Keywords
Betamethasone; Calcipotriol; Psoriasis; Maintenance
Introduction
Psoriasis, a chronic and recurrent skin disease, affects 1-3% of the general population [1]. The most common form of psoriasis is psoriasis vulgaris, usually characterized by pink to red scaly papules and plaques symmetrically. The quality of life of psoriasis patients is often reduced. Patients usually have high expectations on therapy with the wish for a rapid and long-lasting improvement together with good tolerability and practicability [2].
Topical therapy is a fundamental treatment for patients with mild to moderate psoriasis [3]. The optimal regime should provide both rapid, short-term control of the disease and safe, long-term remission. Most topical medication is based on corticosteroids (such as betamethasone) and vitamin D analogues (such as calcipotriol or tacalcitol) [4]. A two-compound product containing calcipotriol and betamethasone (calcipotriol/betamethasone dipropionate ointment) has been developed in order to avoid separate applications and to improve patient compliance [5]. In the treatment of psoriasis vulgaris of active stage, the twocompound product was found to be more effective and safe than either a corticosteroid or a vitamin D analogue alone [6]. The patients are satisfied by the treatment as they can usually see improvement of their clinical condition in a short period of time [3]. However, the data of stationary stage was lack. Our study aimed to investigate the optimal usage of calcipotriol / betamethasone ointment on maintaining the efficacy of psoriasis vulgaris on stationary stage.
Patients and Methods
Subjects enrollment
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki, and was approved by our Institutional Medical Ethics and Human Research Committee. Patients with a clinical diagnosis of psoriasis vulgaris at stationary stage were recruited, from outpatient clinics of the department of dermatology, No. 1 Hospital of China Medical University. The clinical criteria for stationary stage were as follows: the red color of original lesions being lightening, the scale of original lesions being less, and no new lesions appeared. All patients signed consent to participate in the trial. The ages were 18 to 75 years old. The lesions affecting no more than 10% body regions and the Psoriasis Area Severity Index (PASI) not exceeding 10 were requested. The main exclusion criteria were psoriasis vulgaris at active stage, other inflammatory skin diseases confounding the assessment of psoriasis, hypercalcaemia, pregnancy or breast feeding, systemic anti-psoriatic treatment or photo(chemo) therapy within previous 1 month. Patients who were being treated with any topical agent when presented to us and agreed to stop the agent were allowed to join our study.
Treatment
All patients were randomized to one of 3 groups (A, B, C) according to random number table, and received 3-month treatment. Patients in group A received the treatment with calcipotriol/ betamethasone ointment (Daivobet?RR, containing calcipotriol 50 μg/g and betamethasone 0.5 mg/g dipropionate, LEO Pharma, Ball-erup, Denmark) twice weekly, group B received the same ointment once weekly, and group C received calcipotriol ointment (Daivonex?RR , containing calcipotriol 50 μg/g, LEO Pharma, Ballerup, Denmark) once daily. All patients used albolene (Hongqi Pharmaceutical Co., Ltd., Shenyang, China) twice to thrice daily during the 3-month treatment.
Assessments
The extent and severity of psoriasis were recorded at each visit (month 0, M0; M1; M2; M3) using PASI. Patients’ global assessments of treatment response compared to baseline were evaluated on a 4-point scale (excellent, moderate, good, no change or worse). All adverse events were recorded.
Statistical methods
Data were analyzed by SPSS for Windows (version 20.0, SPSS Inc.). The baseline data including age and sex of different groups were analyzed with Analysis of variance (ANOVA) and χ2 test. Comparison of PASI was analyzed using ANOVA for repeated measures and LSD test. P-value < 0.05 was considered as statistical significance. Comparison of patients’ satisfaction was analyzed with Kruskal-wallis H, P-value < 0.05 was considered as statistical significance in general comparison and P-value < 0.017 was considered as statistical significance between paired samples.
