- (2011) Volume 12, Issue 4
Haiying Cheng1, Eirini Merika2, Kostas N Syrigos3, Muhammad Wasif Saif1*
1Columbia University College of Physicians and Surgeons. New York, NY, USA
2Oncology Department, Imperial College Healthcare NHS Trust. London, United Kingdom
3Oncology Unit, Third Department of Medicine, Sotiria General Hospital. Athens, Greece
There are urgent needs to develop novel and more effective regimens to improve outcomes of pancreatic cancer given its dismal prognosis and limited treatment options. Several phase I clinical trials involving novel agents were recently presented at the 2011 American Society of Clinical Oncology (ASCO) Annual Meeting. It appears that hedgehog inhibition with IPI-926 was welltolerated and might be effective in treating pancreatic cancer when combined with gemcitabine. The survival benefits will be tested in the following randomized phase II trial. The new combination of gemcitabine and blockade of checkpoint kinases with AZD7762 showed an acceptable safety profile. Furthermore, inhibition of PI3K by BAY80-6946 was well tolerated with PET-CT suggesting reduction in FDG uptake in some pancreatic cancer. The benefits of above novel agents/regimens need to be further tested in phase II trials.
Adenocarcinoma; Clinical Trials, Phase I as Topic /adverse effects; Checkpoint kinase 1; checkpoint kinase 2; Hedgehog Proteins; Pancreatic Neoplasms; Protein Kinases; Protein-Serine-Threonine Kinases
Chk1, Chk2: checkpoint kinases 1 and 2; mTOR: mammalian target of rapamycin; PTCH: patched; SMO: smoothened
Pancreatic cancer remains to have dismal prognosis with mortality rate to be the same over past two decades [1]. Gemcitabine is still considered to be the standard chemotherapy for metastatic pancreatic cancer but the response rate was 5% and the median survival was only around 6 months. The addition of erlotinib to gemcitabine showed a small but significant improvement in survival. Recently, the oxaliplatin and irinotecan plus fluorouracil and leucovorin (FOLFIRINOX) trial demonstrated improved overall survival to 11.1 months although the regimen was quite toxic [2]. Novel agents are thus needed in the treatment of pancreatic adenocarcinoma.
This is an update from the recent 2011 American Society of Clinical Oncology (ASCO) Annual Meeting focusing on presentations regarding novel agents in phase I clinical trials in pancreatic adenocarcinoma. Four studies were reviewed: the first two discussed inhibition of hedgehog signaling, the third one included checkpoint kinase blocker and the last one evaluated the safety profile of a PI3K inhibitor.
Abnormal activation of hedgehog pathway has been implicated to play important roles in the development of multiple cancers, including pancreatic cancer. In normal cells of most adult tissues, the pathway is quiescent. In cancer cells, the hedgehog signaling is activated when hedgehog ligands bind to their receptor patched (PTCH), relieve the inhibitory effects of PTCH on the smoothened (SMO) receptor and subsequently activate the GLI family transcription factors which turn on genes to promote proliferation [3]. Alternatively, inactivating mutation in PTCH or activating mutation in SMO, such as in basal cell carcinoma, can lead to constitutive activation of signaling (Figure 1).
Hedgehog signaling is altered in almost all pancreatic cancers as suggested by global genetic analyses [4]. The aberrant hedgehog likely signals in a paracrine manner in pancreatic cancer with the bulk cancer cells secreting hedgehog ligands to activate the hedgehog pathways in stroma and cancer stem cells. The former may promote the formation of desmoplastic stroma which is an important component of tumor microenvironment and creates a barrier for effective drug delivery. The latter could facilitate the maintenance of cancer stem cells which may be involved in metastasis [3, 5].
IPI-926, a semisynthetic cyclopamine analogue, is an orally active and potent SMO inhibitor [6]. In an otherwise lethal and gemcitabine resistant mouse model of pancreatic cancer, IPI-926 was able to reduce formation of desmoplastic stroma and to increase tumor vascular density by blocking hedgehog signaling. Consequently, it facilitated the delivery of gemcitabine and prolonged survival [7]. GDC-0449 is another orally active SMO inhibitor and has been shown to have some clinical activities in advanced basal-cell carcinoma and medulloblastoma [8, 9]. Several phase I clinical trials involving hedgehog inhibitors were reported recently.
