Review Article - (2024) Volume 10, Issue 5
Nursing Role for Intra-abdominal pressure (IAP) Monitoring in Critical Care of Adult Patients: Scoping Review
Amnah Mohammed Howthan*
Master Degree of Medical Surgical Nursing, King Saud Medical City, Saudi Arabia
*Correspondence:
Amnah Mohammed Howthan,
Master Degree of Medical Surgical Nursing, King Saud Medical City,
Saudi Arabia,
Email:
Received: 09-Sep-2024, Manuscript No. ipjicc-24-21483;
Editor assigned: 11-Sep-2024, Pre QC No. ipjicc-24-21483 (PQ);
Reviewed: 25-Sep-2024, QC No. ipjicc-24-21483;
Revised: 30-Sep-2024, Manuscript No. ipjicc-24-21483 (R);
Published:
07-Oct-2024, DOI: 10.35248/2471-8505-10.05.41
Abstract
Background: Monitoring Intra-abdominal Pressure (IAP) was crucial for managing critically ill patients since high IAP could result in serious consequences such as Intra-abdominal Hypertension (IAH) and Abdominal Compartment Syndrome (ACS). Despite its importance, critical care nurses have significant gaps in their knowledge and practices surrounding IAP monitoring.
Aim: This scoping review aimed to evaluate the state of IAP monitoring in critical care settings, focusing on the role of critical care nurses and identifying the challenges they faced in recognizing and managing IAH and ACS.
Methods: A systematic search of the literature was undertaken using databases such as PubMed and Google Scholar, adhering to the PRISMA criteria to guarantee a robust review process. Studies were chosen based on their relevance to critical care nurses’ roles in IAP monitoring in critically ill adult patients, as well as their publication date (2020- 2024) and study design.
Results: The analysis found a lack of defined techniques and training for assessing IAP. While trans-vesical measurement was widely employed, there was significant diversity in measuring methodology and the prevalence of IAH and ACS between investigations. Many critical care nurses expressed feelings of inadequacy in their knowledge of IAP monitoring, citing constraints such as a lack of resources and clinical support.
Conclusion and recommendations: The findings highlighted the urgent need for improved critical care nurse training programs to improve their awareness of IAP monitoring procedures. Standardized protocols were proposed to ensure consistency in practice across critical care settings. Investing in technology that allows more accurate and less invasive IAP monitoring was also recommended. Finally, ongoing study into the effectiveness of IAP evaluation approaches was regarded critical for improving patient outcomes.
Keywords
Intra-abdominal pressure; Critical care nursing; Intra-abdominal hypertension; Abdominal compartment
syndrome; Patient outcomes; Nursing education; Monitoring techniques
Introduction
Critical care Patients are at high risk for significant health issues
that can lead to death. Critically sick patients require more
rigorous nursing care and monitoring [1]. Critical care patients
have consequences such as Intra-abdominal Pressure (IAP)
and abdominal compartment syndrome, which requires quick
diagnosis and treatment, high IAP levels can impact organ
perfusion and function [2].
Intra-abdominal Pressure (IAP) is defined as a steady-state
pressure within the abdominal cavity. It is determined by the
elasticity of the abdominal wall and the properties of the
abdominal contents [3]. Intra-abdominal Hypertension (IAH)
and Abdominal Compartment Syndrome (ACS) are not new
issues for critical care patients, as early as the nineteenth
century, IAH was detected and ACS was described, although
these were not called until more recent times [2]. The
prevalence of Intra-abdominal Hypertension (IAH) in the Intensive Care Unit (ICU) is high at over 50%. Studies have
found that 20%-30% of critically sick patients present to the
ICU with IAH, which increases to 30%-55% during their ICU stay
[4].
Intra-abdominal pressure monitoring is commonly used in
clinical practice because it is a safe, accurate, cost-effective,
and quick way to diagnose Intra-abdominal hypertension [5].
Both levels of increased Intra-abdominal tension have been
shown to produce considerable morbidity and mortality in
critically ill patients, this involves acute renal failure, pulmonary
impairment, and decreased blood supply to the gastrointestinal
organs [6]. IAP is described as pressure within the abdominal
cavity that is proportional to the respiratory phase and
abdominal wall resistance [7]. However, it has not been tested
for safety and reliability in the ICU. As a result, alternative
procedures that are less invasive have been developed. IAP can
be determined by measuring bladder pressure (with a Foley
catheter), stomach pressure (with a nasogastric or gastrostomy
tube), rectal pressure (with a balloon catheter), and inferior
vena cava pressure [7]. Transurethral measurement stood
out among these measurements due to its simplicity,
reproducibility, consistency, and low cost. The bladder is a
passive reservoir, which appropriately reflects IAP [7].
Clinical assessment of IAP based on palpation of the abdomen
is inaccurate, and clinically significant IAH can be present in
the absence of abdominal distension [8]. In critical care, IAP
measurements through the bladder or stomach are the most
practicable, and intravenous IAP measurement is considered
the gold standard [9].
Improved IAP assessment allows for more effective monitoring
and management of patients with IAH or ACS. Accurate IAP
measurement is crucial for managing patients with IAH and ACS,
IAP can be measured directly intra peritoneally or indirectly
through a hollow viscus (e.g. bladder, stomach, rectum, or
uterus) [10]. Clinical examination of IAP is inconsistent, with
a sensitivity ranging from 40% to 60%. IAP is thus most usually
estimated using urinary bladder pressure, which is measured
via a manometer attached end-to-side to a urinary catheter,
allowing for intermittent bladder pressure monitoring while
momentarily impeding urine flow [11].
Some systems support the use of a pressure sensor by
introducing a needle into the system to detect pressure,
whilst others employ a column of fluid to measure pressure
mechanically [11]. IAP measurement using intravenous
pressure is easy, consistent, reproducible, and minimally
invasive because the majority of relevant patients require
urinary catheterization for other purposes [11]. IAH increases
morbidity and mortality rates among severely ill individuals, the
limited space and close contact with bordering cavities impair
the function of Intra-abdominal organs, as well as causing
physiological changes and malfunction of organs outside the
abdominal cavity [1].
Common physiological measures such as blood pressure,
electrocardiography, heart rate, and hemoglobin saturation
are routinely monitored for all critical care patients [12].
Although IAP measurement is not a novel idea, its importance
and therapeutic implications in the ICU have just recently
become increasingly apparent, however, measurements of IAP
have rarely been employed as a standard monitoring element,
instead, IAP is often measured only when a specific risk factor
or the existence of IAH has been discovered [12]. Intermittent
IAP measurements through the bladder in symptomatic
patients or those with a strong clinical suspicion of developing
IAH every 4 hours-6 hours are universally acknowledged as
standard treatment [12].
Critically Ill Patients rely heavily on critical care nurses to
monitor Intra-abdominal pressure [13]. Although critical care
nurses are responsible for measuring and reporting IAP, there
is limited information on their awareness of IAH and ACS [14].
Despite best practice guidelines, recommendations are often
not implemented [14]. Advanced nursing practice empowers
nurses to manage Intra-abdominal hypertension with greater
clinical discretion, responsibility, and autonomy [15].
Critical care nurses may experience difficulties in adopting
IAP monitoring due to a lack of resources, such as equipment
and qualified personnel, which may impede their capacity to
monitor it efficiently [13]. Additionally, cultural differences may
influence how patients and families react to IAP monitoring and
care, despite these limitations, critical care nurses can assist
minimize negative outcomes associated with IAH and ACS by
recognizing early signs of IAH, delivering interventions, and
educating patients and families on the need of IAP monitoring
[13]. All hospitals recognize the importance of nurses’ roles
as members of the health-care team. Continuous in-service
education is essential for improving nursing care in the ICU,
nurse education must align with their knowledge and skills
[16]. Research indicates a lack of awareness among nurses on
recognizing high-risk patients and clinical indicators of IAH/ACS
[12].
The purpose of this scoping review is to provide an overview
of current Intra-abdominal pressure in nursing management
among critically ill adult patients and the role of critical care
nurses in measuring Intra-abdominal pressure in critical
care settings. The review will consider current methods for
measuring Intra-abdominal pressure. The results of this
analysis will provide a comprehensive overview of the current
state of Intra-abdominal pressure monitoring and serve as a
guideline for critical care nurses.
Rationale of the Review
The role of critical care nurses in Intra-abdominal pressure
monitoring among critically ill patients is vital to patient
care, as critically ill adult patients are at high risk for serious
health complications that can lead to mortality [1]. Despite
the importance of Intra-abdominal Pressure (IAP) monitoring,
critical care nurses have little understanding and practice
with Intra-abdominal Hypertension (IAH) and Abdominal
Compartment Syndrome (ACS) [7,17]. The use of a urinary
catheter or nasogastric tube to measure IAP is not universally
used, and cultural variations may impact patient and family
responses to monitoring and care [7].