Results
A total of 96 patients (each group 32 cases) entered the study from March 2014 to December 2014. The three groups were well balanced at baseline for age (F=0.210, P=0.811) and sex (χ2=0.156, P=0.925). The baseline characteristics of patients were displayed in Table 1. During the study, respective 2 and 3 patients of group B dropped out of the study at M1 and M2, and 1 patient of group C dropped out at the M3. Finally, 32 patients of group A, 27 of group B and 31 of group C finished the study.
| |
Group A
( n=32) |
Group B
( n=27) |
Group C
( n=31) |
| Age range |
19ÃÆÃâÃâïÃÆââ¬Å¡ÃâýÃÆââ¬Å¡Ãâ¦Ã¾61 |
20ÃÆÃâÃâïÃÆââ¬Å¡ÃâýÃÆââ¬Å¡Ãâ¦Ã¾67 |
22ÃÆÃâÃâïÃÆââ¬Å¡ÃâýÃÆââ¬Å¡Ãâ¦Ã¾63 |
| Mean age |
40.19±10.82 |
40.7±11.81 |
42.03±12.18 |
| Male: Female |
53.1% : 46.9% |
55.6% : 44.4% |
58.1% : 41.9% |
| PASI score range |
2.4ÃÆÃâÃâïÃÆââ¬Å¡ÃâýÃÆââ¬Å¡Ãâ¦Ã¾6.5 |
2.7ÃÆÃâÃâïÃÆââ¬Å¡ÃâýÃÆââ¬Å¡Ãâ¦Ã¾7.9 |
1.9ÃÆÃâÃâïÃÆââ¬Å¡ÃâýÃÆââ¬Å¡Ãâ¦Ã¾10 |
| Mean PASI score |
4.37±1.00 |
4.64±1.31 |
4.99±1.76 |
Table 1: Baseline characteristics of patients in the study.
Efficacy
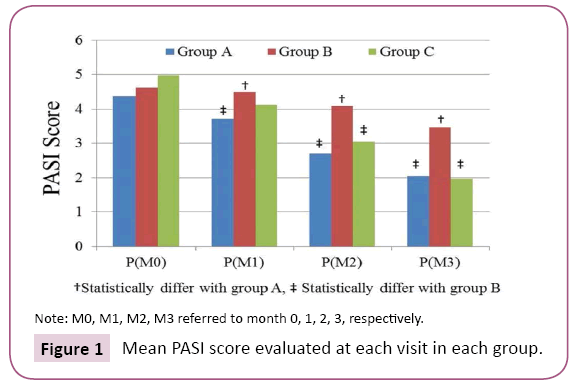
At baseline, the mean PASI score of the 3 groups ranged from 4.369 to 4.990, and no significant difference was seen among the groups (F=1.574, P=0.213) (Figure 1). From M0 to M3, lesions of patients in all the 3 groups significantly improved, respectively (group A: F=688.99, P=0.000; group B: F=367.63, P=0.000; group C: F=221.48, P=0.000). Comparing to M0, the PASI scores of group A and group C respectively decreased to 3.713 ± 0.826 (P=0.000) and 4.113 ± 1.347 (P=0.000) at M1, further decreased to 2.713 ± 0.689 (P=0.000) and 3.045 ± 1.330 (P=0.000) at M2, and reached a very low level of 2.056 ± 0.765 (P=0.000) and 1.971 ± 1.118 (P=0.000) at M3. For group B, the PASI of M1 almost unchanged at 4.496 ± 1.235 (P=0.383), and decreased to 4.085 ± 1.309 (P=0.019) at M2 and 3.470 ± 1.242 (P=0.000) at M3.
Figure 1: Mean PASI score evaluated at each visit in each group.
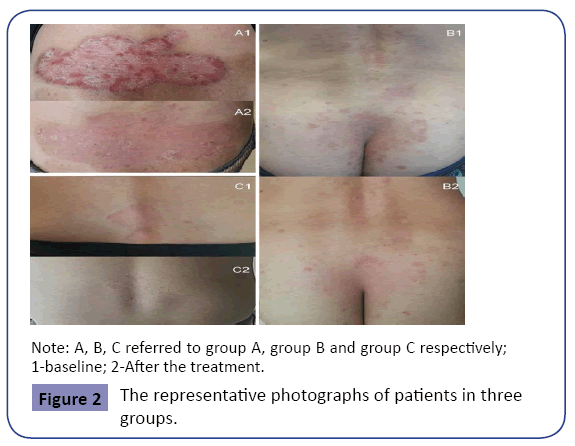
Figure 2: The representative photographs of patients in three groups.
