Case Report - (2024) Volume 8, Issue 3
Received: 30-Jan-2020, Manuscript No. IPOM-24-3285; Editor assigned: 04-Feb-2020, Pre QC No. IPOM-24-3285 (PQ); Reviewed: 18-Feb-2020, QC No. IPOM-24-3285; Revised: 01-Jul-2024, Manuscript No. IPOM-24-3285 (R); Published: 29-Jul-2024, DOI: 10.36648/ipom.8.3.22
Psoriasis is a relatively common immune mediated, chronic, genetically determined, scaly inflammatory disease which primarily affects the skin and secondarily the joints. Various sources have noted the prevalence rates of this condition as between 1% to 2% and 2% to 4%, with ranges from between 0.5% to 4.6% of the population. The most common form of the psoriasis is the plaque type, also known as psoriasis vulgaris, which accounts for approximately 90% of occurrences. The most common anatomical locations of these lesions occur on the elbows, knees, scalp, fingernails and toenails.
Psoriasis; Plaque; Chronic; Anatomical locations
On the other hand, oral psoriasis of the tongue is an extremely rare condition. Oppenheim first reported upon the histopathology of oral psoriasis in 1903. Younai and Phelan reported in 1997 that only 57 cases measured up to confirming a diagnosis of oral psoriasis. Lier, et al. reported that the occurrence of true psoriatic oral mucosal lesions has been disputed in the past and that only another seven cases were identified as of 2009 and that of these 64 reported cases, only 11 of these cases demonstrated characteristic psoriatic lesions of the tongue and in 5 of those 11 cases, cutaneous psoriatic lesions were not present. Mattsson, et al., noted that the diagnosis of oral mucosal psoriatic lesion is problematic as there is currently not an accepted clinical or histopathologic set of criteria. This is also complicated by variable appearance of lesions diagnosed as oral mucosal psoriatic lesions and tends to make diagnostic absolute certainty impossible [1].
Vander Wall and Pindborg described four types of clinical presentations of oral psoriasis: 1) well-defined, gray to yellowish white, very small roundish lesions; 2) lacy, circinate, elevated white lesions of the oral mucosa, including the tongue, which paralleled cutaneous lesions; 3) fiery red erythematous oral lesions corresponding with acute cutaneous lesions and 4) Benign Migratory Glossitis (BMG) which occurs more frequently in patients with cutaneous psoriasis compared to patients without psoriasis.
The association of psoriasis with both fissured tongue and BMG (also known as geographic tongue) is well documented. The prevalence of fissured tongue ranges between 9.8% to 47% and the prevalence of BMG ranges between 5.6% to 8.1% in patients with cutaneous psoriasis.
The prevalence of BMG over-all is between 1% to 2% of the population. Picciani, et al, reported that the oral condition fissured tongue has an incidence of between 5% to 10% of the worldwide population [2].
A 66-year-old patient presented to a private oral medicine clinician in early November 2017, with a chief complaint of, “Burning tongue, red at the tip, white bumps in rear, cuts in tongue lesion and bad taste.” His physician had previously placed him on a nystatin topical rinse for one week without any resolution of the condition. The condition had been ongoing for approximately two and a half months and the patient reported issues with speaking. The patient had changed tooth pastes, to a tooth paste believed to be sodium lauryl sulfate free. Eating spicy foods was not problematic. The patient’s pain was negligible (2 out of 10) upon awakening and increases throughout the day. The condition did not interfere with sleep. The patient was taking apixaban for atrial fibrillation, atorvastatin for cholesterol lowering, lansoprazole for gastric reflux and fexofenadine and azelastine for seasonal allergies, along with a vitamin D supplement. The patient reported no known drug allergies [3]. Clinically, there was no lymphadenopathy noted. The anterior dorsal tongue was noted for erythema and the remaining oral tissues appeared to be within normal limits. The differential diagnosis consisted of hypersensitivity reaction, irritation reaction, oral candidiasis and dysgeusia. The patient was referred to an allergy & immunology physician for food hypersensitivity evaluation in late November and the evaluation studies were negative. The patient reported that his tongue seemed to be doing better and he suspected the reason was that he had removed paprika from his diet. However, the patient’s oral burning symptoms returned in January and the patient was scheduled for a biopsy procedure. The biopsy procedure and histological examination were performed in late January 2018 and pathology reported positive PAS staining for candidiasis. The histopathology slide at medium magnification exhibited elongated rete pegs. The papillary connective tissue was noted for lymphocytic inflammation and dilated blood vessels approximating the epithelial margins. Lower magnification showed marked collections of neutrophils seen in the parakeratin noted as munro abscesses. The patient was placed on a two-week regimen of daily 100 mg fluconazole tablets. But the condition worsened. The patient was then referred to otolaryngology for a fungal DNA identification culture and sensitivity assay. The culture was negative for candida, aerobic, anaerobic or acid-fast bacilli. The otolaryngologist elucidated that the patient had previously been treated for cutaneous psoriasis and the patient also reported a history positive for psoriasis which began as a teenager. He reported that he had had dry red blotchy lesions of the legs, trunk and face. His dermatologist had prescribed calcipotriene ointment for the trunk and leg lesions and desonide for his facial lesions. The medications were sufficient to control the condition. The patient did not remember having psoriatic lesions when the tongue lesions first presented in the late summer of 2017, although, he was not sure whether there were cutaneous psoriatic lesions at that time. The oral medicine clinician, with a new working diagnosis of oral psoriasis, prescribed a topical dexamethasone elixir rinse regimen. The patient’s lesions resolved.
