- (2013) Volume 14, Issue 1
Julio Cesar Wiederkehr*, Barbara A Wiederkehr, Henrique A Wiederkehr and Caroline A Carvalho
Department of Surgery, Federal University of Paraná. Curitiba, Paraná, Brazil
Received September 10th, 2012 – Accepted October 16th, 2012
Context The elevation of serum amylase and lipase are generally associated with pancreatic diseases. However they can be associated with different pathologies unrelated with amylase and lipase. Case report This paper aims to report a case of a patient diagnosed with nonspecific hyperamylasemia and warn of this possibility in the differentiation of hyperamylasemia. Conclusion The correct diagnosis of silent hyperamylasemia is important in order to determine whether there is the risk of pancreatic disease or if we are just ahead of a benign hyperenzymemia.
Hyperamylasemia, Pancreas
CNPH: chronic pancreatic non-pathological hyperenzymemia
The elevation of serum amylase and lipase are usually associated with pancreatic diseases. A significant elevation of serum amylase with abnormalities in the pancreas is usually a manifestation of acute pancreatitis. However, this increase may also be related to pancreatic metabolic diseases and extrapancreatic abnormalities of the pancreatic ducts like recurrence of chronic pancreatitis, diabetic ketoacidosis and chronic viral liver disease [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]. There are still other reasons unrelated to the pancreas that are associated with this disorder, such as ectopic pregnancy, mumps, HIV infection and head trauma (Table 1) [8].

However, Gullo et al. [11] described in 1996 a new syndrome characterized by an asymptomatic state with elevated serum levels of pancreatic enzymes and absence of pancreatic diseases, by which it was called chronic pancreatic non-pathological hyperenzymemia (CNPH).
The cause of this hyperamylasemia is not clear. Some hypotheses report that may result from a defect in the secretion of enzymes by the basolateral surface of the acinar cells [12], causing an increase in the passage of enzymes into the bloodstream, or may also be caused by changes in the Wirsung conduct by secretin stimulation [11].
This paper aims to report a case of a patient diagnosed with nonspecific hyperamylasemia/CNPH, and warn of this possibility in the differential diagnosis of hyperamylasemia.
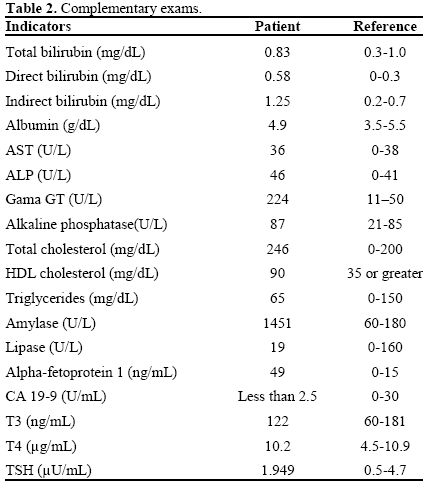
A 31-year-old female patient had nonspecific epigastric abdominal pain. She did not report weight loss and denied abdominal pain, cramping, diarrhea or vomiting. She denied previous episodes. The patient appeared to be in good condition, the abdomen was flat, flaccid and painless; bowel sounds were normal and had no visceromegaly. She denied use of drugs and/or alcohol. On admission laboratory tests were requested which were normal except for gamma-GT 224 U/L (reference range: 11-50 U/L) and amylase 1,451 U/L (reference range: 60-180 U/L) (Table 2) [13].
The abdominal ultrasonography showed no pancreatic abnormalities but showed two stones (about 3 and 5 mm) in both kidneys. MRI showed pancreas with normal texture and dimension.
The patient then underwent pancreatic arteriography and splenoportography in order to analyze the amylase concentrations of the head, body and tail of the pancreas (Figure 1). No differences were found between the amylase and lipase concentrations in the three different collection points (splenic hilum, head and body of the pancreas). The results are shown in Table 3. She has been followed up for more than two years with no symptoms at all.

cases of hyperamylasemia associated with pancreatic diseases are common in clinical practice. This dysfunction can also occur in situations such as kidney failure, brain trauma, traumatic shock, postoperative diabetic acidosis, renal transplants, pneumonia, pregnancy, prostate disease, mesenteric thrombosis and macroamylasemia.
However, when this serum amylase increase presents unrelated to other hyperenzymemias and with no significant symptoms, we should investigate the patient’s clinical history in order to assess a possible association between this increase and systemic diseases (Figure 2) [9], and also investigate the family history for familiar hyperamylasemia.
To characterize this disorder as chronic pancreatic or no pathological hyperenzymemia is also important to determine the behavior of this increase of pancreatic enzymes in a given space of time, as through a study of 42 patients with this syndrome [14], who had followed serum pancreatic enzymes concentrations for 5 consecutive days and had demonstrated that concentrations of these enzymes varied widely, including the periods of stabilization. In all 37 cases with available data abnormal high enzyme concentrations were associated with increase of the lipase and trypsin concentrations. In only three patients, the serum amylase was the only enzyme with high abnormal concentration. Furthermore, Gullo [14] advises that the benign pancreatic hyperenzymemia diagnosis can only be given after an observation period of with no symptoms and/or signs of pancreatic diseases and no structural changes of the organ during this period of time. Other authors [15, 16] have reported cases of families who had recorded extremely high levels of amylase which persisted for several generations without other symptoms.
This condition was called familiar hyperamylasemia, which was consistent with autosomal dominant inheritance pattern and genetics as a cause of this disorder. However, the most controversial debates are about the pancreatic steatosis. Gullo et al. [17] used magnetic resonance imaging to exclude this hypothesis as the cause of hyperamylasemia. Cavallini et al. [18] supported this hypothesis, because they found a significant increase in pancreatic echogenicity (considered as an index of pancreatic steatosis) in 80% of patients with hyperamylasemia compared with 29% of patients in the control group. Therefore, the literature has still not reached a consensus about the real cause of this syndrome.
The present patient had normal pancreatic texture both at ultrasonography and magnetic resonance. According to Hellerhoff et al. [19], i.v. administration of secretin induces the secretion of fluid and bicarbonate by the exocrine pancreas. Thus, ductal filling is increased, and visualization of the pancreatic tract is improved. Under such circumstances, Testoni et al. [20] supported that MRI with secretin stimulation is a known factor able to increase the detection of pancreatic duct abnormalities that may be associated with hyperenzymemia. However, it is not clear how these pancreatic ductal abnormalities can explain the high serum levels of pancreatic enzymes.
This test was not performed in the present case because it was not available in our center. The confirmation that all regions of the pancreas revealed high levels of pancreatic enzyme may exclude ductal abnormalities as the reason for hyperamylasemia.
In conclusion, the correct diagnosis of silent hyperamylasemia is important in order to determine whether there is the risk of pancreatic disease or if we are just ahead of a benign hyperenzymemia. Since CNPH shows no clinical consequences and had not a specific treatment, we should always alert to any symptoms.
The authors have no potential conflict of interest