Keywords
Hand, Hygiene, Compliance, Infection, Prevention, Tamale, Ghana
Introduction
Hospital-acquired infection is one of the current public health
problems the world is engulfed with, and the way forward is
competent Infection Prevention and Control (IPC) compliance
[1]. According to Trampuz and Widmer, thousands of people
die every day in the world from nosocomial infections acquired
through health care procedures through contaminated hands
[2]. The influential factors involved in the menace of nosocomial
infections in our healthcare backgrounds is poor hand hygiene
compliance among healthcare providers [3].
According to Mathur's study, the most competent, easiest, and
cost-efficient technique of infection prevention and control is hand
hygiene compliance [4]. Even though hand hygiene compliance is
the way for the prevention of nosocomial infection in our healthcare
environment, studies have shown that healthcare workers inclusive
nurses do not comply with hand hygiene half the number of times
they are supposed to and this has contributed to HAI increase [5].
The hand of the healthcare worker is acknowledged as the highest
route for the spread of exogenous infections mostly through
invasive procedures [6]. Promoting hand hygiene compliance
should be significant for health authorities and all healthcare
facilities at all levels, in addition to the individual responsibility
of each health provider [5]. The World Health Organization has
recommended five key moments for hand hygiene in health
practice: before contact with a patient, before an aseptic
procedure, after contact with a patient, after contact with body
fluids, and after touching a patient's surroundings [6].
Nakamura and Tompkins's study has revealed that about 5 to
10.0% of all admitted patients develop nosocomial infections and
70.0% of the identified pathogens are resistant to one or more of
the antimicrobial medicine currently in use [7].
Sub-Saharan African countries including Ghana records a
high prevalence rate of HAI, ranging from 2.0 – 49.0%; this is
particularly high among critically ill patients admitted to the noncritical
intensive unit where the rate is projected to range from
21.2 - 35.6%. A survey in Ghana reported a national prevalence
rate of 8.2% and 8.0% for Tamale Teaching Hospital [8].
A study by Labi, et al. on hand hygiene compliance among
healthcare workers in the Northern Region (Kpandai and Tatale-
Sanguli), indicated hand hygiene compliance of 49.6% for preintervention
and final compliance of 67.9% after interventions
such as such training on IPC [9]. The current emphasized need
for hand hygiene practice due to the pandemic of Severe Acute
Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) commonly
known as Covid-19 necessitated this study to assess hand
hygiene compliance among nurses working in the paediatric
department of Tamale Teaching Hospital. Since nurses form a
major proportion of the health care providers and constitute the
“nucleus of the health care system” [10,11]. Because they occupy
more time with patients than any other healthcare provider, their
compliance with hand hygiene guidelines gives the impression to
be more vital in preventing nosocomial infection among patients.
Research Design
A descriptive cross-sectional study was adopted for this study,
using the method of observation for quantitative data.
Study Participants and Setting
The study participants of this study were all nurses working in the
pediatric department of Tamale Teaching Hospital. At the time of
the study the average number of nurses for the department was
107 with average patient population of 130. Serious variation in
patient count is affected by seasonal variation. The total number
of nursing staffs are divided across the days and various shifts.
Also, staff’s duty offs and leaves affects the total staff strength.
Tamale Teaching Hospital is a major referral teaching hospital
in the northern regional capital of Ghana. It serves as the main
referral hospital for five northern regions of Ghana, including the
neighboring countries to the north of Ghana.
Data Collection Tool
The world health organization checklist for five moments of hand
hygiene in the healthcare facility was adopted for this study. The
checklist was adopted and modified to suit the objectives of the
study. The checklist was divided into demographic characteristics
of the participants, such as ward of the observation, day shift of
the observation, category, or rank of nurse observed. Moment of
hand hygiene opportunity, hand hygiene action (handwashing,
hand rub, or missed opportunity).