The goal of this scoping study is to assess critical care nurses’
existing knowledge and practices regarding IAH and ACS, as well
as the problems they face when implementing IAP monitoring
among critically ill adult patients. This review will look at
the current methods for measuring IAP, critical care nurses’ understanding of IAH and ACS, and cultural and resourcerelated
challenges to IAP monitoring implementation [9].
According to IAH and ACS can result in considerable morbidity
and mortality, emphasizing the significance of appropriate
IAP monitoring [2]. Furthermore, critical care nurses may
have difficulty implementing IAP monitoring due to a lack of
resources, such as equipment and qualified personnel [13]. This
scoping research is important due to the dearth of information
on the knowledge and practices of critical care nurses about
IAP, despite the need of IAP monitoring in critically ill adult
patients.
Literature Review
Definition of Intra-abdominal Pressure
The pressure in the abdominal cavity is referred to as Intraabdominal Pressure (IAP) [18]. Intra-abdominal Pressure (IAP) refers to the constant pressure in the abdominal cavity created by the interaction of the abdominal wall and internal organs [12].
In critically ill adults, the Intra-abdominal Pressure (IAP) is typically 5 mmHg-7 mmHg [19]. In critically ill patients in the Intensive Care Unit (ICU), a persistent increase in IAP caused by acute respiratory failure, gastrointestinal dysfunction, abdominal and pelvic hemorrhage, effusion, intensive fluid resuscitation, and/or septic shock can lead to (IAH) or (ACS) [19].
Diseases Related to Measure IAP
Intra-abdominal Hypertension (IAH) is defined as an elevated IAP exceeding 12 mmHg [7]. This syndrome can be a lifethreatening consequence in a variety of therapeutic situations, including critically sick patients, trauma victims, and those undergoing abdominal surgery. IAH can cause organ dysfunction, hypo perfusion, and even organ failure if not managed [7]. IAP measurement is important for diagnosing and managing IAH. There are several methods for measuring IAP, including both invasive and non-invasive procedures [20]. The measurement device used is determined by the clinical context and patient condition [21]. According to Crumley (2020), the study concluded that, Intra-abdominal hypertension is common in critically ill patients of all ages and is associated with negative outcomes such as abdominal compartment syndrome [20]. Because there are no obvious clinical symptoms, the illness is frequently overlooked, highlighting the need for instruments that can reliably test IAP. Commercially accessible devices assess IAP indirectly, usually through the bladder or stomach. More study is needed to demonstrate the benefits of routine screening, define risk factors for IAH/ACS development, and assess the impact of IAP reducing interventions in order to improve patient outcomes.
The development of accurate and reliable IAP measurement instruments is critical for IAH diagnosis and management. Recent work has focused on validating and improving these devices [22]. A comprehensive evaluation of diagnostic sensors for IAP monitoring found numerous devices with promising findings, but additional study is needed to determine their accuracy and reliability [22]. Recent studies have investigated the importance of static and dynamic Intra-abdominal pressure monitoring in the diagnosis and therapy of acute pancreatitis [23].
IAH has been linked to a diverse array of conditions, such as renal kidney disease. The renal resistive index, which quantifies blood flow in the kidneys, is positively correlated with Intraabdominal pressure [24]. This demonstrates that IAH may be a contributing factor to renal dysfunction and failure. Intraabdominal pressure may also increase during pregnancy, particularly when the abdomen is acute. According to Augustin (2023) is a common pregnancy issue that can result in major maternal and fetal consequences if not managed. Monitoring IAP is critical in these cases to avoid complications and guarantee the best possible outcomes [25].
IAP is an important characteristic in critically ill adult patients because it can result in life-threatening consequences including Abdominal Compartment Syndrome (ACS) and Intra-abdominal Hypertension (IAH) [26]. IAP measures in neuro critical patients have been found to be critical for monitoring illness development and predicting prognosis [18]. For example, Xu et al. (2021) discovered that greater IAP was associated with a higher risk of ACS and mortality in neuro critical patients [18].
The intestinal fatty acid binding protein has been found as a possible predictor of IAP-related problems in ICU patients [27]. Furthermore, a study discovered that IAP was a strong predictor of outcome in patients with acute pancreatitis, and its measurement might be utilized as a prognostic marker [28]. Thus, monitoring IAP in critically ill adult patients is vital for preventing and managing these life-threatening consequences [28].
Zou et al. (2021) examined IAP readings in critically ill patients with intra vesical normal saline at 15°C, 25°C, and 35°C temperatures [19]. The study discovered that utilizing normal saline at 35°C resulted in considerably greater IAP values compared to 15°C and 25°C. This suggests that the temperature of normal saline may alter IAP measurements, which is an important factor to consider when monitoring IAP in critically ill patients. This study emphasizes the need of standardizing the temperature of normal saline used for IAP measurements in order to obtain accurate and reliable results. More study is needed to determine the best temperature for IAP measurements and develop a standardized technique for their usage in clinical practice.
Causes and Risk Factors of Intra-abdominal Pressure (IAP) Measurement in Critical Adult Patients
The assessment of Intra-abdominal Pressure (IAP) is an important metric in critically ill adult patients, particularly those with Intra-abdominal Hypertension (IAH) and Abdominal Compartment Syndrome (ACS) [26].
Sepsis, for example, can cause increased capillary permeability, edema, and high IAP, Similarly, trauma can cause bleeding and edema, which increases IAP, burns, pregnancy, obesity, chronic kidney disease, and prolonged mechanical ventilation [18,26,27,28].
Risk factors for IAH and ACS are also present. Older age increases the risk of IAH and ACS due to decreasing lung compliance and cardiac performance [28]. Males are also more susceptible due to differences in abdominal anatomy and physiology [28]. Patients who have had abdominal surgery before are more likely to develop adhesions and scar tissue [26].
The classification of IAP-related disorders is critical for successful management. Intra-abdominal hypertension is divided into 3 categories based on IAP level: Grade I (IAP 12 mmHg-15 mmHg), Grade II (IAP 16 mmHg–20 mmHg), and Grade III (IAP at admission, first and second IAP measurements after admission were ≥ 12 mmHg ), Grade IV (IAP>25 mmHg (Grade IV (IAP>25 mmHg ), Abdominal compartment syndrome is divided into 2 stages: Stage I (mild ACS, defined by raised IAP and decreased urine output) and Stage II (severe ACS, defined by elevated IAP, decreased urine output, and organ failure (Table 1) [26].
Table 1: Summary for risk factors for IAP in adults
| Risk factors
|
| Distended abdomen |
| Peritoneal dialysis |
| Laparoscopy with excessive insufflation pressures |
| Diagnosis of the following |
| Acute pancreatitis |
| Hemoperitoneum/pneumoperitoneum or intraperitoneal fluid collections |
| Intra-abdominal infection/abscess |
| Intra-abdominal or retroperitoneal tumors |
| Liver dysfunction/cirrhosis with ascites |
Sign and Symptoms of IAP
IAP can cause a range of signs and symptoms, which can be subtle and may not always, be immediately apparent [27]. One of the initial indications of IAP is abdominal distension, which can show as a palpable abdominal mass or swelling [8]. This can be accompanied by nausea, vomiting, and stomach pain [29]. As IAP increases, patients may have respiratory compromise, including decreased lung volumes and increasing peak airway pressures. Cardiovascular instability, such as reduced blood pressure and tachycardia, may also develop as the body responds to the increased Intra-abdominal pressure [18].
Other indications of IAP include decreased urine production and oliguria, which can be symptomatic of impaired renal perfusion due to increased Intra-abdominal pressure [27]. Additionally, individuals with IAP may display changes in mental status, such as disorientation, agitation, and altered consciousness, which can be linked to reduced cerebral perfusion [8]. In severe cases of IAP, patients may develop abdominal compartment syndrome, characterized by significant organ dysfunction and failure. Early identification and therapy of IAP are critical to prevent complications and enhance patient outcomes, monitoring methods for IAP measurement have been developed to aid in early detection and management of IAP [29].
Pathophysiology of IAP in Critical Adult Patients
According to De Laet et al. (2020), IAP is a complex pathophysiological process involving the interaction of several variables, including increased fluid and gas accumulation within the abdominal cavity, altered abdominal wall compliance, and impaired respiratory and cardiovascular performance. One of the most common causes of IAP is increased fluid collection in the abdominal cavity, which can be caused by a variety of events such as hemorrhage, ascites, or edema [8,30].
This extra fluid might compress the abdominal organs, reducing blood flow and oxygenation. In addition, trauma, surgery, or inflammation can cause the abdominal wall to become less compliant, contributing to the development of IAP [19]. Increased IAP can have a major impact on respiratory function, such as lower lung volumes, higher peak airway pressures, and poorer gas exchange [30]. This can cause respiratory failure and an increased risk of death. Cardiovascular dysfunction is also common in IAP patients, as evidenced by reduced cardiac output, hypotension, and tachycardia [31]. This can worsen respiratory impairment and raise the likelihood of organ malfunction. IAPrelated pathophysiological alterations can have an impact on different organ systems. For example, elevated IAP can impair renal function, reduce urine production, and raise the risk of acute kidney damage [30]. IAP can also cause gastrointestinal dysfunction, such as delayed gastric emptying and reduced gut motility [8].