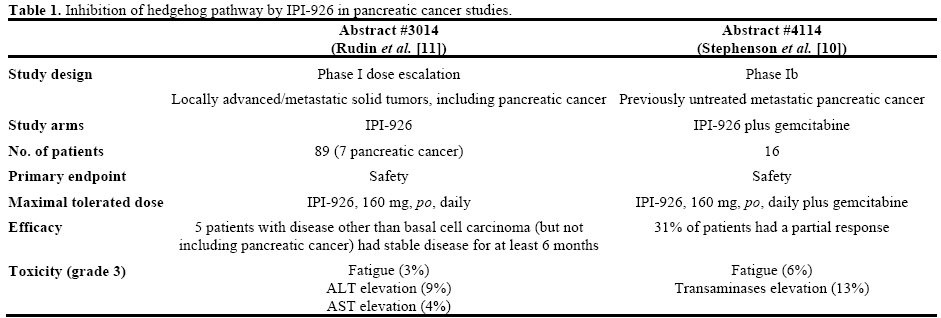
Stephenson et al. (Abstract #4114 [10]) presented their phase 1b study on utilizing IPI-926 plus gemcitabine as first line therapy for patients with metastatic pancreatic cancer. Sixteen patients with mean age of 69 years were included in the trial. Maximal tolerated dose of IPI-926 was determined to be 160 mg, given orally, once, daily along with gemcitabine, 1,000 mg/m2, given weekly, 3 weeks on and 1 week off. It is also the recommended phase II regimen on a 28-day cycle. In general, the combination of IPI-926 and gemcitabine were well-tolerated. IPI-926 related adverse events included fatigue, nausea, vomiting, transaminases elevation, decreased appetite, diarrhea, anemia, thrombocytopenia and peripheral edema. Among them, grade 3 toxicities for IPI-926 were fatigue and transaminases elevation. In addition, one patient developed microangiopathic hemolytic anemia related to gemcitabine and 63% of patients had dose reduction of gemcitabine mainly secondary to thrombocytopenia. No death or adverse events more than grade 3 were observed for the combined treatment. Furthermore, there was no pharmacokinetic interaction between IPI- 926 and gemcitabine. Regarding efficacy, 31% (5/16) of patients had a partial response. Additionally, 63% (10/16) of patients was noticed to have decreased CA 19-9. The randomized phase 2 portion of the study is actively recruiting patients with overall survival as its primary endpoint.
Rudin et al. (Abstract #3014 [11]) performed a phase I study utilizing IPI-926 as a single agent in a panel of advanced or metastatic solid tumors to determine its safety, pharmacokinetics, pharmacodynamics and antitumor activity. Among 89 patients, 7 of them had pancreatic cancer. Maximal tolerated dose of IPI-926 was 160 mg, once, daily on 28-day cycles. As a single agent, IPI-926 was well-tolerated. Most common IPI- 926 related adverse events (at least 10% of patients, mainly grade 1 or 2) were fatigue, ALT elevation, AST elevation, nausea, alopecia, dysgeusia, and muscle spasms. Grade 3 toxicities include fatigue and AST/ALT elevation. No grade 4 or 5 adverse events were reported. Reduction in GLI1 expression in normal skin was noticed for more than half of patients after IPI-926 treatment. Multiple partial responses were observed in patients with basal cell carcinomas. For patients with other solid tumors, 5 of them (not including patients with pancreatic cancer) were noticed to have stable disease for at least 6 months.
Table 1 summarizes the two studies of hedgehog pathway inhibition in pancreatic cancer that were presented in the 2011 ASCO Annual Meeting.
Chemotherapy and ionizing radiation could exert their anti-tumor activities by inducing DNA damages. In response to DNA damage, checkpoint kinases 1 and 2 (Chk1 and Chk2) are commonly activated to cause cell cycle arrest and facilitate effective DNA repair. Therefore, inhibition of Chk1/Chk2 could abrogate these checkpoints, impair DNA repair and subsequently potentiate the cytotoxic activities of DNAdamaging therapies [12].
Several inhibitors of checkpoint kinase are being tested in clinical trials, including AZD7762, a potent ATPcompetitive Chk1/Chk2 inhibitor [13]. Preclinical studies have suggested that AZD7762 could cause checkpoint abrogation and sensitize cancer cells to DNA-targeted treatments, including gemcitabine and radiotherapy [12].