The patient was asked to discontinue the steroid rinse as a challenge and in two weeks the erythema and sensitivity returned. On resuming the topical steroid regimen, the lesions once again resolved. The patient was referred to his dermatologist to consider a biologic therapeutic, but the dermatologist deferred in that the topical rinse seemed to be effective and was a more conservative approach (Figures 1 and 2) [4].
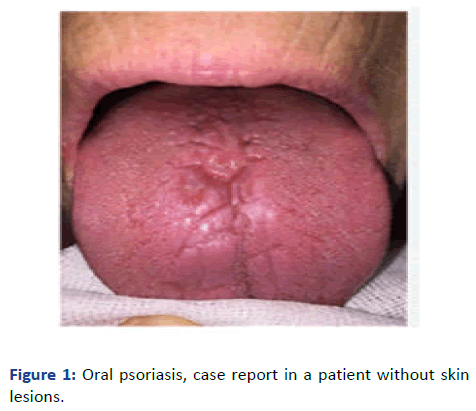
Figure 1: Oral psoriasis, case report in a patient without skin lesions.
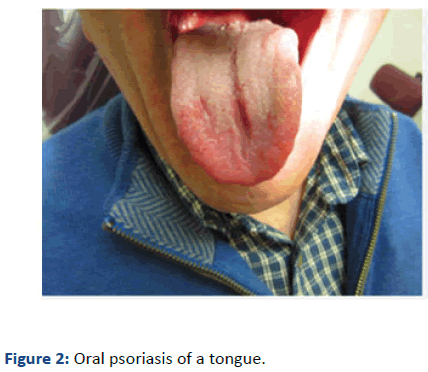
Figure 2: Oral psoriasis of a tongue.
As demonstrated by this case, oral psoriasis lesions are often misdiagnosed for other, more common pathologies. A definitive diagnosis can be challenging due to several factors including an unclear etiology, ill-defined clinical and histopathologic criteria and rare occurrence with a variety of presentations. A differential diagnosis for any suspected oral psoriasis lesion should include lichen planus, syphilis, lupus erythematous, cicatricial pemphigoid, pemphigus, candidiasis, reiter’s syndrome and smoking or trauma. To rule out these different diagnoses and arrive at the correct conclusion, three components have proven useful, namely a) careful patient history, physical exam and biopsy with histological examination [5].
Most oral psoriasis lesions appear in the context of cutaneous lesions, either presenting simultaneously or presenting in patients with a history of dermal psoriasis, as was the case with this patient. A careful patient history is crucial to elucidating such crucial details. After a patient history, it is imperative to conduct a thorough exam of the patient’s skin for psoriatic lesions. Such lesions are often asymptomatic and may be in progression or regression unbeknownst to the patient. Identification of any cutaneous psoriatic lesions would elevate the diagnosis of oral psoriasis in the differential.