General contrast within 3 groups had significantly statistical difference (F=5.974, P=0.004). The PASI scores of group A were significantly lower than those of group B at whatever M1, M2, or M3 (P<0.05). Whereas no significant difference was seen between group A and group C at all these time-points (P>0.05). The PASI score of group B was similar with that of group C at M1 (P=0.209), but higher than that of group C at either M2 (P=0.001) or M3 (P=0.000).
Satisfaction scale
In group A, over 90% patients were satisfied as “moderate to excellent” with the treatment at M1. With the ongoing treatments, the satisfaction degree remained at the high level and no significant was seen among M1, M2 and M3 (χ2=0.258, P=0.879) (Table 2). In group B, only about 50% patients scored moderate to excellent at M1. The percentage decreased to 40.7% at M2 and further to 37% at M3 (χ2=1.010, P=0.604). In group C, about 70% patients rated their satisfaction as “moderate to excellent” at each time-point and there were no significant difference among the three time-points (χ2=0.752, P=0.687).
| |
|
Excellent |
Moderate |
Good |
No change or worse |
| group A (N=32) |
|
|
|
|
| |
M1 |
4
(12.5%) |
25
(78.1%) |
2
(6.3%) |
1
(3.1%) |
| |
M2 |
6
(18.8%) |
21
(65.6%) |
3
(9.4%) |
2
(6.2%) |
| |
M3 |
6
(18.8%) |
23
(71.9%) |
1
(3.1%) |
2
(6.2%) |
| group B (N=27) |
|
|
|
|
| |
M1 |
2
(7.4%) |
12
(44.5%) |
7
(25.9%) |
6
(22.2%) |
| |
M2 |
1
(3.7%) |
10
(37.0%) |
9
(33.3%) |
7
(26.0%) |
| |
M3 |
1
(3.7%) |
9
(33.3%) |
10
(37.0%) |
7
(26.0%) |
| group C (N=31) |
|
|
|
|
| |
M1 |
4
(12.9%) |
18
(58.1%) |
8
(25.8%) |
1
(3.2%) |
| |
M2 |
4
(12.9%) |
20
(64.5%) |
5
(16.1%) |
2
(6.5%) |
| |
M3 |
3
(9.7%) |
18
(58.1%) |
7
(22.5%) |
3
(9.7%) |
Table 2: Satisfactory scale of patients in the study (n(%)).
After series treatments, the satisfaction score showed significantly different among three groups (M1: χ2=9.175, P=0.01; M2: χ2=14.474, P=0.001; M3: χ2=17.348, P=0.000). At whether M1, M2 or M3, the patients’ satisfaction degree of group A was higher than that of group B (P<0.017) and similar with group C (P>0.017). No significant difference was seen between group B and group C at M1 (P=0.070) and M3 (P=0.017), but it was significantly different at M2 (P=0.004). Figure 2 showed the representative photographs of the patients.
Safety
Two cases in group A developed slight to moderate pigmentation, and 4 cases in group C had mild eruption and pruritus during the treatment. Other adverse effects such as hirsutism, skin atrophy, telangiectasia, acne, folliculitis, local infection were not observed. There were no serious adverse events deemed to be related to use of any study medication during the study.
Discussion
Topical sequential therapy for psoriasis vulgaris is designed to maximize the speed of improvement as well as the overall success rate at the beginning of the therapy and to smoothly transition to safe, long-term maintenance at the end of therapy [7]. Classic topical sequential therapy contains 3 steps, i.e., clearing phase (step 1), transitional phase (step 2) and maintenance phase (step 3) [8,9]. The step 1 and step 2 belong to induction phase, and the step 3 is described as the period of treatment after induction [10]. In step 1, psoriasis patches of active stage are completely or nearly cleared. In step 2, the risk of rebound from the abrupt discontinuation of topical agents is minimized by making a gradual transition. In step 3, the efficacy of disease is safely and extendedly maintained at stationary stage. However, in everyday clinic, not all patients comply with the classic 3 steps. Most patients, who had a variety of previous treatment regimes, present to dermatologists only to search a method to maintain their disease on stationary stage. These types of patients have no regular step 1 to 3, just like most of the patients in our study. Till now, seldom data were provided for the patients of stationary stage.
