Original Article - (2017) Volume 18, Issue 5
Department of Surgery, Surgical Oncology and Science, School of Medicine, Sapporo Medical University, Japan
Received June 13th, 2017 - Accepted July 29th, 2017
Objective The number of incidentally detected non-functional pancreatic neuroendocrine tumors is increasing; however, the tumor biology is largely unknown. This study aimed to reveal the oncological features and outcomes of curatively resected non-functional pancreatic neuroendocrine tumors. Methods and patients We retrospectively selected 31 patients with curatively resected non-functional pancreatic neuroendocrine tumors without distant metastasis from 52 consecutive patients who underwent surgery for neuroendocrine tumors in the hepato-biliary-pancreatic region at a single institute from 2003 to 2016. The impact on oncological outcome of tumor grade as determined by the Ki-67 proliferative index and lymph node metastasis was evaluated. Results Among the study patients, 58.1% were incidentally diagnosed. Seven patients (22.6%) showed lymph node metastasis, and recurrence was detected in 2 patients (9.4%) as liver metastasis. The median length of observation after operation was 46 months; the five-year disease-free survival rate was 89.4%. No deaths were recorded. At least one lymph node was evaluated independent of surgical procedures. Laparoscopic distal pancreatectomy with additional lymph node dissection around the celiac trunk showed similar quality of lymph node dissection as open distal pancreatectomy. G2 tumor grade was significantly associated with lymph node metastasis; however, preoperative diagnosis by endoscopic ultrasound-guided fine-needle aspiration showed limited sensitivity in G2 patients. Lymph node metastasis was significantly associated with recurrence. The patients with lymph node metastasis experienced a significantly lower fiveyear disease-free survival rate than those without lymph node metastasis. Conclusion Lymph node metastasis was associated with oncological outcome of non-functional pancreatic neuroendocrine tumors. Our surgical procedures contributed to obtaining lymph node information. Further studies are warranted for precise prediction of lymph node metastasis in nonfunctional pancreatic neuroendocrine tumors.
Endoscopic Ultrasound-Guided Fine Needle Aspiration; Neuroendocrine Tumors; Surgical Procedures, Operative
DFS disease-free survival; DP distal pancreatectomy; DPPHR duodenum-preserving pancreatic head resection; EUSFNA Endoscopic ultrasound-guided fine-needle aspiration; IPMN intraductal papillary mucinous neoplasm; ISGPF International Study Group on Pancreatic Fistula; Lap laparoscopic; LN lymph node; lyv-ne microinvasion lymphovascular or perineural microinvasion; MP middle pancreatectomy; NF-pNET non-functional pancreatic neuroendocrine tumor; PD pancreaticoduodenectomy; PDAC pancreatic ductal adenocarcinoma; POPF postoperative pancreatic fistula; SPN solid pseudo-papillary neoplasm
A pancreatic neuroendocrine tumor (pNET) is a rare disease which constitutes 1%-2% of all pancreatic cancers [1]. This tumor is clinically divided into two major categories; functional tumors with excess production of hormones and non-functional (NF) tumors without excess hormone production. The tumor biology is still largely unknown. For functional pNET, treatment is planned based on not only oncological, but also endocrinological aspects to relieve symptoms caused by adverse effects of the excess hormones. It has been reported that the incidence of pNET is increasing in Japan and the United States [2, 3]. In recent years, the incidence of non-symptomatic pNET with smaller size has increased, implying widespread and frequent use of high-resolution medical imaging in recent clinical practice [4, 5]. This change in demography emphasizes some controversies in the management of NF-pNET, especially when the tumor is small and non-symptomatic. Generally, pNET has a more indolent tumor biology than that of pancreatic ductal adenocarcinoma (PDAC), and there is no established way to precisely evaluate malignant potential. Intraductal papillary mucinous neoplasm (IPMN), the most common cystic tumor of the pancreas, also has more indolent features than PDAC. For IPMN, precise oncological evaluation, especially with the goal of evaluating malignant potential, has been pursued by means of cumulative findings and the establishment of clinical guidelines [6, 7, 8]. In this context, it seemed useful to review and analyze cases for the purpose of shedding light on the tumor biology of NF-pNET. The present study focused on curatively resected NF-pNET with the goal of clearly revealing oncological features and tumor behavior after curative resection. First, we evaluated the impact of our surgical procedures, especially concentrating on lymph node (LN) dissection. Then, we investigated the influence of tumor grade determined by the Ki-67 proliferative index and LN metastasis as important malignant features of NFpNET to assess oncological outcome.