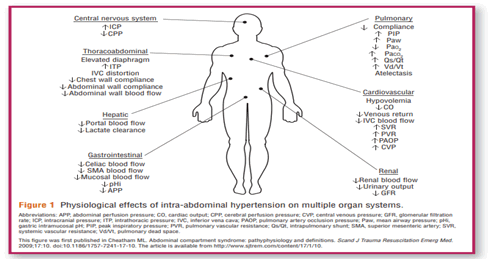
Complications of (IAP) in Critical Adult Patients
According to Strang et al. (2021, IAP related problems can result in considerable morbidity and mortality in critically sick patients [27]. Respiratory compromise is a complication of IAP that can emerge as decreased lung volumes, increased peak airway pressures, and impaired gas exchange [30]. In addition, IAP can produce cardiovascular instability, which includes reduced cardiac output, hypotension, and tachycardia [30]. Another IAP consequence is abdominal compartment syndrome, which occurs when Intra-abdominal pressure exceeds 20 mmHg [30]. This syndrome can cause serious organ malfunction and failure, including respiratory, cardiovascular, and renal impairment. Abdominal compartment syndrome is a life-threatening illness that requires rapid treatment. In addition, IAP can produce gastrointestinal issues such as delayed gastric emptying and reduced gut motility [32]. This might cause nausea, vomiting, and abdominal pain, which can worsen the patient’s condition. Furthermore, IAP can have a major impact on the neurological system, causing mental status changes such as disorientation, agitation, and altered consciousness [33]. Physiological effects of IAP on Multiple Organ Systems are discussed in Figure 1 [34].
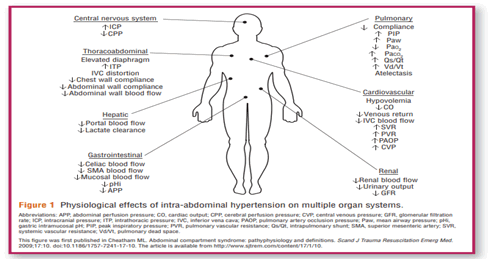
Figure 1: Physiological effects of IAP on multiple organ systems
Contraindication of (IAP) in Critical Adult Patients
Abdominal Compartment Syndrome (ACS) is a substantial contraindication to IAP measurement [35]. ACS can occur when abdomen pressure rises to a level that impairs organ function, and measuring IAP may be inappropriate if the patient’s condition puts them at risk for hemodynamic instability [35]. Furthermore, certain patient populations, such as those with severe respiratory compromise or gastrointestinal disorders (e.g. bowel obstruction), may have contraindications that hinder IAP monitoring. The procedure for measuring IAP needs careful consideration of the patient’s position, as badly positioned individuals can result in false readings [33].
Furthermore, critically ill patients who have recently had abdominal surgery may be at risk for elevated IAP. After surgeries such as laparotomy or other procedures in which the abdomen is manipulated, the possibility of measuring IAP must be balanced against the danger of future complications [12].
The Important of (IAP) in Critical Adult Patients
IAP is an important factor of Intra-abdominal organ perfusion, and it can lead to serious consequences including Abdominal Compartment Syndrome (ACS). Elevated IAP impairs blood flow to abdominal organs, potentially causing ischemia and organ failure [30]. IAP has been demonstrated in studies to be an accurate predictor of numerous problems in critically ill patients. Strang et al. (2021) found that Intestinal-Fatty Acid-Binding Protein (I-FABP) levels could predict problems associated with IAP elevation in ICU patients [27]. This emphasizes the importance of precise IAP measures as part of the overall clinical assessment. Elevated IAP may suggest the need for immediate action, such as decompressive surgery or fluid management modifications, to avoid further worsening.
IAP is also linked to nutritional status and care of critically ill individuals. Monitoring IAP, as indicated in Guan et al. (2024) guidelines, can inform nutritional therapies, especially when patients exhibit indications of intestinal edema or reduced gastrointestinal function [36]. Elevated IAP may present issues for sufficient nutritional supply, underlining the significance of tailored treatment plans that incorporate IAP data to improve patient recovery.
The relevance of IAP is especially clear in the postoperative situation. Dugar et al. (2024) discovered that IAP measures could predict wound problems in individuals undergoing an emergency laparotomy [37]. Monitoring IAP in these circumstances can help guide clinical decisions by identifying at-risk patients and implementing preventive measures to improve surgical outcomes.
Prevalence and Incidence of (IAP) in Critical Adult Patients in the World
The incidence of IAP in critical adult patients has been investigated in a variety of situations and demographics. According to one study, 9,345 patients were screened, and 95 were evaluated, yielding a mean age of 56.7 years and 79% male. Alcohol was the leading cause of liver cirrhosis (45.3%), followed by alcohol combined with hepatitis C (9.5%). Infection and haemorrhage were both precipitating causes (26% and 21%, respectively). The prevalence of Intra-abdominal Hypertension (IAH) was 82.1%, with Abdominal Compartment Syndrome (ACS) at 23.2% and a mean maximal Intra-abdominal pressure of 16.0 mmHg. Independent risk variables for IAH included alcoholic cirrhosis, the West-Haven score, and the PaO2/FiO2 ratio, while infection was associated with ACS. The 28-day death rate was 52.6%, which was strongly related with greater IAP and ACS. The study emphasizes the need of early detection and management of IAH/ACS in critically ill cirrhotic individuals [38]. Another cohort study published in 2020 discovered that the prevalence of IAP was 34.6% among patients admitted to ICUs in a low-income country.
In terms of incidence, the same cohort study in 2020 found a 21.1% daily incidence of IAP among patients admitted to ICUs in a low-income country [39]. These data indicate that IAP is a rather prevalent illness in critically ill patients, particularly those with liver cirrhosis.
Patients with IAP have much higher mortality rates. A cohort research in 2020 discovered that patients with IAP had a higher mortality rate of 54.5% compared to 24.4% among those without IAP [39]. Furthermore, mortality rates rose with increasing IAP severity, reaching 73.7% among patients with severe IAP [39]. These findings emphasize the need of early detection and treatment of IAP in critically sick patients to avoid complications and enhance outcomes.
Prevalence and incidence of (IAP) in Critical Adult Patients at Saudi Arabia
The prevalence and incidence of Intra-abdominal Pressure (IAP) in critically ill adults in Saudi Arabia are poorly reported. However, Qutob et al. (2022) conducted an online crosssectional survey to investigate clinicians’ understanding of abdominal compartment syndrome and IAP in Saudi Arabia [40]. According to the survey, a considerable majority (70.3%) was familiar with Intra-abdominal Hypertension (IAH) and its effects on organ function, with an even greater number (73.7%) understanding the notion of Abdominal Compartment Syndrome (ACS). Despite this understanding, over 43.0% of participants expressed uncertainty about measuring Intraabdominal Pressure (IAP). The use of inotropes or vasopressors was the most often cited intervention for IAH and ACS, accounting for 13.5% of all interventions discussed.
Management and Nursing Care for Increased and Decreased IAP
Management and nursing care for increased and decreased Intra-abdominal Pressure (IAP) is an essential part of patient care, especially in critical care units [8,34]. Intra-abdominal pressure is the pressure within the abdominal cavity, which typically fluctuates between 0 mmHg and 5 mmHg. Pressures more than 12 mmHg are defined as Intra-abdominal Hypertension (IAH), which can result in consequences such Abdominal Compartment Syndrome (ACS). Effective nursing care requires close monitoring and early interventions to address both raised and lowered IAP, since changes can have a major impact on organ function and overall patient stability [8,34].
Continuous monitoring of IAP is required for both increasing and decreasing pressures. Nursing staff must look for symptoms of IAH, such as abdominal distention, decreased urine output, or changes in ventilatory parameters. Implementing defined protocols and using monitoring devices are critical for early detection of IAP changes [20].
When dealing with increasing IAP, nursing interventions are largely concerned with relieving the pressure and resolving any underlying issues. Optimizing patient placement is a simple yet beneficial step, as elevating the head of the bed can encourage diaphragmatic excursion and lung expansion [8]. Furthermore, careful fluid management is required, including monitoring and possible modifications to fluid intake and output. Diuretics may be administered in cases of fluid overload, depending on the physician’s instructions. If there are indicators of oncoming ACS, nurses must be prepared to assist with abdominal decompression operations while also emphasizing the significance of early enteral feeding [29,34].