A series of clinical studies have demonstrated that standard once daily application of calcipotriol/betamethasone dipropionate ointment could induce a rapid improvement of psoriasis vulgaris of active stage over 4-week treatment [11-13]. But these studies did not provide the regime to maintain the efficacy. The present study, focusing on patients of stationary stage, showed that a new regime of twice-weekly of the ointment produced a significant reduction of PASI and a high satisfaction degree after 1-month treatment. With the ongoing treatment till 3 month, the efficacy constantly increased and 90% patients were very satisfied with the treatment. During the period, another regime of once-weekly was also observed and PASI decreased to some extent. But only approximate 40% patients were satisfied with the treatment at the end of 3 month. According to previous study on atopic dermatitis patients, the concept of using twice-weekly regime is rationale [14]. The twice-weekly regime of topical agent could prevent flare and prolong flare-free intervals of chronic skin diseases.
Two previous studies applied calcipotriol/betamethasone ointment for 12 weeks on psoriasis patients [13-15]. The protocol was once-daily for 4 weeks followed by 8 weeks of the product at weekend alternating with calcipotriol at weekday. Another protocol was once-daily of the product for 8 weeks followed by 4-week of calcipotriol. Their protocols involved step 1 and step 2 of classic topical sequential therapy, but lacked step 3. Although good efficacies were observed in both protocols, the long-term maintenance data was absent. We suppose if our twice-weekly regime is applied to the patients, we would see long-term control of the disease. As our twice-weekly method enabled good compliance of the patients with less economic burden, less application frequency, less side effects and so on.
In our study, twice-weekly usage of calcipotriol/betamethasone ointment for 3 months did not develop obvious adverse events. In a long-term 52-week study, once-daily usage of the twocompound product was shown to be more safe and well tolerated than alternating 4-week periods of two-compound product and calcipotriol, or 4-week of two-compound product followed byctasia, striae distensae, acne, folliculitis, etc, which limit its’ long-term application [18]. Side effects of 48-week of calcipotriol [16,17]. Topical corticosteroid has the potential to cause skin atrophy, telangietopical calcipotriol include burning, pruritus, edema, peeling, dryness, and erythema [8]. Two-compound product containing corticosteroid and calcipotriol appears to have fewer side effects than either therapy alone, possibly because the two components neutralized each other’s adverse events. Present and previous data state that the two-compound product is safe for long-term management of psoriasis.
Although the 52-week once-daily treatment with calcipotriol/ betamethasone ointment achieved good efficacy of psoriasis vulgaris from active stage to stationary stage [17,18], the high expense of drugs and the anxiety of everyday use of corticosteroid would frustrate the compliance of some patients. We recommend our twice-weekly regime for everyday clinical practice in consideration of lower expense and better compliance of the patients.
In summary, treatment with calcipotriol/betamethasone dipropionate ointment twice-weekly was shown to be a clinically beneficial, well-tolerated and cost-effective method of long-term maintenance therapy for psoriasis vulgaris of stationary stage. Due to small sample size of short treating duration in the study, the conclusion needs further confirmation by studies with larger sample size and longer treatment duration.
References
- Greaves MW, Weinstein GD (1995) Treatment of psoriasis. New Engl J Med332:581-588.
- Dubertret L, Mrowietz U, Ranki A, Van de Kerkhof PC, Chimenti S, et al. (2006) European patient perspectives on the impact of psoriasis: the EUROPSO patient membership survey. Br J Dermatol155:729-736.
- Charakida A, Dadzie O, Teixeira F, Charakida M, Evangelou G, et al. (2006) Calcipotriol/betamethasone dipropionate for the treatment of psoriasis. Expert OpinPharmacother7:597-606.