Data Collection
Fifty-two patients underwent surgery for neuroendocrine tumors in the hepato-biliary-pancreatic region including the duodenum consecutively from January 2003 to December 2016 at Sapporo Medical University Hospital. These patients were retrospectively analyzed, and 31 patients with NF-pNET were selected for analysis according to the following criteria: A) exhibited no symptoms or signs suggestive of excess hormone production, B) showed no distant metastasis in preoperative diagnostic imaging or intraoperative observation and underwent curative pancreatic resection, C) had pathologically proven primary pNET in the pancreas, D) received observation for more than six months after operation. For these 31 patients, information on clinical presentation, demographics, surgical procedure, postoperative course, pathological diagnosis, and followup including recurrence and survival were collected from the medical records at Sapporo Medical University Hospital. The study was approved by the Institutional Review Board and conducted in adherence with the Declaration of Helsinki.
Surgical Procedures
Basically, pancreaticoduodenectomy (PD), mainly pylorus-preserving PD, was conducted for pancreatic head lesions. Distal pancreatectomy with splenectomy (DP) including total resection of the pancreatic tail with or without total resection of the pancreatic body, was conducted for lesions of the pancreatic body and tail depending on locations. In PD and DP, regional peripancreatic lymph nodes were dissected. Further lymph node dissection around the celiac trunk, common hepatic artery, hepatoduodenal ligament, or superior mesenteric artery was conducted depending on tumor status and the surgeon’s discretion. Six patients underwent laparoscopic distal pancreatectomy (Lap-DP). We applied the techniques of laparoscopic gastric cancer surgery to Lap-DP for additional lymph node dissection around the celiac trunk, common hepatic artery or proximal splenic artery, in anticipation of obtaining more information regarding LN status. Pancreatic parenchyma-preserving resection such as middle pancreatectomy (MP) or duodenum-preserving pancreatic head resection (DPPHR) was conducted depending on tumor status and the surgeon’s judgment. Even in MP and DPPHR, at least one lymph node was harvested. Postoperative pancreatic fistula (POPF) was graded according to the classification of the International Study Group on Pancreatic Fistula (ISGPF) [9].
Pathological Analysis
In addition to routine diagnosis by hematoxylin and eosin (H & E) staining, immunohistochemistry for chromogranin A (CgA), synaptophysin, or CD56 was used to diagnose NET. All cases were reviewed and classified according to the World Health Organization 2010 (WHO 2010) classification with determination of the Ki-67 proliferative index. The tumor factor, LN status, and quality of resection were evaluated according to the classification of the Union for International Cancer Control (UICC) [10].
Statistical Analysis
Continuous variables are described as median and range. Qualitative variables are described as nominal scales and percentages. Comparison of continuous variables and qualitative data between two groups were conducted by the Mann-Whitney U test and Fisher’s exact test, respectively. Disease-free survival (DFS) was defined as the time from operation to disease recurrence. A patient was censored at the last observation time if no event had occurred. Survival curves were plotted by the Kaplan-Meier method and compared by the log-rank and Wilcoxon tests. Binomial logistic regression analysis was performed to determine associations between the variables that were significant in univariate analysis and LN metastasis. Receiver operating characteristic (ROC) analysis was conducted to analyze the cut-off value of tumor size, which is the most predictive of LN metastasis. Statistical analysis was performed using GraphPad Prism 7 software (GraphPad Software, Inc.; La Jolla, CA, USA) and IBM SPSS Statistics v. 20 (IBM Japan; Tokyo, Japan).