When IAP is reduced, nursing care focuses on identifying potential problems associated with the condition. Patients may develop visceral organ dysfunction or insufficient perfusion, which can cause hypotension or altered mental status. Close monitoring is therefore required to detect these indications early [8]. To avoid respiratory difficulties caused by low IAP levels in mechanically ventilated patients, ventilatory settings may need to be altered. In cases of hypovolemia, cautious fluid resuscitation can assist restore hemodynamic stability, nevertheless, it must be controlled to avoid excessive Intraabdominal fluid accumulation. Furthermore, good coordination with the healthcare team is critical for addressing underlying difficulties and providing comprehensive patient management [8].
Critical Care Nursing Role and Document in IAP
Critical care nursing is essential in monitoring and regulating Intra-abdominal Pressure (IAP) in critically ill patients. The measurement of IAP is critical because it has a major impact on hemodynamic stability and organ function. Nursing responsibilities include monitoring IAP levels, identifying symptoms of Intra-abdominal Hypertension (IAH), and providing early interventions. The literature emphasizes the importance of defined methods for measuring and documenting IAP in the critical care environment to enable consistent monitoring and timely decision-making [5,8].
Accurate documentation of IAP is critical for assessing trends over time and implementing effective interventions. Nurses are in charge of documenting baseline readings, reassessing IAP after interventions, and recording any related clinical findings. By collecting these data, the nursing team may better communicate the patient’s state to the healthcare team, allowing for collaborative discussions on management plans [8,40,41]. Furthermore, the use of modern measurement techniques has been stressed, and nurses should be conversant with these procedures as they grow [5,12].
IAP treatment also takes into account a variety of factors that can influence abdominal pressure, such as patient posture, sedation, and ventilator assistance. Non-invasive ventilation has been proven in studies to have effects on IAP, which nursing personnel must recognize and document [42]. Similarly, sedation levels can affect IAP measures, needing close monitoring [31].
Critically ill individuals are especially sensitive to IAH complications, such as Abdominal Compartment Syndrome (ACS), which can result in severe morbidity or fatality [41,43]. Nurses, as frontline caregivers, are responsible for identifying symptoms of IAH and ACS early on, such as abdominal distension and decreased urine output. Prompt detection can result in early treatment actions, such as fluid management or surgical consultation, ultimately enhancing patient outcomes [8].
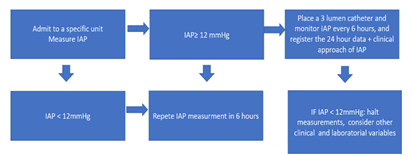
Measuring Intra-abdominal Pressure
Various approaches have been devised to accurately assess IAP. The most commonly used procedures include direct intermittent measures (dialysis or laparoscopy), indirect (catheters implanted through the bladder, stomach, uterine, or rectum), and continuous measurements (catheters positioned in the bladder, stomach, or peritoneal). Flowchart for monitoring Intra-abdominal hypertension is discussed in Figure 2 [44].
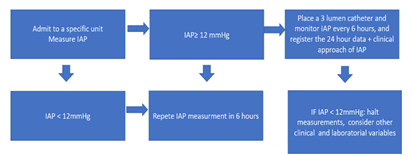
Figure 2: Flowchart for monitoring intra-abdominal hypertension
Methods to measure (IAP)
Intra-abdominal Pressure (IAP) measurement is vital in the management of critically ill patients in the intensive care unit. Several approaches for accurately assessing IAP have been developed, each with unique applications and benefits. This overview focuses on 3 main methods: Manometry, transducers, and the Compass Connection methodology.
Manometer: Manometry is one of the traditional ways for measuring IAP. Typically, a pressure transducer is attached to a catheter inserted into the urine bladder or gastrointestinal system. The instrument monitors the pressure within these hollow organs, which reflects the pressure inside the abdominal cavity. To maintain consistency, the measurement is done in a standardized position, typically supine [8]. Manometry is regarded as a valid way of assessing IAP, nevertheless, accurate readings require proper training and procedure adherence. This approach has been validated in multiple clinical contexts and is still commonly used in intensive care units (Table 2) [18].
Table 2: Straightforward approach to measuring Intra-abdominal pressure using a manometer for adult patients in an ICU
| Step |
Action |
| Patient preparation |
Confirm patient identity and review relevant medical history |
| Position the patient supine |
| Explain the procedure to the patient (if alert) to reduce anxiety |
| Catheter insertion |
Use a sterile Foley catheter (12-16 Fr is common) |
| Insert the catheter into the bladder using sterile technique |
| Secure the catheter to prevent accidental dislodgment |
| Setting up the manometer |
Connect the Foley catheter to the manometer using sterile, appropriately sized tubing |
| Fill the tubing and manometer with sterile saline to eliminate air bubbles |
| Position the manometer at the level of the iliac crest (mid-axillary line) for accuracy |
| Measuring IAP |
Close the drain from the Foley catheter to prevent urine from flowing out during measurement |
| Allow the pressure to stabilize for a few seconds |
| Once stabilized, record the IAP from the manometer in mmHg. Normal IAP is usually between 5 mmHg-12 mmHg |
| Continuous monitoring (if needed) |
If necessary, allow continuous monitoring by leaving the system closed while regularly checking the manometer |
| Document IAP readings in the patient’s medical records |
| Follow-up actions |
If IAP is elevated (>12 mmHg), consult the healthcare team for appropriate management |
| Monitor the patient’s overall clinical condition, adjusting care as needed based on IAP |
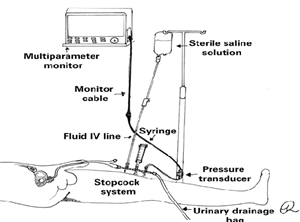
Transducer: The use of pressure transducers is a more advanced method for measuring IAP. A pressure transducer is frequently coupled to a catheter implanted in the bladder or abdomen to provide continuous IAP monitoring capabilities. This technology is highly accurate and can continually send pressures to the monitoring system, enabling for real-time tracking of IAP changes [5]. Transducers are especially useful in critical care situations, when patients’ status might change fast. The continuous aspect of this monitoring system gives vital information that can aid in the timely management of increased IAP (Figure 3) (Table 3) [18,45].
Table 3: Straightforward approach to measuring Intra-abdominal pressure using a transducer for adult patients in an ICU setting
| Step |
Action |
Notes |
| Patient preparation |
Confirm patient identity and history |
Supine position ensures an accurate reference point |
| Position the patient in supine position |
Helps to reduce anxiety |
| Explain the procedure to the patient (if alert) |
-
|
| Catheter placement |
Use sterile technique for catheter insertion into the bladder |
Prevents infection |
| Secure the catheter after insertion |
Minimizes movement |
| Setting up the transducer |
Connect the sterile tubing from the urinary catheter to the pressure transducer |
Ensure a leak-free connection |
| Fill the transducer and tubing with sterile saline to eliminate air |
Important for accurate pressure measurement |
| Position the transducer at the mid-axillary line at the level of the iliac crest |
Provides an accurate reference point |
| Zero the transducer at the correct level (bladder level) |
Necessary for accurate readings |
| Measuring IAP |
Close the drainage system temporarily to prevent pressure escape |
Ensure accurate pressure measurement |
| Allow pressure to stabilize for a few seconds before reading |
Ensure reading reflects true pressure |
| Record the IAP displayed on the monitor (normal range: 5 mmHg-12 mmHg) |
Readings >12 mmHg may indicate complications |
| Continuous monitoring |
Set the monitor for ongoing pressure measurement if needed |
Allows for real-time tracking of IAP |
| Document IAP readings at regular intervals |
Required for clinical assessment and management |
| Follow-up actions |
If elevated pressures are noted, collaborate with the healthcare team for assessment |
Consider fluid management or surgical |
| Continue to monitor and adjust care based on the IAP readings and patient condition |
Integrated into the overall treatment plan |
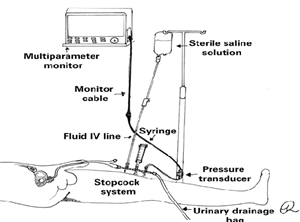
Figure 3: Intra-abdominal pressure measurement using the pressure transducer technique and a three-way stopcock system
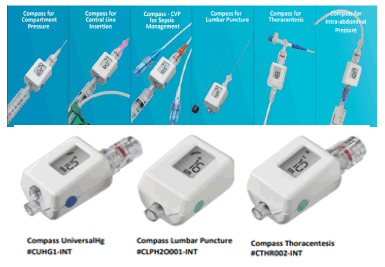
Compass Intra-abdominal Pressure monitoring (IAP): Diagnosing and treating life-threatening conditions relies on time-sensitive, dependable data. The popular methods currently being used to get information are cumbersome, time consuming, or inaccurate. Such methods can take control away from the clinician [46] (Figure 4).
