Mini Review - (2016) Volume 2, Issue 4
Eftychia Karoutsou1*, Petros Karoutsos2 and Dimitrios Karoutsos3
1Ellinon Axiomaticon 17, Kareas, Athens, Greece
2Athens Medical Center, Gaia Maternity clinic, Vas Sofias 104, Athens, Greece
3Department of Obstetrics and Gynecology General Hospital of Rethymno, Athens, Greece
*Corresponding Author:
Eftychia Karoutsou
Ellinon Axiomaticon 17, Kareas, Athens, Greece
E-mail: eutuxiakaroutsou@yahoo.gr
Received date: November 04, 2016; Accepted date: November 21, 2016; Published date: November 28, 2016
Citation: Karoutsou E, Karoutsos P, Karoutsos D. Obesity and Endometrial Cancer: Is There a Role for Immunotoxicity? J Clin Epigenet. 2016, 2:4. doi: 10.21767/2472-1158.100032
Copyright: © 2016 Karoutsou E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Chronic inflammation and obesity are reciprocal pathophysiological processes underlying the element of the immune response. In obesity, alterations of cytokines are thought to contribute to a low grade inflammation within the adipose tissue affecting the development of several secondary diseases. Although micro-inflammation is involved in the initiation of immune response, excessive inflammation may promote tumor development. This review will discuss the reflexive relationship between endometrial cancer and obesity through immunomodulatory effects exerted by environmental chemicals.
Keywords
Environmental chemicals; Obesity; Cytokines; Hypertension
Introduction
Metabolic syndrome is characterized by hypertriglyceridemia, diabetes mellitus, and hypertension and insulin resistance. Obesity is a central player in the pathophysiology of the metabolic syndrome, via the secretion of excessive adipokines. These inflammatory cytokines such as tumor necrosis factor-α and interleukin 6 are elevated in obesity and are counterbalanced by anti- inflammatory cytokines such as adiponectin and visfatin [1]. Adiponectin, protects against liver fibrosis, due to its anti-inflammatory effect. On the other hand, inflammatory cytokines, such as tumor necrosis factor- a, decrease insulin release yet being already noxious for the development of fatty liver. For a long time neural and endocrine signals were studied for their impact on adipocyte metabolism and control of storage or release of fatty acids. In fact, bidirectional communication exists between adipocytes and other tissues [2]. Fat cells, through their integrated signals and inflammatory adipokine secretion, are responsible for immune system dysfunction; thereas, a major risk factor for endometrial and other types of cancer. Possible role that lipophilic pollutants stored in abdominal and visceral adipose tissue may play in the lipid metabolism and immunity function regarding the endometrial cancer will be discussed hereafter.
Obesity and Immunity Influential
Animal models offer important insight into how metabolic abnormalities linked to excess body weight can impair immunity. Diet-induced obese animals, present altered immunological parameters, such as lymphopenia, lower splenic mitogenic response and a tendency to lower cytotoxic activity of NK cells [3-5]. In addition, obese pigs, already having impaired metabolism, showed macrophages infiltration. These changes were associated with global DNA hyper methylation in both B-cells and T- cells [6].
Nevertheless, obese individuals show increased risk factors for severe infections and immune system dysfunction that may aggravate the immune response to vaccines [7]. The obese population did not respond to hepatitis B vaccination [8-10] and to tetanus toxoid [11]. Additionally, response to influenza vaccines has been reduced in obese individuals [12,13]. Obese individuals present with higher neutrophil, monocyte as well as total leukocyte counts [13] and suppressed lymphocyte responsiveness to mitogens [14-16].
The epigenetic mechanisms that link obesity to cancer seem to be multifactorial and to involve the interplay of metabolic and immune factors; the background behind these associations is only starting to be understood. Insulin resistance is a central player, but there are several other metabolic candidates including insulin-like growth factors and factors released by adipocytes, such as leptin and obesity-related inflammatory markers i.e., tumor necrosis factor-α and interleukin, the nuclear factor kappa beta (NF-κB) system and oxidative stress [17-19]. Obesity is a condition of chronic inflammation characterized by abnormal production of inflammatory cytokines with local and systemic effects that can contribute to the development of tumors [19]. Although local limited inflammation may be involved in the initiation of immune responses, excessive inflammation may promote tumor progression in steady-state conditions [20,21].
