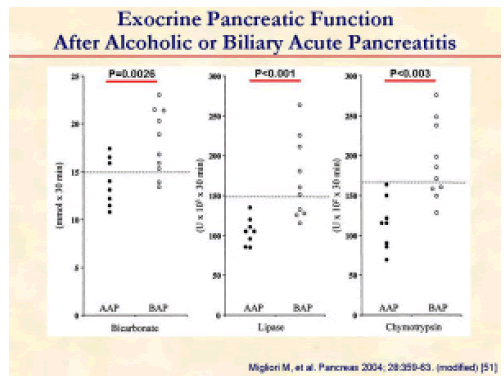
An example of the exocrine pancreatic study comes from the paper of Migliori et al. [51]. In this study patients with acute pancreatitis were studied using the secretin-cerulein test. After acute alcoholic pancreatitis, pancreatic insufficiency was significantly more frequent and more severe than after biliary pancreatitis. These findings, together with the fact that the insufficiency was also more persistent, suggest that acute alcoholic pancreatitis may occur in a pancreas which already has chronic lesions.
Enzyme supplementation during the refeeding of patients with acute pancreatitis represents an important issue regarding nutritional support. However, there are no studies showing the possible efficacy of enzyme oral supplementation especially in those patients who suffered from acute alcoholic pancreatitis.