• Compass disposable pressure transducers provide digital
• Pressure measurements in an instant to help clinicians with
• Quantitative direction for proper treatment courses
• Compass eliminates the set up complexities and inaccuracies of other traditional pressure transduction systems. The easy-touse, single-use, sterile compass is versatile to a wide range of clinical applications requiring pressure monitoring
• Measures in either mmhg or cm H2O
• Available in luer lock or luer slip connections
• Available with and without a guidewire port
• Single, sterile, disposable packaging, 5 per box
• Precise to American National Standards Institute standards-accurate measurements
• Compact, sterile, disposable
• Not made with natural rubber latex
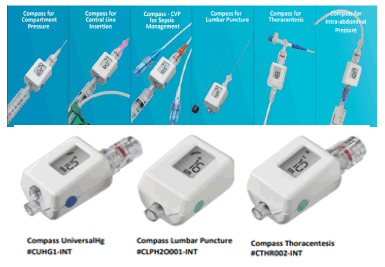
Figure 4: Compass digital pressure monitors compact physiological pressure transducer
IAP CUHG1-INT
The Compass Intra-abdominal Pressure monitoring (IAP) is as shown in Table 4.
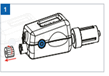
Table 4: Compass Intra-abdominal Pressure monitoring (IAP)
| Compass Intra-abdominal Pressure monitoring (IAP)
|
- Activate and calibrate Compass Universal Hg by depressing the blue power
- button for approximately one second until the display reads ‘00 mm’. Remove the proximal luer cap Removing this cap prior to calibration does not affect the reading
|
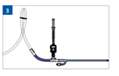
|
- Prime Compass and accessories prior to attaching it to the sampling port of the Foley catheter
|

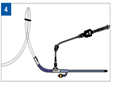
|
- Connect Compass directly to the female luer lock sampling port of the Foley catheter
|
|
- Note: A short (~25cm–51 cm) extension tube can be connected to the sampling port and the male luer lock connection of Compass Universal Hg to facilitate the positioning of the Compass device at the mid-axillary line (level of urinary bladder)
|
|
| Pressure Measurement
|
- Confirm Compass Universal Hg is positioned at the mid-axillary line (level of the urinary bladder). For patients in an inclined position, place Compass at the iliac crest at the mid-axillary line
- Clamp the tubing that leads to the collection device with a slide clamp, rubber band or haemostat
- Infuse ~20 cc saline for adults or quantity per hospital protocol within 10 seconds. Infusion can be directly into Compass Universal Hg or through a needleless valve positioned at the female luer lock port of Compass Universal Hg
- Allow system to equilibrate (a few seconds) prior to reading the pressure
- Verify Intra-abdominal pressure from the pressure data displayed on Compass Universal Hg Liquid Crystal Display
- Record any infused saline in the patient chart to adjust urine output. When measurement is completed, unclamp the drainage tube
- Disconnect the syringe and cap Compass Universal Hg with a sterile dead-end cap or needleless valve if the needleless valve isn’t already present. Repeat process for subsequent measurements
|
|
| Device Power Off and Recalibration
|
| Press the button three times in a ‘PUSH-PUSH-HOLD’ sequence (i.e. quickly push the button twice and then hold the third button-push until the device turns off). To recalibrate and zero the device, open the device to atmosphere and depress the power button until the display reads ‘00 mm’. For complete instructions and warnings, consult the Instructions for use supplied with the device
|
Conditions for a Reproducible IAP Measurement
The Conditions for a Reproducible IAP Measurement is as shown in Table 5 [10].
Table 5: Conditions for a Reproducible IAP Measurement
| Expressed in mm Hg (1 mm Hg=1.36 cm H2O) |
| Measured at end-expiration |
| Performed in the supine position |
| Zeroed at the iliac crest in the mid-axillary line |
| Priming volume <25 mL of saline (1 mL kg-1 for children up to 20 kg) |
| Measured 30 sec-60 sec after instillation to allow for bladder |
Methods
A thorough scoping analysis was carried out to look into the current evidence on the function of critical care nurses in Intra-abdominal pressure monitoring among critically ill adult patients. The assessment followed a rigorous methodology, including the PRISMA flow chart, to guarantee transparency and adherence to best evidence-based practices.
The review methodology rigorously followed the suggestions made by Arksey et al. (2005) for defining the scope of review methodology, emphasizing the importance of a systematic and complete approach to data gathering and analysis [47]. This scoping review offers significant insights and evidence-based suggestions for healthcare professionals and policymakers on the most successful tactics for critical care nurses to use in Intra-abdominal pressure monitoring, as well as areas for future research.
Search Strategy
In 2024, a systematic search was carried out using online resources such as PubMed, Google Scholar, and the Cochrane Library to uncover research on critical care nurses’ roles in Intra-abdominal pressure monitoring among critically ill adult patients. The search keywords were linked using Boolean operators (AND, OR) to optimize search results and assure topic relevancy. A combination of keywords and phrases was used to locate relevant documents. The search terms included “critical care nurses” or “nurses” or “intensive care nurses” or “ICU nurses,” “Intra-abdominal pressure monitoring” or “IAP monitoring or ACS OR IAH”.
The search criteria were intended to include studies that looked into critical care nurses’ knowledge, practices, and issues with Intra-abdominal pressure monitoring. The terms included “critical care nurses” and “Intra-abdominal pressure monitoring”, as well as “critically ill adult patients”. Additional criteria were utilized to filter the search results, such as English language limits, study design constraints (quantitative and qualitative studies), and publication date restrictions (2020- 2024). The study only included critical care nurses who worked in intensive care units.
Inclusion Criteria
The current scoping review examined papers on the function of critical care nurses in Intra-abdominal pressure monitoring among critically Ill adult patients. Studies that investigated critical care nurses’ knowledge, practices, and issues with Intraabdominal pressure monitoring were considered. In addition, papers on critical care nurses working in Intensive Care Units (ICUs) were included. The evaluation included both quantitative and qualitative studies published in English between 2020 and 2024.
Exclusion Criteria
On the other hand, the current scoping review omitted studies that did not match specific criteria. Studies that did not specifically address critical care nurses or their role in Intraabdominal pressure monitoring were eliminated. Furthermore, research published before 2020 or after 2024, or those not published in English, were excluded.
Selection Process
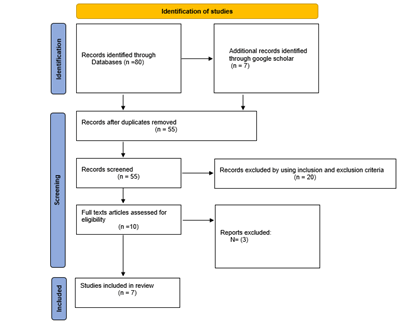
In 2024, the review search returned 80 results. After deleting duplicates, 55 studies remained. After examining the titles and abstracts, 20 studies were removed because they did not meet the inclusion criteria. Thus, 10 studies were thoroughly examined to assess eligibility, three studies were excluded since they did not describe the original investigations. As a result, this scoping review includes 7 studies (Figure 5) (Table 6).
Table 6: Summary of selected studies
| Author
|
IAP Measuring Methods
|
Results
|
| Xu et al.
|
- IAP has historically been measured using a variety of ways, with Intra-Bladder Pressure (IBP) being a generally acknowledged indirect measurement approach.
- Recent improvements include the introduction of continuous IAP monitoring devices, which improve convenience by providing digital display, long-term data storage, and real-time clinical analysis.
|
- The typical IAP is usually equal to or less than 12 mm Hg.
- IAH is characterized as two consecutive IAP values of more than 12 mmHg within 4 hours-6 hours.
- ACS is defined by an IAP greater than 20 mmHg and organ dysfunction/failure, which can result in significant consequences such as gastrointestinal ischemia, acute renal failure, and lung injury, all of which contribute to increased morbidity and death.
