- (2015) Volume 16, Issue 3
Kim V Ånonsen1,4, Trond Buanes2,4, Bård Ingvald Røsok2, Truls Hauge1,4, Bjørn Edwin3,4
Department of 1Gastroenterology, 2Gastroenterological Surgery, 3The Interventional Centre and 4Institute of Clinical Medicine Oslo University Hospital and University of Oslo, Oslo, Norway
Received February 12th, 2015 – Accepted March 28th, 2015
Context Recent guidelines for the management of cystic lesions of the pancreas recommend observation for selected neoplasms using imaging criteria. However, current imaging modalities lack diagnostic accuracy, and the indication for surgery is debated. Objective In this study we have explored the outcome of laparoscopic distal pancreatic resections in all patients referred with potential pancreatic cystic neoplasms, with histological diagnosis as endpoint. Methods Between 1997 and 2009 all patients referred to our tertiary referral centre having a cystic neoplasm of the distal pancreas accepted for surgery, were included in the present observational study. Results A total of 69 patients were included. Sixty two patients underwent distal pancreatectomies, in whom 19 were spleen-preserving, and 7 enucleations were performed. Two procedures were converted to open technique. The lesions removed in 27 patients (39%) were either malignant or premalignant. The final diagnoses were serous cystic neoplasm (n=29), mucinous cystic neoplasm (n=12), pseudocyst (n=11), solid pseudopapillary neoplasm (n=10), intraductal papillary mucinous neoplasm (n=5) and other (n=2). Overall morbidity was 33%; 56% of the complications were classified as mild. Fistula rate was 10%. One patient died postoperatively from a cerebral haemorrhage. Conclusion Most complications after laparoscopic distal resection of cystic pancreatic lesions are mild, but the proportion of patients with benign lesions (61%) has to be reduced by focused preoperative investigations. Endoscopic ultrasound examination (EUS), enabling aspiration of cyst fluid and fine needle aspiration is an additional option for the preoperative workup.
Pancreas
During the last decade, treatment of cystic pancreatic lesions has changed radically. Numerous guidelines have emerged to advise clinicians [1-3]. Previously, all cystic pancreatic lesions apart from pseudocysts were considered for surgery. Today consensus advocates observation in selected patients based on imaging criteria. However, management guidelines relate to specific histopathologic entities, which frequently remain unknown preoperatively [4, 5]. Recent literature has focused on the outcome of a stratified management. The international consensus working group’ recommendations, the “Sendai guidelines”, were updated in 2012, and a larger proportion of sidebranch intraductal papillary mucinous lesions (SB-IPMNs) may be considered for serial imaging, compared to the 2006 guidelines. On the other hand, in patients with small SB-IPMNs (“Sendai negative”) undergoing surgery at a large pancreatic centre in Germany, one in five cysts were found to harbour malignancy [6], highlighting the debate on indication for surgery in this setting [7, 8].
In our tertiary pancreatic centre, the threshold has been low for laparoscopic surgery in patients with distal cystic pancreatic tumours. Surgery includes both a diagnostic and for some patients a therapeutic procedure. It is important to evaluate this approach as current guidelines have limited the indication for surgery. The present investigation was initiated prior to the implementation of new guidelines for cystic pancreatic lesions. The aim was to evaluate the outcome of surgery 1997–2009 with histological diagnosis as endpoint.
All patients undergoing laparoscopic pancreatic surgery for cystic pancreatic lesions in the distal pancreas at our tertiary centre between 1997 and 2009 were prospectively included in present study, which was approved by the local ethics committee. Patients with lesions in the pancreatic head were excluded.
Inclusion Criteria
All patients, eligible for the surgical procedure, were considered for inclusion. Indication for surgery was based on a combination radiological findings (computed tomography and magnetic resonance imaging or ultrasonography), patient symptoms and biochemical investigations for hormonally active tumours. A final diagnostic assessment concluded on what was the most likely suspected pathology. If this was a pseudocyst, secondary to pancreatitis, the patient was excluded. When the conclusion was: Most likely a cystic neoplasm in the distal pancreas, the patient was included. The present study was initiated nine years before the Sendai criteria were published [9]. At this time we considered all neoplastic lesions in the distal pancreas (location to the left of the portal vein, i.e. body and/or tail) an indication for surgery.
Based on the combined preoperative radiological and clinical data, the peroperative strategy was chosen according to the following principles: if a lesion was supposed to have a significant malignant potential, distal resection together with splenectomy was preferred. Otherwise, spleen-preserving distal pancreatic resection was chosen [10]. In the case of a small, superficial and tentatively benign lesion, i.e. with significant distance from the main pancreatic duct, enucleation was considered adequate [11]. Radiological diameter <20 mm and distance from the main pancreatic duct >3 mm were criteria for the enucleations.
Surgical Technique
Patients were operated under general anaesthesia, placed in a modified supine position with the left side raised. The first trocar was placed in the umbilicus, one additional 12 mm trocar in the midline between the xiphoid process and the umbilicus and one 12 mm trocar at the level of the umbilicus, pararectally. Occasionally an additional 5 mm trocar was placed subcostally in the medioclavicular line. Two main instruments were used to mobilize the splenic flexure of the colon medially, opening the lesser sac then dissecting the peripancreatic tissue. Also the gastrocolic ligament and the short gastric vessels were divided mobilising the transverse colon. Intraoperative ultrasound was used for exact tumour localisation. In case of spleenpreserving distal pancreatectomy, the splenic vessels were dissected from the pancreas to maintain adequate circulation of the spleen. An EndoGIA® was used to divide the pancreas, and a drain was placed at the resection margin for analysis of amylase in the secreted fluid. The surgical technique has been described in detail earlier [12].