- Langley RG, Gupta A, Papp K, Wexler D, Osterdal ML, et al. (2011) Calcipotriol plus betamethasone dipropionate gel compared with tacalcitol ointment and the gel vehicle alone in patients with psoriasis vulgaris: a randomized, controlled clinical trial. Dermatol222:148-156.
- Van Geel MJ, Mul K, Oostveen AM, Van de Kerkhof PC, De Jong EM, et al. (2014) Calcipotriol/betamethasone dipropionate ointment in mild-to-moderate paediatric psoriasis: long-term daily clinical practice data in a prospective cohort. Br J Dermatol171:363-369.
- Murphy G, Reich K (2011) In touch with psoriasis: topical treatments and current guidelines. J EurAcadDermatolVenereol25:3-8.
- Koo J (1999) Systemic sequential therapy of psoriasis: a new paradigm for improved therapeutic results. J EurAcadDermatolVenereol41:S25-S28.
- Koo JY (2007) Using topical multimodal strategies for patients with psoriasis. Cutis 79: 11-17.
- Koo J, Blum RR, Lebwohl M (2006) A randomized, multicenter study of calcipotriene ointment and clobetasol propionate foam in the sequential treatment of localized plaque-type psoriasis: short- and long-term outcomes. J Am AcadDermatol55:637-641.
- Paul C, Gallini A, Archier E, Castela E, Devaux S, et al. (2012) Evidence-based recommendations on topical treatment and phototherapy of psoriasis: systematic review and expert opinion of a panel of dermatologists. J EurAcadDermatolVenereol3:1-10.
- Douglas WS, Poulin Y, Decroix J, Ortonne JP, Mrowietz U, et al. (2002) A new calcipotriol/betamethasone formulation with rapid onset of action was superior to monotherapy with betamethasone dipropionate or calcipotriol in psoriasis vulgaris. ActaDermVenereol82:131-135.
- Papp KA, Guenther L, Boyden B, Larsen FG, Harvima RJ, et al. (2003) Early onset of action and efficacy of a combination of calcipotriene and betamethasone dipropionate in the treatment of psoriasis. J Am AcadDermatol48:48-54.
- Kragballe K, Noerrelund KL, Lui H, Ortonne JP, Wozel G, et al. (2004) Efficacy of once-daily treatment regimens with calcipotriol/betamethasone dipropionate ointment and calcipotriol ointment in psoriasis vulgaris. Br J Dermatol150:1167-1173.
- Reitamo S, Allsopp R (2010) Treatment with twice-weekly tacrolimus ointment in patients with moderate to severe atopic dermatitis: results from two randomized, multicentre, comparative studies. J Dermatol Treat 21:34-44.
- White S, Vender R, Thaci D, Haverkamp C, Naeyaert JM, et al. (2006) Use of calcipotriene cream (Dovonex cream) following acute treatment of psoriasis vulgaris with the calcipotriene/betamethasone dipropionate two-compound product (Taclonex): a randomized, parallel-group clinical trial. Am J ClinDermatol7:177-184.
- Kragballe K, Austad J, Barnes L, Bibby A, de la Brassinne M, et al. (2006) A 52-week randomized safety study of a calcipotriol/betamethasone dipropionate two-compound product (Dovobet/Daivobet/Taclonex) in the treatment of psoriasis vulgaris. Br J Dermatol154: 1155-1160.
- Kragballe K, Austad J, Barnes L, Bibby A, de la Brassinne M, et al. (2006) Efficacy results of a 52-week, randomised, double-blind, safety study of a calcipotriol/betamethasone dipropionate two-compound product (Daivobet/Dovobet/Taclonex) in the treatment of psoriasis vulgaris. Dermatol213:319-326.
- Menter A, Korman NJ, Elmets CA, Feldman SR, Gelfand JM, et al. (2009) Guidelines of care for the management of psoriasis and psoriatic arthritis. Section 3. Guidelines of care for the management and treatment of psoriasis with topical therapies. J Am AcadDermatol60:643-659.