- The novel IAP monitoring system can identify IAH and analyze clinical status in real time, allowing for better correlation analysis with other physiological indicators such as intracranial pressure to guide treatment and predict prognosis.
|
| Li et al.
|
- The review states that, while many IAP assessment techniques exist, direct measurement is not suggested as a standard practice due to its high cost and invasiveness. This procedure should only be used in critically ill individuals where normal methods are contraindicated or potentially erroneous. Transvesical measurement is the most extensively used approach, providing a viable choice for both continuous and intermittent IAP assessment.
|
- The scoping review found 42 of the 9,954 screened papers that matched the inclusion criteria. The research looked at several Intra-abdominal Pressure (IAP) measurement techniques and classified them into three types: Direct measurement, indirect measurement, and less invasive measurement approaches. The majority of research performed agreement evaluations, while some investigated crucial criteria such as the safety, time expenditure, and repeatability of various IAP measuring methodologies.
|
| Zou et al.
|
- The researchers discovered a significant difference in Intra-abdominal Pressure (IAP) readings between the 15°C and 35°C saline groups (t=-2.55, P=0.027). In contrast, IAP measurements showed no statistically significant difference between the 25°C and 35°C groups (t=0.73, P=0.48). A Bland-Altman analysis revealed consistency in IAP readings between the 25°C and 35°C saline groups, supporting data dependability at these temperatures.
|
- In this study, IAP was determined by injecting 25 mL of sterile saline into the bladder, as per the World Society of Abdominal Compartment Syndrome standards. The main feature of this method is that the saline does not have to be at a certain temperature; nonetheless, the study looked into the effect of several saline temperatures (35°C, 25°C, and 15°C) on measurement accuracy. The data imply that, while it is preferable to use saline at body temperature (35°C) for IAP measurements, saline temperatures over 25°C produce reliable results. In contrast, the study suggests that saline should not be used at temperatures below 15°C since it may cause measurement mistakes.
|
| Pereira et al.
|
- The study emphasizes the vital importance of monitoring Intra-abdominal Pressure (IAP) in critically ill cirrhotic patients, particularly those at risk of IAH and ACS. Although the specific IAP measurement methods used in this study are not described in the results, the context suggests adherence to established techniques for measuring IAP, most likely involving bladder pressure monitoring in accordance with the World Society of Abdominal Compartment Syndrome's standard practices. Proper IAP assessment is critical for the early detection, prevention, and treatment of IAH and ACS, which may eventually improve outcomes in this high-risk patient population.
|
- In multi centric retrospective cohort study, a total of 9,345 individuals were screened, with 95 critically sick cirrhotic patients considered. The average age of the participants was 56.7 years, with 79% being male. The cause of liver cirrhosis was primarily alcoholic (45.3%), with some individuals having both alcohol-related disorders and hepatitis C virus (9.5%). Infections (26%) and bleeding (21%) were the triggering events for these patients. At ICU admission, the mean severity scores were MELD 26.2 and SAPS II 48.5. The study found a significant prevalence of Intra-abdominal Hypertension (IAH) and abdominal compartment syndrome (ACS), with 82.1% and 23.2%, respectively. The mean maximum Intra-abdominal Pressure (IAP) was 16.0 mmHg. Regarding IAH grading, 17.9% had no IAH, 26.3% were classed I, 33.7% II, 17.9% III, and 4.2% IV. Independent risk variables for IAH included alcoholic cirrhosis, the West-Haven score, and the PaO2/FiO2 ratio, whereas infection was a significant risk factor for ACS. The study also found a troubling 28-day death rate of 52.6%, with higher IAP and ACS indicating worse outcomes. Independent mortality risk factors included the MELD score, white blood cell count, PaO2/FiO2 ratio, and lactate concentration during ICU admission.
|
| Smit et al.
|
- While the specific techniques of measuring Intra-abdominal Pressure (IAP) were not specified in the data, the context implies adherence to accepted protocols for IAP monitoring in critically ill patients. IAP is often measured using bladder pressure or other established techniques that meet the World Society of Abdominal Compartment Syndrome criteria. The outcomes of this study highlight the need of appropriate IAP monitoring in high-risk patient populations, as the high prevalence of IAH and ACS is associated with higher morbidity and mortality. Identifying individuals at high risk, such as those with a BMI>30 kg/m², emergency abdominal surgery, or pancreatitis, is crucial for timely monitoring and interventions.
|
- Between March 2014 and March 2016, a prospective, observational, single-center cohort research included 503 patients, with 307 men (61%), and 196 females (39%). Patients admitted to the intensive care unit were diagnosed with a variety of conditions, including pancreatitis, elective or emergency open abdominal aorta surgery, orthotopic liver transplantation, other major abdominal procedures, and trauma. Of these individuals, 164 (33%) developed Intra-abdominal Hypertension (IAH), while 18 (3.6%) developed Abdominal Compartment Syndrome (ACS). Patients with pancreatitis had the highest rate of ACS (57%), followed by those receiving orthotopic liver transplantation (7%) and abdominal aorta surgery (5%).
|
| Malik et al.
|
- The Intra-abdominal Pressure (IAP) was measured every 8 hours for 72 hours following the patients' admission to the intensive care unit. While the specific procedure for measuring IAP is not specified, it is generally done via bladder pressure monitoring in accordance with recognized recommendations. The study successfully connected the frequency and severity of IAH to patient outcomes by following patients for two weeks after admission to the ICU, underlining the clinical value of routine IAP monitoring in the ICU setting, particularly following laparotomy. The findings indicate that diagnosing and treating abdominal hypertension is vital for efficiently managing patients in the critical care setting.
|
- Between April and September 2021, a comparative cross-sectional study was done at the Combined Military Hospital in Rawalpindi, Pakistan, on 200 patients who underwent laparotomy and were later admitted to the Intensive Care Unit (ICU). Of the patients assessed, 150 (75%) had positive outcomes, while 50 (25%) had negative outcomes. The average age of the patients was 40.63 years, with a standard variation of ±9.448. Notably, 171 (85.5%) of the patients did not have elevated Intra-abdominal Pressure (IAP), but 29 (14.5%) had Intra-abdominal Hypertension (IAH). Statistical analysis found a significant link between high Body Mass Index (BMI) and poor outcomes in patients with IAH, as well as a correlation between the existence and severity of IAH among study participants, both with p-values less than 0.05.
|
|
Gorad, K
|
- IAP was measured using a Foley catheter implanted in the urine bladder and 50 mL of saline for intra-vesical pressure measurement. This technique for measuring IAP is described as straightforward and less intrusive, allowing for precise monitoring of IAP in patients positioned supine. The study sought to offer a valid clinical tool for screening patients at risk of problems associated with elevated abdominal pressure by establishing normal IAP readings in regular patients and determining the threshold for IAH. The researchers noted that adequate IAP measurement and monitoring might act as an important warning sign for clinicians to implement safety measures and prevent the progression to Abdominal Compartment Syndrome (ACS).
|
- A total of 250 hospital-admitted patients were evaluated in prospective trial to measure Intra-abdominal Pressure (IAP) utilizing a new creative technique including a Foley catheter. The group comprised 196 male and 54 female patients. The study discovered that patients who underwent laparoscopic abdominal surgeries (e.g., laparoscopic appendectomy and/or laparoscopic cholecystectomy), as well as those with conditions such as obstructed hernia (enterocele), intestinal obstruction, pancreatic ascites, pneumothorax, alcoholic liver disease with ascites, and chronic obstructive pulmonary disease, had higher IAPs than other patients. The average IAP reported in normal patients ranged from 7cm-9 cm of water, while IAP values greater than 9 cm of water were classed as Intra-abdominal Hypertension (IAH).
|
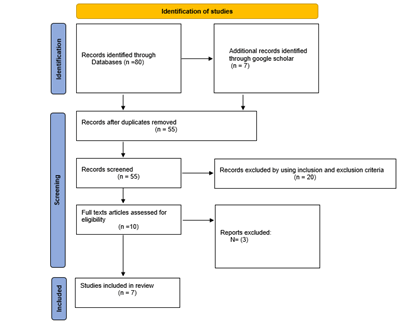
Figure 5: PRISMA 2009 flow diagram
Data Extraction
A review search was carried out, with all titles and abstracts provided, inclusion and exclusion criteria applied, reasons for inclusion and removal explained, and duplicates removed. A PRISMA flowchart was used to depict the four stages of the scoping review approach. Figure 5 depicts the process for a systematic review. Table 6 summarizes the features of the seven included studies. The summarized data was then assessed. The author(s), IAP Measuring Methods used in each study, and findings were all extracted and evaluated.
Results
The results are discussed in Table 6.
Discussion
Critical care nurses have limited knowledge and skills in Intraabdominal
Pressure (IAP) monitoring, which can result in
delays in the detection and management of Intra-abdominal
Hypertension (IAH) and Abdominal Compartment Syndrome
(ACS) [1,17]. This lack of understanding is not restricted to a
single demographic or geographic location, as research in
Pakistan [17].
A review of the literature emphasizes the necessity of educating critical care nurses about IAP monitoring in order to enhance
patient outcomes [32]. Despite the availability of guidelines and
protocols for IAP monitoring, many nurses lack the necessary
knowledge and abilities to properly follow them [2]. This lack of
information can result in ineffective IAP measuring techniques,
which can have catastrophic consequences for critically ill
patients.
Intra-abdominal Pressure (IAP) monitoring has received a lot
of attention in recent years because of the consequences for
critically ill patients. This scoping review indicates a growing
consensus on the relevance of IAP assessment, but it also
highlights differences in techniques, conclusions, and clinical
applications as mentioned in several researches.
Historically, IAP has been measured using a variety of
approaches, with Intra-bladder Pressure (IBP) being a popular
indirect method [18]. The review focuses on improvements in
continuous IAP monitoring devices that improve data collecting
and clinical analysis. The usual IAP is ≤ 12 mmHg, but identifying
Intra-abdominal Hypertension (IAH) as two consecutive IAP
measurements beyond this threshold requires monitoring in
patient management. IAH can cause serious complications,
including Abdominal Compartment Syndrome (ACS), which is
defined by an IAP of more than 20 mmHg as well as organ failure
[18,38]. The association found between higher IAP levels and
greater morbidity and mortality rates across multiple patient
cohorts is especially troubling, emphasizing the importance of
routine IAP monitoring in high-risk patients.