Demography, Surgical Procedures, Pathological Findings, and Outcomes of the 31 Study Patients
Thirty-one patients who underwent curative resection for NF-pNET without distant metastasis at the time of resection were selected for analysis over the 14-year study period (Table 1). In this retrospective cohort, 13 patients (41.9%) manifested symptoms before surgery. The most frequent symptom was weight loss (n=4), and the second most frequent symptom was back pain (n=3) or abdominal pain (n=3). In addition to PD and DP, pancreatic parenchyma-preserving resection, such as MP or DPPHR, was performed for 7 patients (22.6%). Laparoscopic DP was conducted in 6 patients (19.4%). All of the other operations were conventional open laparotomy. According to the WHO 2010 classification, 51.6%, 45.2% and 3.2% of patients were diagnosed as having G1, G2 and NEC tumors, respectively. Lymphovascular or perineural (ly-v-ne) microinvasion was observed in 12 patients (38.7%). LN metastasis was observed in 7 patients (22.6%). The R0 resection rate was 96.8%. Only one patient who was diagnosed with a solid pseudo-papillary neoplasm (SPN) preoperatively underwent R1 resection by Lap-DP due to peripancreatic invasion of a G2 NF-pNET. Radical open resection of the pancreatic bed, remnant pancreatic body, and left prerenal fascia with extended LN dissection was conducted after the initial operation.
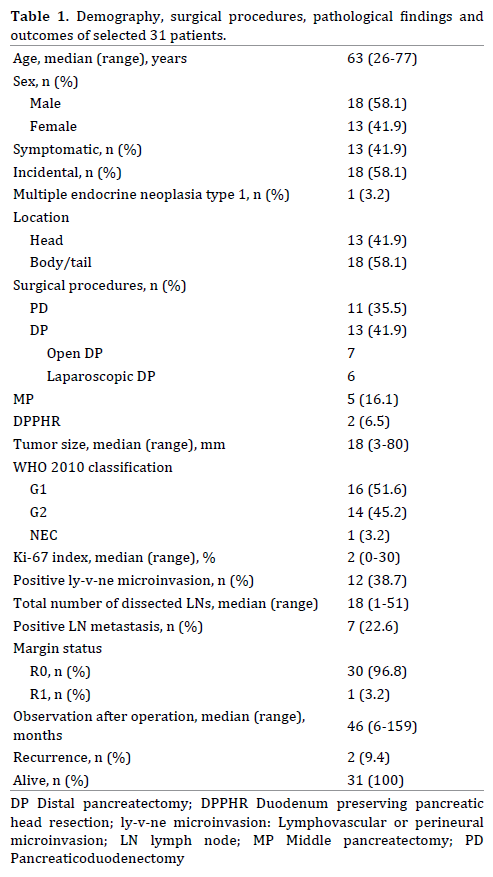
Recurrence occurred in 2 patients (3.2%), which was detected only in the liver at 29 and 38 months after surgery, respectively, and there were no local recurrences recorded in either of the patients. All study patients were alive within the median observation period of 46 months. The five-year DFS rate was 89.4% (Figure 1a).
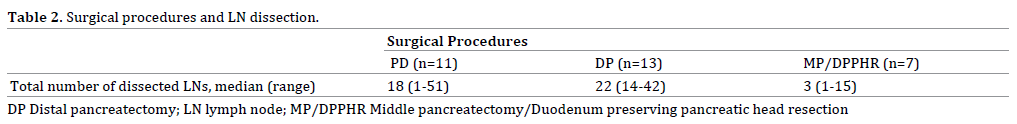
Surgical Procedures and LN Dissection
The impact of type of operation on LN dissection was evaluated (Table 2). In all types of surgery, at least one LN was always harvested and then pathologically evaluated. The total number of dissected LNs was significantly higher in patients who underwent PD (P=0.004) and DP (P<0.001) than in the patients who received pancreatic parenchymapreserving surgery; however, there was no significant difference between PD and DP (P=0.638).