Sausville et al. (Abstract #3058 [14]) conducted a phase I study of AZD7762 plus gemcitabine in patients with a panel of advanced solid tumors, including pancreatic cancer. Forty-two patients (mean age: 58 years) were included in the trial. AZD7762 (dose escalation 6-40 mg, i.v.) was first administered alone on days 1 and 8 during cycle 0, then a 7-day break, followed by AZD7762 in combination with gemcitabine (750 or 1,000 mg/m2 , i.v.) on days 1 and 8 on 21-day cycles. Maximal tolerated dose of AZD7762 was found to be 30 mg when given with gemcitabine 1,000 mg/m2. The most common adverse events were fatigue (n=17), nausea (n=11), neutropenia (n=11) and pyrexia (n=11). Among them, AZD7762 related grade 3 or higher toxicities included neutropenia (n=7) and hyperglycemia (n=3). In addition, two cardiac doselimiting toxicities were observed when AZD7762 was given alone during cycle 0: grade 3 asymptomatic elevated troponin I and grade 3 myocardial ischemia. Both resolved after stopping AZD7762. No significant pharmacokinetic interaction was noticed between AZD7762 and gemcitabine. Efficacy wise, two patients (both with NSCLC, gemcitabine naïve) had a partial response by the Response Evaluation Criteria In Solid Tumors (RECIST) criteria.
Mutations in K-ras oncogene are critical in the development of pancreatic ductal adenocarcinoma. The PI3K/AKT/mTOR pathway lies further downstream of the RAS family. It plays a key role in mediating effective alterations in a broad range of cellular function, such as cell growth, proliferation, motility, survival and intracellular trafficking in response to extracellular signals. The pathway is activated by ligands binding to tyrosine kinase receptors, such as insulin growth factor-1, which in turn activate PI3K. PI3K generates 3-phosphorylated phosphoinositides and activates AKT (protein kinase B/AKT) which in turn regulates various kinases, transcription factors and other regulatory molecules. This PI3/AKT pathway is involved in inhibition of apoptosis and stimulation of cell proliferation as well as glucose metabolism. Further downstream exists the mammalian target of rapamycin (mTOR), which is also activated in many cancers; it regulates translation of mRNA that codes for proteins involved in survival signals, acting as a promoter of cell proliferation and translation and growth and proliferation of cancer vascular endothelial cells. At least 50% of all cancers are related to deregulation of this pathway including pancreatic cancer. Its aberrant activation leads to inhibition of chemotherapy mediated apoptosis and similarly its inhibition has been associated with anti-tumor effects in pre-clinical studies and may be used as a potential therapeutic target in many cancers such as breast , renal, ovarian and of course pancreatic [15, 16, 17].
Evidence suggests that PI3K may serve as a target for drug development. Wortmannin and LY294002 are molecules which disrupt the ATP binding pocket of PI3K and have been shown to induce growth inhibition and apoptosis [18, 19]. They have been tested in ovarian cancer cells in the murine peritoneum and in fact LY294002 in addition to paclitaxel proved more efficacious than the latter alone [20]. BAY 80-6946 is a potent and highly selective reversible class I PI3K inhibitor. Class I PI3Ks catalyse the conversion of phosphatidylinositol-3,4-bisphosphate to phosphateidylinositol- 3,4,5-triphosphate. The latter is undetectable in resting cells but abundant in highly active cells and modulates AKT activation.
Patnaik et al. (Abstract #3035 [21]) have studied the safety profile, pharmacokinetic properties, pharmacodynamic and potential efficacy of this compound in a panel of advanced solid tumors in the context of a phase I open-label trial. Seventeen non-diabetic patients with various solid tumors, among which three with pancreatic cancer, were included in the study population. Tumor specific pharmacodynamic were assessed using FDG-PET/CT. The maximal tolerated dose was defined to be 0.8 mg/kg intravenously on a weekly basis for 3 weeks every four weeks. Hyperglycemia was encountered in 6 of 7 patients receiving the maximal tolerated dose. Acute left ventricular failure with lactic acidosis, liver dysfunction and renal insufficiency and severe hyperglycemia limited dose escalation and were observed in one patient. Acute hypertension was attributed to treatment on one occasion. The most frequent adverse events reported included: fatigue, nausea, vomiting, alopecia, diarrhea, mucositis and dysgeusia as well as anemia. Disease stabilization was observed for up to 8 months for endometrial cancer (no data available for pancreatic arm). FDG uptake was reduced by 23% in a liver of a pancreatic patient. Their results were consistent with effective exposure to the drug and PI3K inhibition.