When the findings of several researches are compared,
differences arise in the prevalence of IAH among different
patient categories discovered that medical patients and those
undergoing emergency procedures had IAH rates of around
42.5% and 43.75%, respectively, which were much higher than
the 12.5% frequency found in elective surgery patients. This
finding highlights the importance of focused IAP monitoring
measures in critically sick patients, particularly those with
established risk factors such alcoholic cirrhosis or emergency
abdominal surgery, as noted by [8].
Furthermore, the methods used to measure IAP vary between
research, with transvesical measurement being used in many
situations because to its safety and repeatability. Zou et al. (2021)
studied the impact of saline temperature on measurement
accuracy and concluded that, while body temperature saline is
preferable, satisfactory results can be obtained at temperatures
higher than 25°C [19]. This understanding contributes to the
discussion on enhancing technical aspects of IAP measurement
to ensure accuracy and consistency in clinical practice.
Cohort studies, such as those carried out by support the
significance of routine IAP monitoring following surgical
procedures [47,48]. Malik et al. (2023) found a substantial link
between the severity of IAH and patient outcomes, emphasizing
the importance of detecting and controlling increased IAP as
soon as possible. The findings of Gorad and Prabhu support
the claim that standardized IAP monitoring methodologies
can serve as an important alert system for doctors, giving a
proactive strategy to preventing ACS [49].
Despite advances in IAP monitoring, several studies advise
against direct measurement due to its high cost and invasive
nature [5]. While innovative technologies such as wireless
transvaginal approaches show promise, their clinical accuracy
remains questionable, necessitating more validation before
general usage [5]. This sentiment is shared across the literature,
where the need for less invasive technologies is balanced with a
recognition of existing standards and practices.
The findings of Pereira et al. (2021), Smit et al. (2022) on the high
occurrence of IAH and ACS among cirrhotic patients highlight
the critical need for close surveillance in this high-risk group
[8,38]. With an alarming 28-day death rate and documented
independent mortality risk factors, such as the MELD score,
the research clearly shows that proactive IAP assessment can
help with early management and perhaps improve patient
outcomes.
Finally, this scoping review demonstrates a consensus on the
vital necessity for IAP monitoring in distinct patient categories,
as well as an understanding of discrepancies in measuring
procedures and prevalence rates [50]. While existing procedures
are reliable, future research should focus on improving
these techniques and solving the information gap about less
intrusive options. Comprehensive standards and training for
clinical teams are required to fully realize the potential of IAP
monitoring as a common practice, improving treatment for
critically sick patients.
Conclusion
Intra-abdominal Pressure (IAP) monitoring is vital in the care
of critically ill patients because it can influence hemodynamic
stability and patient outcomes. There is a definite link between
raised IAP levels and consequences including Intra-abdominal
Hypertension (IAH) and Abdominal Compartment Syndrome
(ACS), which can result in increased morbidity and death.
However, the data show that critical care nurses frequently
lack proper training and familiarity with IAP measuring
methodologies, indicating a substantial gap that could
jeopardize patient care.
This scoping research has highlighted the necessity of teaching
critical care nursing personnel about IAP monitoring techniques.
It emphasizes the importance of standardized assessment
methodologies and raising awareness of the therapeutic
significance of IAP alterations. Variability in methodology and
understanding among healthcare workers, combined with a
range of risk factors that predispose patients to increased IAP,
indicates to a pressing need for greater training and standardized
protocols in critical care settings.
Recommendations
• Enhanced training programs: Create and implement tailored instructional programs for critical care nurses that include the principles, methodologies, and practical applications of IAP monitoring. These should include handson training sessions for the various measuring methods, such as manometry and indirect assessments.
• Standardized protocols: Develop uniform procedures and recommendations for measuring and managing IAP across all critical care settings. This should include specific definitions of normal and abnormal IAP levels, monitoring frequency, and management measures.
• Interdisciplinary collaboration: Encourage collaboration among nursing, medical, and allied health workers to ensure a thorough grasp of IAP monitoring across the entire clinical team.
• Investment in technology: Encourage the use of novel technology for IAP monitoring that can offer continuous and accurate measurements with little invasiveness, decreasing the strain on healthcare personnel while enhancing patient safety.
• Regular audits and feedback: Conduct regular audits of IAP management processes to ensure protocol adherence and identify areas for improvement. Nursing personnel should receive feedback to help them maintain best practices.
• Research and validation: Encourage continuous research into the efficacy of various IAP assessment techniques and their impact on patient outcomes, as well as studies examining the long-term implications of IAP management measures.
Acknowledgement
None.
Conflict Of Interest
Authors have no conflict of interest to declare.
References
- Reyad OR, Mahmoud FH, Eldriny SNM (2022) Assessment of nurses' knowledge and practice regarding intra-abdominal pressure measurement and abdominal compartment syndrome Prevention. Egyptian J Hos Med. 89(1):4578-4586.
[Google Scholar]
- Hunt L, Frost SA, Newton PJ, Salamonson Y, Davidson PM (2017) A survey of critical care nurses' knowledge of intra-abdominal hypertension and abdominal compartment syndrome. Aust Crit Care. 30(1):21-27.
[Crossref] [Google Scholar] [PubMed]
- Christensen M, Craft J (2018) The cardio-respiratory effects of intra-abdominal hypertension: Considerations for critical care nursing practice. Int Crit Care Nurs. 44:53-58.
[Crossref] [Google Scholar] [PubMed]
- Gray S, Christensen M, Craft J (2018) The gastro-renal effects of intra-abdominal hypertension: Implications for critical care nurses. Int Crit Care Nurs. 48:69-74.
[Crossref] [Google Scholar] [PubMed]
- Li Z, Wang H, Lu F (2024) Monitoring and management of Intra-abdominal pressure in critically ill children. Crit Care Nurs. 43(3):44-51.
[Crossref] [Google Scholar] [PubMed]
- Al-Abassi AA, Saadi AS Al, Ahmed F (2018) Is intra-bladder pressure measurement a reliable indicator for raised intra-abdominal pressure? A prospective comparative study. BMC Anesthesiol. 18(1):69.
[Crossref] Google Scholar] [PubMed]
- Lagosz P, Sokolski M, Biegus J, Tycinska A, Zymlinski R (2022) Elevated intra-abdominal pressure: A review of current knowledge. World J Clin Cases. 10(10):3005.
[Crossref] [Google Scholar] [PubMed]
- Smit M, Meurs MV, Zijlstra JG (2022) Intra-abdominal hypertension and abdominal compartment syndrome in critically ill patients: A narrative review of past, present, and future steps. Scand J Surg. 111(1):14574969211030128.
[Crossref] [Google Scholar] [PubMed]
- Sugrue M, Waele JD, Keulenaer BD, Roberts D, Malbrain M (2015) A user's guide to intra-abdominal pressure measurement. Anaesthesiol Intensive Ther. 47(3):249-258.
[Crossref] [Google Scholar] [PubMed]
- Margallo FMS, Wise RD, Rodseth RN, Correa-Martin L, Becker P, et al. (2017) Correlation between different methods of intra-abdominal pressure monitoring in varying intra-abdominal hypertension models. Sou Afri J Crit Care. 33(1):15-18.
[Google Scholar]
- Iacubovici L, Karol D, Baar Y, Beri A, Herzberg H, et al. (2023) Assessment of Intra-abdominal pressure with a novel continuous bladder pressure monitor-a clinical validation study. Life. 13(2):384.
[Crossref] [Google Scholar] [PubMed]
- Li Z, Lu F, Dai Y, Sheng M, Su L, et al. (2024) Knowledge, Attitudes and Practices (KAP) regarding intra-abdominal pressure monitoring among pediatric intensive care nurses: A cross-sectional study. Int J Nurs Sci. 11(3):381-386.
[Crossref] [Google Scholar] [PubMed]
- Grealy B, Johansson L, Coyer F (2019) Essential nursing care of the critically ill patient. Crit Care Nurs. 103.
[Google Scholar]
- Hunt LM (2017) The nurses' role in intra-abdominal pressure monitoring in the critical care setting (Doctoral dissertation).
[Google Scholar]
- El-gwaad ORRA, Mahmoud FH, Eldriny SNM (2022) Assessment of nurses' knowledge and practice regarding intra-abdominal pressure measurement and abdominal compartment syndrome prevention. Assessment. 89(1):4578-4586.
[Crossref] [Google Scholar]
- Geravandi S, Soltani F, Mohammadi MJ, Alizadeh R, Valipour A, et al. (2018) The effect of education on the nursing care quality of patients who are under mechanical ventilation in ICU ward. Data Brief. 16:822-827.