Of interest, Professor Giovanni De Pergola suggested that central fat accumulation and male gender independently increase the thickness of arterial wall, whereas inflammation and inflammatory markers do not exert an independent effect on this parameter [22]. Abdominal obesity is associated with vascular endothelial dysfunction, caused by reduced nitric oxide availability secondary to an enhanced oxidative stress production. Virdis et al. showed that tumor necrosis factor-α participates on the endothelin-1/ nitric oxide imbalance in small arteries from obese patients, implicating an inflammatory role for perivascular adipose tissue [23]. Notwithstanding, on examining the impact of obesity on treatment outcomes i.e., for prostate cancer, it was found that obesity was associated with higher-grade tumors, a trend towards increasing risk of positive surgical margins and higher biochemical failure rates [24]. Moreover, features of omental adipose tissue in endometrial cancer patients with different obesity phenotype have been associated with the clinical course of endometrial cancer; an inclination to correlation with better tumor differentiation was seen for UCP1 and CD68 protein expression in patients with 'metabolically healthy' obesity [25]. Further, adipose tissue is seen as endocrine organ, synthesizing so called adipocytokines - leptin, adiponectin, visfatin, that play a key role in the carcinogenesis of endometrial cancer and can be used as new markers for establishing the potential risk of this disease [26]. It could be said, that obesity wields impact on the development of vascular diseases, such as atherosclerosis or increases the risk of cancer, via pathways that involve hormonal control, cellular proliferation and even more significant immunity (Table 1).
| Immune factors activated by obesity | Clinical progression of diseases such as atherosclerosis or cancer |
|---|---|
| NLRP3, NLRP1, NLRP4 or AIM 2 inflammasomes | Vascular disease and brain disorders |
| CCR5 ligand and inflammatory chemokine MIP-1 | Oesophagogastric carcinoma |
| Increased levels of VEGF and IL-6 higher proportion of CD8+ T cells and NKT cells | Tumor progression |
| Activated proinflammatory CD4+ and CD8+ T cells | Oesophageal adenocarcinoma |
| NF-Kappa B a critical link | Cancer |
| Insulin resistance, hyperinsulinaemia, increased IGF-1 | Postmenopausal Breast Cancer |
| Leptin STAT 3, AP-1, ERK 2 and MARK Insulin signalling | Colon cancer |
| Cytokines, ROS, cell stress | Cancer |
| The adipokinesecretomeupregulation of proinflammatory adipokines | Cardiovascular diseases |
Table 1: Integrated disease inflammatory signals in response to obesity drive atherosclerosis and increase cancer risk.
'Since the early 1990s, researchers have tested recombinant cytokines, including IL-2, GM-CSF, and interferon, as local and systemic immunotherapies for cancer, in combination with chemotherapy in gene transfer experiments, and in vaccines— with limited success. These cytokines have also been studied for their potential antitumor properties since recombinant cytokines became available in sufficient quantities more than 20 years ago, starting with interferons and IL-2', said Oppenheim [27]. 'Only in the past few years have researchers begun focusing on the role that endogenous cytokines may play in increasing cancer risk' completing his train of thoughts. The pro-inflammatory cytokines can exacerbate the insulin resistance [17], while chronic overproduction by inflammatory cells of reactive oxygen species and cytokines, related to obesity, can induce mutagenic changes and DNA damage triggering cancer development [19]. Additionally as displayed by Frances Balkwill studies of cytokines in the microenvironment [28], certain cytokines are actually cancer-modifying genes. She found in fact that, in human ovarian cancer, the cytokine network is rich in proinflammatory cytokines, growth factors, and chemokines and that TNF-α in particular plays a central role in the microenvironment—in stromal development and regulation of matrix metalloproteinases required for tumor invasion.
What is immunotoxicity?
The immune system is directly integrated into the organism and interacts intimately with the functioning of many organs and organ systems. Immune function is particularly susceptible to disruption by environmental chemicals. Although major changes in the immune system are rapidly expressed in significant morbidity, and even mortality of the organisms involved, they are often preceded by subtle changes in some of its components that could be used as early tracers or as biomarkers per se [29]; this is of particular interest since these effects generally occur at levels lower than those causing toxic responses of the immune system [30]. But, how environmental chemicals influence the function of the immune system? Do they encumber the role of obesity in increasing cancer risk and what is the case of immunotoxicity and endometrial cancer?