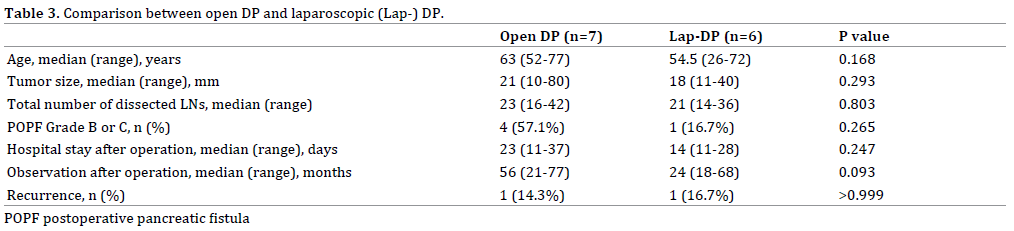
Further evaluation was performed between open DP and Lap-DP (Table 3). We conducted additional lymph node dissection around the celiac trunk, common hepatic artery, and proximal splenic artery during Lap-DP. Pathological diagnosis revealed that six LNs on average were evaluated in addition to peripancreatic LNs after Lap-DP. There were no significant differences between patient age, tumor size, total number of dissected LNs, outcome including the rate of POPF, length of hospital stay and observation after operation, and recurrence rate. We conjectured that Lap-DP with additional LN dissection around the celiac trunk, common hepatic artery, and proximal splenic artery were as feasible as open DP for the quality of LN dissection and gross outcome.
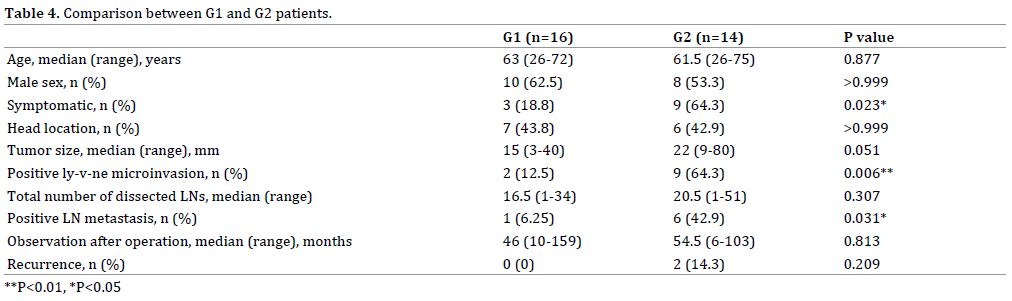
Tumor Grade and Features
Features of G2 patients (n=14) were compared with those of G1 patients (n=16) (Table 4). Univariate analysis showed no significant differences in tumor size, total number of dissected LNs, length of observation, or recurrence rate between G2 and G1 patients. The 5-year DFS rates of G2 and G1 patients were 79.5% and 100%, respectively, with no significant difference (P=0.164 by the log-rank test and P=0.1687 by the Wilcoxon test). However, the G2 patients were significantly more symptomatic than the G1 patients, with high prevalence of ly-v-ne microinvasion and LN metastasis.
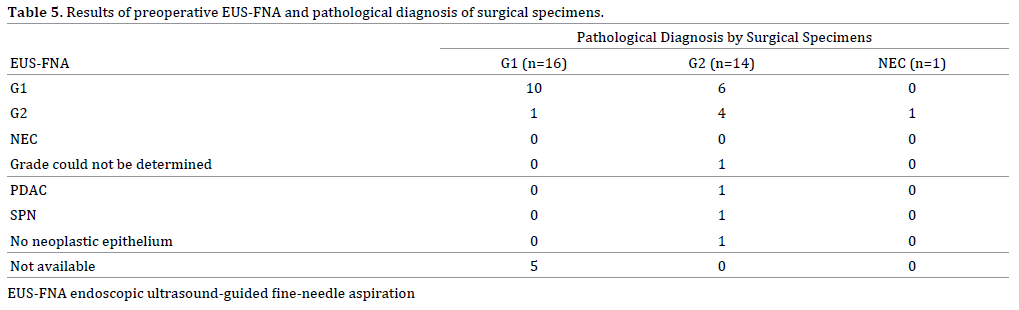
Pathological information about preoperative endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) was available in 26 of the patients (Table 5). The EUS-FNA specimens were diagnosed as NET in 23 patients (88.5%). In the other 3 patients, one patient was diagnosed with PDAC, one patient was diagnosed with SPN, and the final patient was diagnosed as not having neoplastic epithelium. The WHO 2010 grade according to Ki-67 staining could be determined in 22 of the patients. The grade of surgical specimens matched the EUS-FNA findings in 14 patients, for a concordance rate of 63.6% (14/22). The positive predictive value (PPV) of the EUSFNA results was 62.5% (10/16) for G1 and 66.7% (4/6) for G2. However, in the 14 patients with G2 who were diagnosed via surgical specimens, only 4 of those patients were diagnosed by preoperative EUS-FNA, indicating that the sensitivity in the G2 patients was 28.6% (4/14). On the other hand, the sensitivity in the G1 patients who underwent EUS-FNA was 90.9% (10/11).