There are urgent needs for developing novel agents in pancreatic cancer given its dismal prognosis and limited treatment options. Here we review four phase I clinical trials chosen from a number of studies containing new therapeutics that were presented in the 2011 ASCO Annual Meeting.
Inhibition of hedgehog pathway by IPI-926, an oral SMO inhibitor appears to have acceptable toxicity profiles either alone or in combination with gemcitabine [10, 11]. In addition, when combined with gemcitabine, IPI-926 demonstrated some promising clinical efficacy in treating pancreatic cancer [10]. The randomized phase II portion of that trial is actively enrolling patients to evaluate whether addition of IPI 926 to standard gemcitabine regimen could prolong survival in metastatic pancreatic cancer. By targeting tumor microenvironment (desmoplasia) and cancer stem cells, the hedgehog inhibitors could potentially not only improve drug delivery to malignant cells but also diminish further systemic metastasis [3]. Despite the exciting hypotheses, many questions remain to be answered. One study used skin GLI1 level as a pharmacodynamic biomarker to assess hedgehog signaling inhibition [11]. It would be interesting to know whether this is a validated marker and whether it associates with antitumor activities. Furthermore, given that pancreatic cancer is an extremely complex and heterogeneous disease entity, is it possible that we could identify biomarkers to predict which population may benefit the hedgehog inhibitors most? It would also be reasonable to test the efficacy of combinations of hedgehog inhibitors and other cytotoxic agents, such as cisplatin, in the context that we now may have a tool for better drug delivery. Nevertheless, the phase II study would first shed some light on whether there is survival benefit from the combined hedgehog inhibitors and gemcitabine.
Concerning checkpoint kinase inhibition, the maximal tolerated dose of the dual Chk1/Chk2 inhibitor, AZD7762 in combination with gemcitabine was determined. It was found that the agent was associated with some interesting adverse events. In particular, it may be worthwhile investigating the mechanisms underlying its cardiac toxicity. It is unclear whether it has additional anti-tumor activity when combined with gemcitabine from current phase I study. Therefore, a carefully designed phase II trial that contains a placebo arm is needed to clarify its benefit in pancreatic cancer. All members if the PI3K related kinases (PIKK) have been implicated in human cancer, both as oncogenes and tumor suppressor genes. Evidence supports the role of the PI3K/AKT/mTOR pathway in pancreatic carcinogenesis and that the pathway may be amenable to pharmacological manipulations. The BAY 80-6946 is among a series of awaited investigational oncology compounds by BAYER and is among the first PI3K inhibitors to be tested in humans. Its side-effect profile was limited and the most common side effect, hyperglycemia, is amenable to early detection and treatment. Hyperglycemia is thought to occur because AKT is a key regulator of glucose metabolism as it targets the insulin receptor substrate [22]. So perhaps selective inhibition of upstream PI3K isoforms as some may be preferentially involved in insulin signaling or keeping structural resemblance to the insulin receptor to a minimum might help minimize hyperglycemia. The kinase component of the PI3K pathway seems to be the most promising target for the development of new therapeutic drugs. Lots of questions remained unanswered such as where along the pathway are we more likely to gain therapeutic benefit while minimizing toxicity. Would targeting activating substrates or their regulatory subunits have the same effects? Functional specialization of PI3K subunits/isoforms suggests that selective inhibition with acceptable toxicity might be possible. Further research into identifying activating mutations of the PI3K pathway is needed as this may also serve as a potential gene target or identifying molecules which are implicated into the metastatic phenotype, promoting cell migration and cell adhesion (gene amplification has been observed in gastric adenocarcinoma). It remains to be seen whether genetic or pharmacologic blockage of these pathways would improve the clinical outcome wither when used alone or in combination with other targeted agents for the treatment of cancer.
In conclusion, with better understanding the pathogenesis of pancreatic adenocarcinoma, novel agents are being developed and tested in clinical trials. Some of them have shown reasonable safety profile as presented in the 2011 ASCO Annual Meeting. Phase II trials are needed to prove their clinical efficacy.
The authors have no potential conflicts of interest