Immunomodulatory Effects by Environmental Chemicals
Chemicals exert effects both at the cellular and the organic level of the immune system [30-33]. Observations in humans and studies in rodents have clearly demonstrated that a number of environmental and industrial chemicals can adversely affect the immune system. Exposure to asbestos, benzene, and halogenated aromatic hydrocarbons such as Polybrominated Biphenyls (PBBs), Polychlorinated Biphenyls (PCBs), and Dioxins (TCDD) can lead to immunosuppression in humans. Classical cytotoxic immunosuppressants act by inhibiting DNA synthesis. Others may act through activation of T-cells or by inhibiting the activation of helper cells [34-40]. While immunosuppression has been brought about in the past primarily to prevent rejection of transplanted organs, new applications involving mediation of the effects of interleukins and other cytokines are emerging [27]. Ιt was previously described that obesity, from a pathophysiologic point of view, balances on the edge of a precipice with the inflammation [41,42]; yet specific causal relationships are undetermined in human individuals. Consumption of a saturated fatty acid-rich diet resulted in a proinflammatory 'obesity-linked' gene expression, whereas consumption of a monounsaturated fatty acid-rich diet caused a more anti-inflammatory profile [43]. Dibutyltin (DBT) is known to affect the immune system in nanomolar concentrations; researchers tested the ability of DBT to alter production of cytokines in special immune cells, the macrophages. In this in vitro study, it was found that macrophages exposed to increasing amounts of DBT secreted increasing concentrations of two cytokines, interleukin-6 and tumor necrosis factor-α. Οf interest is that in these experiments, DBT inhibited the expression of genes involved in glucose metabolism and in the inflammation response [44]. Indeed [45], there is growing amount of evidence that organotins may be causing irreversible effects on the metabolic and immune systems. Organotins promote adipogenesis in vitro and in vivo [46]. Furthermore, developmental exposure in utero led to a fatty liver phenotype and enhanced lipid staining of neonatal fat depots resulting in a significant increase in the epididymal fat pad size of mice later in life [47]. The next step is the introduction of the term 'obesogen' as representing an environmental pollutant that adversely affects various aspects of adipose tissue functions (Figure 1) [48].
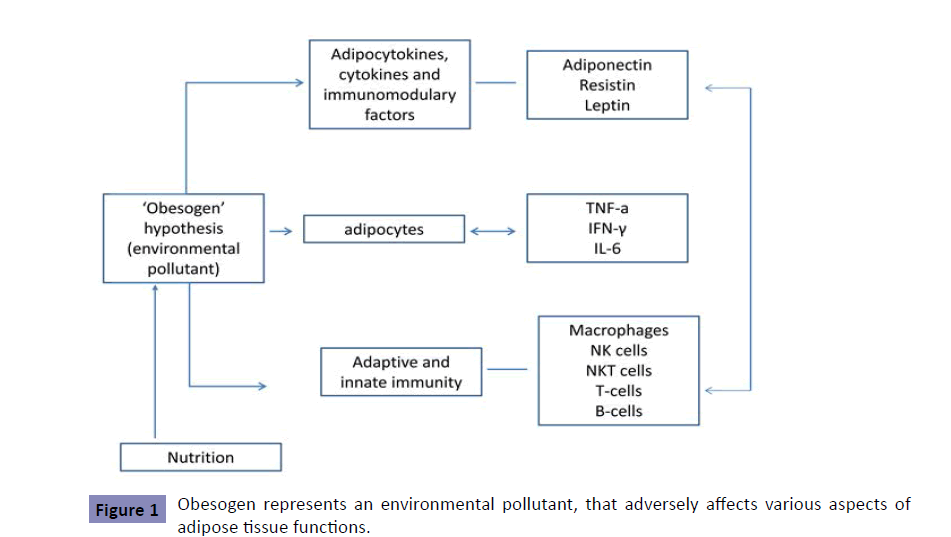
Figure 1: Obesogen represents an environmental pollutant, that adversely affects various aspects of adipose tissue functions.
More recently, the concept was extended to include substances that may modify metabolic balance at the hypothalamic level. In mice, TBT (tributyltin) is adipogenic at all ages and in both sexes and that it might be an ER activator in fat cells, These findings might help to resolve the apparent paradox of an adipogenic chemical being also an estrogen receptor activator by showing that the two apparently opposite actions are separated by the different doses to which the organism is exposed [49,50]. The environmental 'obesogen' hypothesis predicts that inappropriate receptor activation by organotins will lead directly to adipocyte differentiation and will render exposed individuals susceptible to obesity and immune- related metabolic disorders having already chosen the typical high-calorie, high-fat Western diet [46]. It is postulated that two prime candidate obesogens, tributyltin (TBT) and tetrabromobisphenol A [51], a related to BPA compound, could possibly at high levels of exposure predispose to all endpoints of obesity, such as endometrial cancer [49]. Indeed, BPA exhibited estrogenic activity, but there were remarkable differences. Tetrachlorobisphenol A (TCBPA) showed the highest activity, when being comparatively examined by means of different in vitro and in vivo reporter assays [51]. It was not until recently that gene expression analysis of human endometrial endothelial cells exposed to BPA revealed the paradox of decreased cell proliferation and increased cell death in response to BPA [52], offering important clues to the mechanisms of action of immunomodulating chemicals- a part of the 'obesogen hypothesis'.
Epilogue
The link that has been proposed between organotins and adipocyte differentiation opens an important new era of research into epigenetics on human health with respect to obesity and emerging diseases such as diabetes or neoplasia. Therefore, additional research directed at understanding the action of chemical obesogens at the receptor level will highlight the connection between obesity and cancer not independent of the exposure dose and may also reveal hidden new mechanisms regulating adipose tissue development. Concluding, immune dismodulation exerted by the environmental chemicals could be the first step in the multistage carcinogenesis.