Data Analysis
Data analysis was done using SPSS version 20. Categorical
variables like respondents’ sex, and practice level analysis were
presented as frequencies and percentages using tables and
figures. The hand hygiene compliance level in the department
was calculated by dividing the number of present hand hygiene
actions (handwashing, hand rub with hand sanitizer, and both)
by total hand hygiene indications and multiplying it by 100. The
bivariate analysis was done using Chi-square to determine factors
associated with hand hygiene compliance and multivariate
analysis for prediction done using binary logistics regression.
Results
Demographic characteristics of study participants
The study recorded a total of 410 observations. From the
observation majority (51.0%) of the study observations were
females and most (69.0%) of them were within the age bracket
of 30 – 39 years. In terms of occupational categorization, most
(85.1%) of the observations were on registered general nurses.
The majority (38.3%) were from the neonatal intensive care unit
(NICU), 32.0% from the children's emergency ward (CEW), and
29.8% from the main pediatric ward. Most of the observations
were done during the working day of the week and most (46.8%)
were done during the morning shifts (Table 1).
Table 1: Demographic characteristics of study participants.
| |
Frequency |
Percentage |
| Sex |
Male |
201 |
49.0 |
| Female |
209 |
51.0 |
| Estimated age group |
18 - 29 years |
107 |
26.1 |
| 30 - 39 years |
283 |
69.0 |
| 40 - 49 years |
10 |
2.4 |
| 50 - 59 years |
10 |
2.4 |
| Category of nurse |
RGN |
349 |
85.1 |
| RM |
29 |
7.1 |
| Enrolled nurse |
32 |
7.8 |
| Ward |
Paediatrics ward |
122 |
29.8 |
| CEW |
131 |
32.0 |
| NICU |
157 |
38.3 |
| Day of the work |
Working day |
350 |
85.4 |
| Weekend |
60 |
14.6 |
| Duty shift |
Morning |
192 |
46.8 |
| Afternoon |
132 |
32.2 |
| Night |
86 |
21.0 |
Source: an observational study, 2020.
Hand hygiene compliance level
Out of the 410 indications for hand hygiene compliance, hand
hygiene was present or done for 329 indications and not done for
81 indications. Hence the hand hygiene compliance level recorded
from observation was 80.2% and 19.8% for no compliance.
The dominant (47.3%) hand hygiene action was hand washing;
hand washing was high (68.4%) when it came to after touching a
patient indication. The second most (17.3%) hand hygiene action
was hand rub with hand sanitizer, hand rub was high (39.3%)
after touching patient surroundings. Hand hygiene action missed
was high (40.2%) before touching the patient's surroundings.
From observation, gloves were used in 77.8% of the indications.
The observation indicated that hand hygiene was only practiced
8.8% before glove use and 96.9% after glove use.
Factors associated with hand hygiene compliance
Chi-square analysis revealed a statistically significant relationship
between the professional nursing category and hand hygiene
compliance, X2 (2, 410) = 49.76, P ≤ 0.001. However, with age and
sex, there was no significant relation to hand hygiene compliance.
Chi-square analysis revealed statistical significant relationship
between Wards of the pediatric department, X2 (2, 410) = 12.24,
P = 0.002, day of the week, X2 (2, 410) = 7.596 P = 0.006,
shift of the day, X2 (1, 410) = 57.882, P ≤ 0.001 and presence of
hand hygiene compliance (Table 2).
Table 2: Chi-square analysis of factors and hand hygiene compliance.