[Crossref] [Google Scholar] [PubMed]
- Hashmi M (2024) Knowledge competency score among critical care nurses concerning intra-abdominal hypertension measurement. J Nur Mid Pak. 1-7.
[Google Scholar]
- Xu X, He Z, Shan Y, Mao Q, Feng J, et al. (2021) Intra-abdominal pressure measurements in neurocritical patients. J Vis Exp. 11:(171)
[Crossref] [Google Scholar] [PubMed]
- Zou J, Zheng L, Shuai W, Li Q, Wang Q, et al. (2021) Comparison of intra-abdominal pressure measurements in critically ill patients using intravesical normal saline at 15°C, 25°C, and 35°C. Med Sci Monit. 27: e932804-1.
[Crossref] [Google Scholar] [PubMed]
- Crumley C (2022) Intra-abdominal pressure measurement devices: A technologic analysis. J Wound Ostomy Continence Nurs. 49(3):220-225.
[Crossref] [Google Scholar] [PubMed]
- Kaussen T, Gutting M, Lasch F, Boethig D, Dingemann J, et al. (2021) Continuous intra-gastral monitoring of intra-abdominal pressure in critically ill children: A validation study. Intensive Care Med Exp. 9(1):24.
[Crossref] [Google Scholar] [PubMed]
- Liao CH, Cheng CT, Chen CC, Wang YH, Chiu HT, et al. (2021) Systematic review of diagnostic sensors for intra-abdominal pressure monitoring. Sensors. 21(14):4824.
[Crossref] [Google Scholar] [PubMed]
- Tiwari SC, Rachit Agarwal DN, Tiwary IK, Goenka U, Afzalpurkar S, et al. (2020) Role of static and dynamic intra-abdominal pressure monitoring in acute pancreatitis. Pancreas. 49(5):663-667.
[Crossref] [Google Scholar] [PubMed]
- Candan Y, Akinci M, Eraslan O, Yilmaz KB, Karabacak H, et al. (2020) The correlation of intra-abdominal pressure with renal resistive index. J Surg Res. 252:240-246.
[Crossref] [Google Scholar] [PubMed]
- Augustin G (2023) Increased intra-abdominal pressure. In acute abdomen during pregnancy. Springer Int Pub. 45-73.
[Google Scholar]
- Smit M (2021) Intra-abdominal hypertension and abdominal compartment syndrome in critical illness: measure the pressure. Ann Intensive Care. 10:130.
[Crossref] [Google Scholar] [PubMed]
- Strang SG, Habes QL, Tuinebreijer WE, Verhofstad MH, Pickkers P, et al. (2021) Intestinal fatty acid binding protein as a predictor for intra-abdominal pressure-related complications in patients admitted to the intensive care unit; A prospective cohort study (I-fabulous study). J Crit Care. 63:211-217.
[Crossref] [Google Scholar] [PubMed]
- Gupta AK, Yadav E, Gupta N, Yelamanchi R, Bansal LK, et al. (2022) Role of intra-abdominal pressure as a prognostic marker and its correlation with APACHE II and SOFA scores in patients of acute pancreatitis. Ind J Sur. 1-7.
[Google Scholar]
- Song M, Zhao P, Hu W (2022) Application effect of intra-abdominal pressure monitoring system in early enteral nutrition nursing of icu patients contrast media and molecular imaging. Contrast Media Mol Imaging. 2022:3545278.
[Crossref] [Google Scholar] [PubMed]
- Laet IE De, Malbrain MLNG, Waele JJ De (2020) A clinician's guide to management of intra-abdominal hypertension and abdominal compartment syndrome in critically ill patients. Crit Care. 24(1):97.
[Crossref] [Google Scholar] [PubMed]
- Padar M, Starkopf J, Blaser AR (2021) Deepening of sedation with propofol has limited effect on intra-abdominal pressure-an interventional study in mechanically ventilated adult patients with intra-abdominal hypertension. J Crit Care. 65:98-103.
[Crossref] [Google Scholar] [PubMed]
- Rajasurya V, Surani S (2020) Abdominal compartment syndrome: Often overlooked conditions in medical intensive care units. World J Gastroenterol. 26(3):266-278.
[Crossref] [Google Scholar] [PubMed]
- Depauw P, van Eijs F, Wensing C, R Geuze, Santbrink H Van, et al. (2023) The Spine Intra-Abdominal Pressure (SIAP) trial. A prospective, observational, single arm, monocenter study looking at the evolutions of the IAP prior, during and after spine surgery. J Clin Neuro Sci. 113:93-98.
[Crossref] [Google Scholar] [PubMed]
- Lee RK, Gallagher JJ, Ejike JC, Hunt L (2020) Intra-abdominal hypertension and the open abdomen: Nursing guidelines from the abdominal compartment society. Crit Care Nurs. 40(1):13-26.
[Crossref] [Google Scholar] [PubMed]
- Isaias GC, Duenas C, Perales K, Juan ETD, Andres SG, et al. (2022) Approach to patient management in critical condition. Health Sci J. 16:1-26.
[Google Scholar]
- Guan X, Chen D, Xu Y (2024) Clinical practice guidelines for nutritional assessment and monitoring of adult ICU patients in China. J Intensive Med. 4(2):137-159.
[Crossref] [Google Scholar] [PubMed]
- Dugar D, Goel S (2024) Intra-abdominal pressure measurement as a predictor of postoperative wound complications in patients undergoing emergency laparotomy: A prospective observational study. Cureus. 16(2): e54860.
[Crossref] [Google Scholar] [PubMed]
- Pereira R, Buglevski M, Perdigoto R, Marcelino P, Saliba F, et al. (2021) Intra-abdominal hypertension and abdominal compartment syndrome in the critically ill liver cirrhotic patient-prevalence and clinical outcomes. A multicentric retrospective cohort study in intensive care. PLos One. 16(5): e0251498.
[Crossref] [Google Scholar] [PubMed]
- Nansubuga P, Mwanje AK, Kizito S, Obua D, Sendagire C, et al. (2020) The prevalence, incidence and mortality associated with intra-abdominal hypertension among patients in intensive care units of a low-income country: a cohort study. Open Res Afr. 3(53):53.
[Google Scholar]
- Qutob R, Alkhannani AHA, Alassaf T Y, Alhokail SO, Bagazi GA, et al. (2022) Physicians' knowledge of abdominal compartment syndrome and intra-abdominal hypertension in Saudi Arabia: An online cross-sectional survey study. Int J Gen Med. 15:8509-8526.
[Crossref] [Google Scholar] [PubMed]
- Saad HA, El-Taher Ak, Abo-alella HA, Riad M, Eraky ME, et al. (2023) Prospetive evaluation of the risk of compartmental intra-abdominal pressure on mortality in severe acute pancreatitis. Researchsquare.
[Google Scholar]
- Regli A, Nanda R, Braun J, Girardis M, Max M, et al. (2022) The effect of non-invasive ventilation on intra-abdominal pressure. Anaesthesiol Intensive Ther. 54(1):30-33.
[Crossref] [Google Scholar] [PubMed]
- Kryvoruchko IA, Olefir OS (2021) The assessment of the severity of patients with generalized intra-abdominal infection: An emphasis on the predictive value of reducing abdominal perfusion pressure in the complex treatment of patients. Acta Scient MED SCI. 5(11):17-26.
[Google Scholar]
- Caldas BS, Ascencao AMS (2020) Protocols for diagnosis and management of intra-abdominal hypertension in intensive care units. Rev Col Bras Cir. 47: e20202378.
[Crossref] [Google Scholar] [PubMed]
- Milanesi R, Caregnato RC (2016) Intra-abdominal pressure: An integrative review. Einstein (Sao Paulo). 14(3):423-430.
[Crossref] [Google Scholar] [PubMed]
- Iskus Health. (2017).
- Arksey H, O'Malley L (2005) Scoping studies: Towards a methodological framework. Int J Soc Res. 8(1) 19-32. ?
[Crossref] [Google Scholar]
- Malik MI, Burki AMK, Ameer K, Iqbal MR, Jalil A, et al. (2023) Intra-abdominal hypertension and its outcome in patients admitted in surgical icu after laparotomy. Paki Armed Force Med J. 73(2):549-52.
[Google Scholar]
- Gorad K, Prabhu V (2021) A study of intra-abdominal pressure measurement using a new innovative technique with foley's catheter. Med J Dr. DY Patil Uni. 14(5):492-495.
[Crossref] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: The prisma statement, Plos Med. 6(7):e1000097.
[Crossref] [Google Scholar] [PubMed]
Citation: Howthan AM (2024) Nursing Role for Intra-abdominal Pressure (IAP) Monitoring in Critical Care of Adult Patients: Scoping Review. J Intensive Crit Care. 10:41.
Copyright: © 2024 Howthan AM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.