Even yet, isolated cases of oral psoriasis have been reported and the diagnosis cannot be ruled out based on a negative history and physical exam alone. A biopsy with Periodic Acid- Schiff-Diastate (PAS-D) staining is often useful to distinguish between a superficial fungal infection and psoriasis. In general, pathologic changes seen within the mucous membranes parallel those of cutaneous psoriasis-elongation and thickening of rete ridges with overall acanthosis. The papilla of lamina propria is elongated and edematous. More specific immunohistochemical staining for factors such as VEGF and TNF-α is useful in a more definitive diagnosis of oral psoriatic lesions. Even so, as reported in this case, initial biopsies may be misleading and the clinician must continue to maintain a global picture of the three pillars of diagnosis, that is patient history, physical exam and labs or biopsies. Continued follow-up and flexibility in treatment are fundamental to arriving at the correct diagnosis, especially in an ambiguous disease process such as oral psoriasis. In the case presented, the biopsy initially reported inflamed oral mucosa with candidiasis. However, after refractory antibiotic treatment, a subsequent biopsy was performed that was negative for candidiasis leading the clinician to inquire more about possible cutaneous psoriasis whereupon the patient revealed a history of dermal psoriasis in his teenage years. People with dermal psoriasis are known to be more susceptible to oral psoriasis or geographic tongue. Histologically, oral psoriasis and geographic tongue are similar, but presents in different locations. Many times, geographic tongue exhibits a prominent white serpentine border and erythematous center while oral psoriasis has a white border that is either less prominent or not present [6].
Management of oral psoriasis covers a spectrum of treatments ranging from nonintervention to biomarker testing and biologic therapy to skin grafting. For asymptomatic lesions, treatment is not necessary and undoubtedly many of these lesions are unreported. Commonly, oral psoriasis can cause erythema, bleeding, plaque or ulcers and symptoms of discomfort such as pain, loss of taste and hypersensitivity. For irritant driven lesions, lifestyle modifications focused on removing the irritant are preferred. Common irritants include spicy foods, smoking and abrasive dentures or teeth. For nonirritant related lesions, first line treatment typically centers around palliative care using topical anesthetics such as viscous lidocaine, diphenhydramine and alkaline rinses have all been reported to provide relief.
Corticosteroids are also useful to reduce inflammation and suppress the migration of polymorphonuclear lymphocytes. Often regression of the psoriatic lesion is observed and these patients have a good prognosis long term. For patients refractory to this care, advances in the understanding of cytokines and inflammatory disease processes have introduced a new field in the therapeutic treatment of psoriasis. Historically anti-TNF agents developed for rheumatology and gastroenterology have been used with some success in treating psoriasis. Etanercept, introduced in 2004, was the first FDA approved biologic for dermatologic treatment and has a safe and efficacious record. Recently, much progress has been made in understanding the role of the IL-23/Th17 signaling pathway in immune-mediated diseases. Biologics such as ixekizumab and secukinumab that disrupt IL-17 or its receptor in the case of brodalumab, are highly effective and safe in treating moderate to severe psoriasis. To be complete, these therapies are primarily intended to treat dermal psoriasis, but with the close relation and often co-presentation of both dermal and oral psoriasis, the clinician may consider their use in severe oral psoriasis. Referring to the patient presented, because the topical rinses were effective, biologic treatment was not pursued [7].
Currently, much research is being made in the field of biomarkers for the strategic diagnosis and treatment of psoriasis. Unfortunately, at this time, no biomarkers specific to psoriasis of any type have been identified, but researchers remain hopeful biomarkers will yield novel strategies and treatments to improve patient management and outcomes. Surgery such as gingival grafting should be reserved for candidates refractive to medical therapy.
Lastly, consideration must be given to the simultaneous presentation of oral psoriasis with another disease on the differential, most often candidiasis. While treatment of many oral lesions is straightforward, the astute clinician must always consider the potential overlap of multiple disease processes, complicating both diagnosis and treatment [8].
While rarely reported, oral psoriasis is a diagnosable lesion with effective and adequate treatments. The patient presented follows the classic storyline of misdiagnoses and mistreatment often due to a misleading biopsy and/or incomplete history. Although cases of isolated oral psoriasis have been reported, due to its close relation with its dermal cousin, a patient history or physical exam finding of dermal psoriasis is a notable clue in diagnosing oral psoriasis. Treating oral psoriasis should be pursued in a step-wise fashion beginning with irritant removal and escalating treatment as necessary to palliative care and eventually biologic therapy. Grafting and other surgical procedures should be considered after all medical treatment has been considered. Oral psoriasis is an uncommon ailment that can be effectively diagnosed and treated through common medical practices including a thorough patient history, methodical physical exam, confirmatory testing and continued patient-physician dialogue.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ferris W (2024) Oral Psoriasis Case Report. J Ora Med. 8:21.
Copyright: © 2024 Ferris W. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.