| |
Observed hand hygiene compliance |
|
|
|
| Present |
Absent |
X2 |
df |
P-value |
| Sex |
Male |
157 |
78.1% |
44 |
21.9% |
1.133 |
1 |
.287 |
| Female |
172 |
82.3% |
37 |
17.7% |
- |
- |
|
| Estimated age group |
< 30 years |
86 |
80.4% |
21 |
19.6% |
0.02 |
1 |
.969 |
| ≥ 30 years |
224 |
79.2% |
59 |
20.8% |
- |
- |
- |
| Category of nurse |
RGN |
290 |
83.1% |
59 |
16.9% |
49.769 |
2 |
.000 |
| RM |
9 |
31.0% |
20 |
69.0% |
- |
- |
- |
| Enroll nurse |
30 |
93.8% |
2 |
6.2% |
- |
- |
- |
| Ward |
Paediatrics |
85 |
69.7% |
37 |
30.3% |
12.244 |
2 |
.002 |
| CEW |
111 |
84.7% |
20 |
15.3% |
- |
- |
- |
| NICU |
133 |
84.7% |
24 |
15.3% |
- |
- |
- |
| Day of the work |
Working day |
273 |
78.0% |
77 |
22.0% |
7.596 |
1 |
.006 |
| Weekend |
56 |
93.3% |
4 |
6.7% |
- |
- |
- |
| Duty shift |
Morning |
181 |
94.3% |
11 |
5.7% |
57.882 |
2 |
.000 |
| Afternoon |
100 |
75.8% |
32 |
24.2% |
- |
- |
- |
| Night |
48 |
55.8% |
38 |
44.2% |
- |
- |
- |
| Hand hygiene materials available |
Water and Soap |
78 |
68.4% |
36 |
31.6% |
13.923 |
1 |
.000 |
| Water and soap plus hand sanitizer |
251 |
84.8% |
45 |
15.2% |
- |
- |
- |
Source: an observational study, 2020.
Indicators for hand hygiene and hand hygiene
compliance
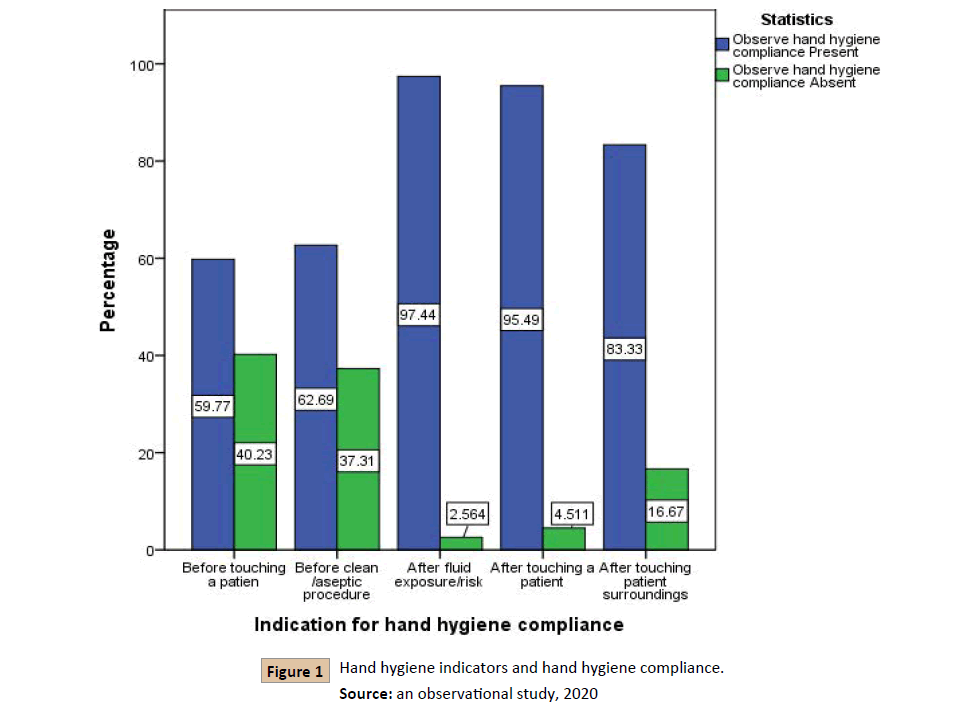
Chi-square analysis indicated a significant relation between WHO
five moments hand hygiene indicators and actual hand hygiene
compliance, X2(4, 410) = 63.307, P ≤ 0.001. Proportionally after body
fluid exposure hand hygiene indicator recorded the highest (97.4%)
hand hygiene compliance, next was after touching a patient (95.5%),
then after touching the patient environment (83.3%), after that, was
before the clean or aseptic procedure and finally and least (59.8%)
complied indicator was before touching a patient (Figure 1).