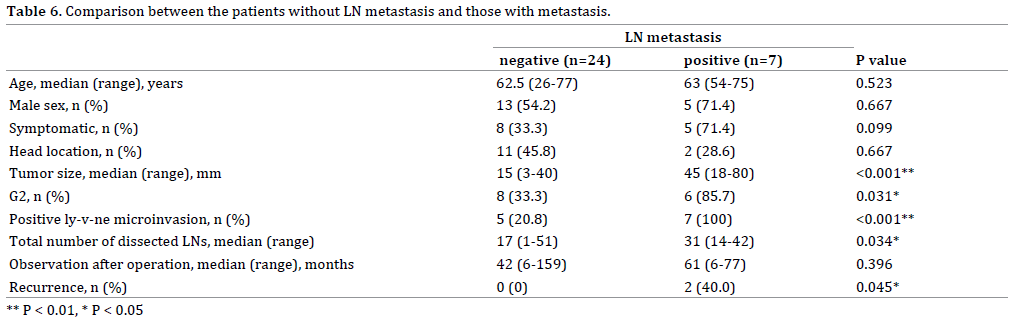
LN Metastasis and Features
The G2 tumor grade was significantly associated with LN metastasis; however, preoperative diagnosis by EUSFNA showed limited sensitivity in the G2 patients. To reveal the detailed features of LN metastasis in NF-pNET, the patients with LN metastasis (n=7) were compared with the patients without LN metastasis (n=24), as summarized in Table 6. Among the patients with LN metastasis, the tumor size and the total number of dissected LNs were significantly larger, and there was a higher prevalence of ly-v-ne microinvasion and G2 tumors than in the patients without metastasis. Finally, LN metastasis was significantly associated with recurrence. The 5-year DFS rates of the patients with and without LN-metastasis were 62.5% and 100%, respectively, with statistically significant difference (P=0.019 by the log-rank test and P=0.020 by the Wilcoxon test) (Figure 1b). Multivariate analysis was performed to determine predictive variables for LN metastasis or recurrence from the significant factors found through univariate analysis. No independent predictive variables were detected by binomial logistic regression analysis (data not shown). From ROC analysis of the tumor size, a cut-off size of 20. 5 mm was determined to predict LN metastasis, which showed an area under the curve (AUC) value of 0.893 (P<0.001), sensitivity of 0.857, and specificity of 0.792 (Figure 2).
NF-pNETs without excess production of hormones are less symptomatic than functional pNETs. At present, the number of non-symptomatic NF-pNETs with small tumor size that are incidentally discovered is increasing. Vagefi et al. reported that in the early 2000s, the majority of surgically resected pNETs were non-functional (65.9%) and were incidentally discovered (60.4%) [4]. In another study, the tumor size of incidentally discovered and surgically resected NF-pNETs ranged 4 mm to 170 mm, with a median size of 30 mm [11]. In our cohort, 58.1% of the NF-pNETs were discovered incidentally without symptoms during medical exams for the other diseases and regular medical checkups. Tumor size ranged from 3 mm and 80 mm, with a median size of 18 mm, which was smaller than in previous reports [4, 11]. These features might depend on the data collection period, as the data on our patients were collected from 2003 to 2016, for the latest 14 years.