Figure 1: Hand hygiene indicators and hand hygiene compliance.
Source: an observational study, 2020
Multiple logistics regression of factors
associated with hand hygiene non-compliance
The ward of the participant predicted hand hygiene noncompliance,
those in CEW were about 60% less likely to noncritical comply with hand hygiene as compared to those in the pediatric
ward (AOR = 0.4, 95%, C.I. 0.162 – 0.890). Also, the shift of the day
predicted hand hygiene non-compliance, those on the afternoon
shift were three times likely to non-comply with hand hygiene
as compared to those on the morning shift (AOR = 3.1, 95%, C.I.
1.172 – 7.980). And those on the night shift were almost nine
times likely to non-comply with hand hygiene as compared to
those on the morning shift (AOR = 8.6, 95%, C.I. 3.147 – 23.359).
The occupational of participant predicted hand hygiene noncompliance,
registered midwives were about 53 times likely
to non-comply with hand hygiene as compared to registered
general nurses (AOR = 53, 95%, C.I. 11.324 – 252.019). Finally,
the type of hand hygiene indication predicted hand hygiene noncompliance.
Comparing hand hygiene before touching patient,
non-compliance with the other hand hygiene indicators were
less likely, hand hygiene after fluid exposure (AOR = 0.05, 95%,
C.I. 0.005 – 0.510), after patient touch (AOR = 0.06, 95%, C.I.
0.021 – 0.199) and after touching patient surroundings (AOR =
0.4, 95%, C.I. 0.161 – 0.941) (Table 3).
Table 3: Binary logistics regression for predictors of hand hygiene non-compliance.
|
B |
Wald |
Sig. |
AOR |
H-L GOF test
X2 (8)= 14.297, P =0.074
95% C.I. for AOR |
| Lower |
Upper |
|
Paediatrics ward |
|
|
Ref |
|
|
|
| CEW |
-.969 |
4.968 |
.026 |
.379 |
.162 |
.890 |
| NICU |
-1.134 |
2.871 |
.090 |
.322 |
.087 |
1.195 |
Day of the
Work (weekend / Working day) |
-.572 |
.868 |
.352 |
.564 |
.169 |
1.881 |
| Morning |
|
|
Ref |
|
|
|
| Afternoon |
1.118 |
5.219 |
.022 |
3.058 |
1.172 |
7.980 |
| Night |
2.149 |
17.658 |
.000 |
8.574 |
3.147 |
23.359 |
| RGN |
|
|
Ref |
|
|
|
| RM |
3.978 |
25.264 |
.000 |
53.423 |
11.324 |
252.019 |
| EN |
-.384 |
.203 |
.653 |
.681 |
.128 |
3.622 |
| Before touching a patient |
|
|
Ref |
|
|
|
| Before clean /aseptic procedure |
-.364 |
.641 |
.423 |
.695 |
.285 |
1.694 |
| After fluid exposure/risk |
-3.014 |
6.365 |
.012 |
.049 |
.005 |
.510 |
| After touching a patient |
-2.750 |
22.583 |
.000 |
.064 |
.021 |
.199 |
| After touching the patient surroundings |
-.944 |
4.391 |
.036 |
.389 |
.161 |
.941 |
| Hand hygiene material availability |
-.530 |
1.917 |
.166 |
.589 |
.278 |
1.246 |
Source: an observational study, 2020.
The logistic regression model appropriately explained the
outcome variable (hand hygiene compliance) since the Hosmer-
Lemeshow goodness-of-fit test p-value was more than 0.05,
(X2(8) = 14.297, p = 0.074) (Table 3), hence the model fits the
study data (Table 3).
Discussion
The study recorded a total of 410 observations, about 32.4% of
them were on after touching a patient, then 21.2% were on before
touching a patient, and least was on after body fluid exposure. The
majority (47.3%) of actions taken for hand hygiene compliance
was hand washing, then 17.3% for hand rub with hand sanitizer.
About 15.6% of actions for hand hygiene were both handwashing
and hand rub with hand sanitizer. However, there was a missed
action of 19.8% for hand hygiene opportunities. Also in a similar
study, the most (63.6%) preferred method of hand hygiene was
washing with water and soap [12]. Healthcare workers ought to
embrace either one procedure for hand hygiene, thus alcohol
hand-rub or handwashing with antimicrobial or non-antimicrobial
soap, but hand washing is recommended if the hands are dirty.
The usage of both procedures concurrently is not endorsed, as it
doubles both cost and time.
From observation, gloves were used in 77.8% of the indications.
The observation indicated that hand hygiene was only practiced
8.8% before glove use and 96.9% after glove use. Appropriate
hand hygiene is essential before wearing gloves, as trapped
moisture under gloves can be a source of skin irritation and
upsurge the harboring of bacteria.
A recent study in the surgical department of TTH by Alhassan et
al. on hand hygiene and facemask compliance among healthcare
providers reported a below-average number of participants
complying with hand hygiene [13]. However, in this current hand
hygiene compliance level recorded from observation was 80.2%
and 19.8% for non-compliance. In Ghana, a study in Cape Coast
Teaching Hospital indicated a low hand hygiene compliance
thus, 27.3% [13]. Also, in Ethiopia, an observational study on
hand hygiene compliance among healthcare workers revealed
overall compliance of 22.0% among the health care workers [14].
This study finding is still very high when compared to another
observational study in Istanbul, Turkey using a sum of 704 hand
hygiene opportunities observed from the neonatal and pediatric
intensive care units in Marmara University, Pendik Training and
Research Hospital, from June 2013 to July 2013, rather a low hand
hygiene compliance of 37.0% (261/704) among the healthcare
workers [12].
The current study revealed a statistically significant relationship
between the professional nursing category and hand hygiene
compliance. Registered midwives predicted hand hygiene
compliance for about 53 times likely as compared to registered
general nurses, this is in line with another study where compliance
varied by occupation [12]. However, in another study, there was
no difference in hand hygiene compliance among professional
groups [15,16].
This study revealed a significant relationship between wards
of the department, those in CEW were about 60% less likely
to non-comply with hand hygiene as compared to those in the
pediatric ward. NICU and CEW are perceived to be busy wards
of the department, so would have been expected that the higher
workload will result in low hand hygiene compliance as compared
to the pediatric ward. Since in a similar study in Ghana workload
was a factor related to poor hand hygiene compliance [17].
Day of the week was significantly related to hand hygiene
compliance; compliance was high (93.3%) during weekends as
compared to 8.0% for working days. Even though this did not
predict hand hygiene compliance at the multivariate analysis,
this is expected as working days are usually the busy days hence
the likelihood of non-compliance. The shift of the day was also
related to compliance, those on the morning shift were more
likely to comply with hand hygiene as compared to those on
the night. Hand hygiene non-compliance was highly predicted
by the night shift as those on the night were about nine times
likely to non-comply as compare to those on the morning shift.
Also, those on the afternoon shift were about three times likely
to non-comply as compared to those in the morning. More
compliance for the morning shift can be related to the fact that
day time duties are usually associated with the availability of
working materials. Meanwhile, in another study, there was no
difference in hand hygiene compliance among different shifts of
the day [15].
Finally, the study revealed a significant relation between WHO
five moments hand hygiene indicators and actual hand hygiene
compliance. Comparing hand hygiene before touching a patient,
non-compliance with the other hand hygiene indicators were less
likely. Hand hygiene non-compliance was only likely 0.05 times
after fluid exposure. Hand hygiene non-compliance was likely
only 0.06 times after patient touch. And after touching patient
surroundings non-compliance was only likely for about 40%. In
Ethiopia, an observational study on hand hygiene compliance
among healthcare workers revealed hand hygiene compliance
was higher after body fluid exposure 75.8% and better for
after-patient contact 42.8%. However lower for before patient
contact 2.4%, before a clean or aseptic procedure 3.6%, and
after contact with patient surroundings 3.3% [15]. Also in
study, the level of compliance relative to WHO five moments of
hand hygiene was: overall compliance before patient contact
was 43.2%, before a clean/aseptic procedure was 8.5%, after
body fluid exposure was 18.1%, after contact with patients
was 68.1%, and after contact with patient surroundings was
43.2% [12].