Pancreatic parenchyma-preserving resections—MPs and DPPHRs—were performed in 22.6% of the patients in our cohort. The total number of dissected LNs was significantly lower in parenchyma-preserving resections than in PDs and DPs, as previously reported [12], although at least one LN was always harvested to evaluate LN status as much as possible. There were no local recurrences and disease-specific or non-specific deaths recorded among our study patients; the median length of observation was 46 months after curative resection. We compared the patients who underwent Lap-DP with the patients who received open DP, noting the comparable quality of LN dissection and oncological outcome. The performance of Lap-DP has become more widespread as a minimally invasive surgery (MIS) for pNET. A meta- analysis of the MIS approach specific for pNETs suggested better short-term outcomes [13]. Oncological indications for parenchyma-preserving resection or LN dissection are more complicated and represent a controversial topic for treating NF-pNET. Fernández-Cruz et al. reported acceptable oncological outcomes of laparoscopic enucleation for NF-pNET with regional LN dissection, paying close attention to the status of LNs [14]. Recurrence of G1 NF-pNET at a local LN was reported after spleen-preserving DP without LN dissection [15]. Lombardi et al. [16] pointed out that 39% of NFpNETs with a size of ≤ 2 cm showed malignant potential, including distant metastasis, local LN metastasis, and local infiltration. Furthermore, among 40 resected NF-pNETs, with size ranging from 1 cm to 2 cm, two disease-specific deaths were reported [17]. In contrast to these data on individuals, Conrad et al. [18] analyzed surgically resected pNETs without distant metastasis from a large database and found that LN metastasis was a negative predictor for survival only when tumors were confined to the pancreas; extended LN dissection did not show significant survival advantage in any stage group. Further accumulation of surgical cases of NFpNET and prospective randomized control trials are urgently needed to determine detailed indications for parenchymapreserving resection and LN dissection.
In our cohort, G2 patients were significantly more symptomatic, with a higher prevalence of ly-v-ne microinvasion and LN metastasis. However, there were no significant associations between G2 and tumor size, recurrence rate, or DFS. We conjectured that our cohort without distant metastasis was diagnosed and resected at the very early stage of tumor development before the differences between G1 and G2 tumor were manifested clearly. The other possibility was that the accuracy of preoperative tumor grade evaluation might have influenced the subsequent treatment plan (i.e., surgical procedure or extent of LN dissection) and consequently the oncological outcome. The concordance rate of our preoperative EUS-FNA was 63.6%, which was relatively lower than the rate of 74% to 89% in previous studies [19, 20, 21]. Furthermore, only 28.6% of the G2 patients were diagnosed by preoperative EUS-FNA, highlighting need for caution in depending on EUS-FNA to make treatment decisions. LN metastasis was found to be significantly associated with DFS, recurrence rate, larger tumor size, and higher rate of G2 and ly-v-ne microinvasion. Venous or perineural microinvasion has also been reported as an independent predictor of recurrence [22, 23]. In our cohort with a lower number of total and recurrent cases than in the previous reports, ly-v-ne microinvasion was not associated with recurrence (P=0.141). ROC analysis revealed that the prognostic cut-off value of tumor size for LN metastasis was 20.5 mm, which was within the range of previous reports, although the cut-off value widely varied among previous studies, ranging from 15 mm to 40 mm including pathological and radiological size [12, 24, 25, 26, 27, 28, 29]. LN metastasis might be difficult to predict precisely based on routine clinical information such as symptoms, tumor size, and tumor grade. Recently, Jiao et al. detected frequently mutated genes in pNET; important gene alterations in pNET were almost completely different from common gene mutations in PDAC and newly discovered gene mutations in IPMN [30, 31], suggesting unique tumorigenic mechanisms of pNET that are distinguished from PDAC and IPMN. The genetic and molecular pathogenesis of pNETs is important fundamental information for future improvements in prognosis and selection of treatment [32]. Further studies are warranted.
A limitation of the present study was that it was a retrospective analysis of a small number of patients in a single institute. In addition, preoperative diagnosis of tumor grade by EUS-FNA might have influenced the selection of the surgical procedures and consequently the outcomes. Another limitation was that the small number of total and recurrent cases hindered the detection of independent predictive factors.
The present study retrospectively analyzed the features of curatively resected NF-pNET without distant metastasis. In accordance with the current trend, the majority of cases were incidentally detected. The 5-year DFS rate was 89.4% with no deaths. At least one LN was evaluated independently of surgical procedures. Lap-DP with additional LN dissection around the celiac trunk demonstrated feasible outcomes comparable to the outcomes of open DP. Tumor grade of G2 was significantly associated with LN metastasis; however, preoperative diagnosis by EUS-FNA showed a limited sensitivity in G2 patients. LN metastasis was significantly associated with recurrence, and the cut-off value of tumor size for predicting LN metastasis was 20.5 mm. Further studies are needed for better prediction of LN metastasis and selection of treatment.
None of the authors have any conflict-of-interest to disclose related to this article.