Limitation
This study is not without limits; the study was unable to explore
all factors known to be associated with hand hygiene compliance.
Conclusion
The study recorded very good hand hygiene compliance among
the nurses. The factor that predicted non-compliance included:
the ward of the department, the shift of the day, the occupational
category of the nurse observed, and the kind of hand hygiene
indicator.
Ethical Consideration
Permission for data collection from the hospital-acquired through
the research department of Tamale Teaching Hospital. Since
this is an observational study participants were not informed.
All sources for information used in this research were duly
acknowledged to avoid any form of plagiarism.
Data Availability
All dataset related to the findings of this study is available with
the submitting author.
Conflicts of Interest
There is no conflict of interest with this submission.
Funding Statement
Funding for this study was completed by the author without any
external funding.
References
- Sarani H, Balouchi A, Masinaeinezhad N, Ebrahimitabas E (2015) Knowledge Attitude and Practice of Zabol University of Medical Sciences (2014). Glob J Health Sci.
- Trampuz A, Widmer A (2004) Hand Hygiene: A frequently missed lifesaving opportunity during patient care. Mayo Clin Proc79: 109-16.
- Jain M, Dogra V, Mishra B, Thakur A, Loomba PS (2012) Infection control practices among doctors and nurses in a tertiary care hospital. Ann Trop Med Public Health 5: 29-33.
- Mathur P (2011) Hand hygiene: Back to the basics of infection control. Indian J Med Res 134: 611–20.
- CDC (2017) CDC Features Centers for Disease Control and Prevention.
- WHO (2009) WHO Guidelines on Hand Hygiene in Health Care: a Summary. Geneva: World Health Organisation.
- Nakamura RK, Tompkins E (2012) Nosocomial Infection. Compendium.
- Labi AK, ObengNkrumah N, Owusu E, Bjerrum S, Bediako-Bowan A (et al). (2018) Hospital-acquired infections in Ghana. J Hosp Infect 1-34.
- Labi AK, ObengNkrumah, N, Nuertey BD, Issahaku S, Ndiaye NF, et al. (2019) Hand hygiene practices and perceptions among healthcare workers in Ghana: A WASH intervention study. J Infect Dev Ctries.
- Buerhaus PI, Auerbach DI, Staiger DO (2007) Recent trends in the registered nurse labor market in the US: short-run swings on top of long-term trends. Nurs Econ 25: 59-66.
- American Association of Colleges of Nursing (2019) Nursing Fact Sheet. American Association of Colleges of Nursing.
- Karaaslan A, Kadayifci EK, Atıcı S, Sili U, Soysal A, et al. (2014) Compliance of Healthcare Workers with Hand Hygiene Practices in Neonatal and Pediatric Intensive Care Units: Overt Observation. Interdiscip Perspect Infect Dis 1-5.
- Alhassan AR, Kuugbee E, Der E (2020) Surgical Healthcare Providers’ Compliance to Hand Hygiene and Facemask Use: A Case of Tamale Teaching Hospital Ghana. J Prev Infec Contr 6: 4:51.
- Engdaw GT, Gebrehiwot M, Andualem Z (2019) Hand hygiene compliance and associated factors among health care providers in central Gonder zone public primary hospitals, Northwest Ethiopia. Antimicrob Resist Infect Control 8: 1-7.
- Kolola T, Gezahegn T (2017) A twenty-four-hour observational study of hand hygiene compliance among health care hospital Ethiopia. Antimicrob Resist Infect Control 1-5.
- Ghana Statistical Service (2010) population and housing census district analytical report: Tamale Metropolis. Accra: Ghana Statistical Service 2014.
- Amissah I, Salia S, Craymah JP (2016) A Study to Assess Hand Hygiene Knowledge and Practices among Healthcare Workers in Teaching Hospital in Ghana. IJSR 5.