Postoperative complications occurring in-hospital were recorded and retrospectively classified by the Revised Accordion Classification from grade 1 (mild) to 6 (death) [13]. The pancreatic fistula severity grading criteria of the ISGPF was used [14]. These criteria were published after study start, and classification was done retrospectively.
Neoplasms were categorised according to the WHO classification from 2000 [15]. However, the WHO revised its classification in 2010, and now all solid pseudopapillary neoplasms (SPPN) are categorised as low-grade malignancies [16]. Thus, SPPNs originally reported to be benign were recoded into low-grade malignancies.
Lesions were classified according to their pathological diagnosis into two groups: patients with or without malignant potential. For this reason, serous cystic neoplasms (SCN), pseudocysts, retention cysts and lymphoepithelial cysts were classified as neoplasms without malignant potential. Mucinous cystic neoplasms (MCN), SPPNs and intraductal papillary mucinous neoplasm (IPMN) were classified as tumours with malignant potential. Patients with established malignancy were included among the latter.
Statistical analysis was performed using SPSS (IBM SPSS Statistics Version 21 for Windows). Nonparametric statistical tests were used, and variables were compared using the Mann-Whitney test. Statistical significance was set at a p value less than 0.05.
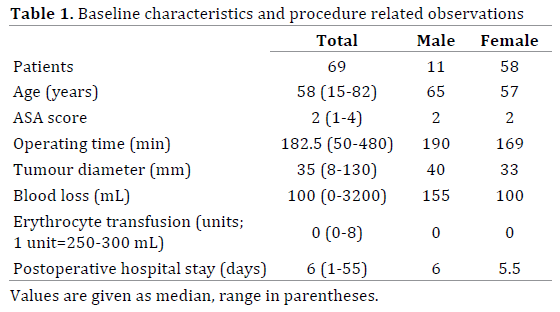
A total of 193 patients underwent resection of the body and/or tail of the pancreas by the laparoscopic approach during the study period. The indication for resection was neoplasm with uncertain malignancy potential, most often a solid tumour. In 69 patients the indication for resection was a cystic neoplastic lesion, which was the inclusion criteria in the present study, as specified above. Baseline characteristics for these 69 patients are shown in Table 1. Sixty-two patients underwent distal pancreatectomies, in whom 19 were spleen-preserving. In seven additional cases enucleations were performed. Overall operating time was median 182.5, range 50-480 minutes. Operating times with and without splenectomy were median 167 and 220 minutes, respectively (P=0.19), and median 127.5 minutes in enucleations.
Histology of the resected specimens is summarized in Table 2. Histopathologically, 57 patients (83%) had benign and 12 patients (17%) had malignant lesions, two invasive IPMNs and ten SPPNs. There were three IPMNs with moderate dysplasia. All 12 MCNs were reported as benign by the pathologists.

When the patients were grouped according to the lesions’ malignant potential, distal laparoscopic resections had been performed in 27 patients (39%) with neoplasms with malignancy or a malignant potential (Figure 1).
In two patients with IPMN the tumour diameter was less than 30 mm, both with moderate dysplasia, i.e. borderline tumours. The diameter of the tumour in the first was 29 mm; this patient had a positive family history of pancreatic cancer. The second had a 15 mm tumour and a two year history of abdominal pain, nausea and weight loss.
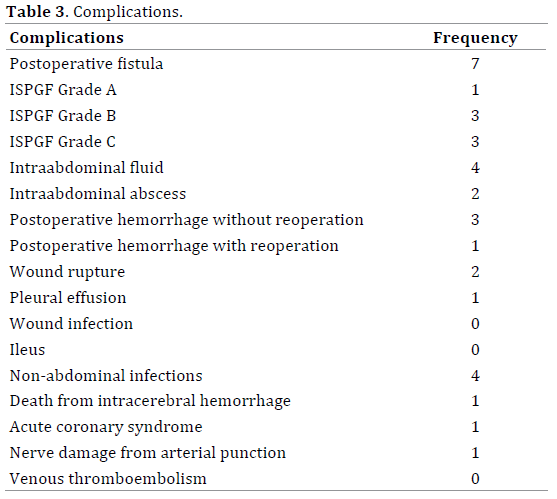
Complications are summarised in Table 3. Twenty-three patients had 27 complications, 15 of these were mild; Accordion Classification grade 1 through 6 were 15, 6, 3, 2, 0 and 1, respectively. Fistulas complicated the postoperative period in seven patients (10%). ISGPF group classification is specified in table 3. Two patients were reoperated for bleeding and wound rupture (at the site of specimen removal), respectively. Two other patients with pseudocysts were converted to a laparotomy, one for the construction of a jejunal anastomosis, the other because of a bleeding that could not be controlled laparoscopically. One patient suffered a cerebral bleeding shortly after a distal pancreatectomy with splenectomy, and died 11 days postoperatively. The complication rate did not differ between patients having lesions with or without a malignant potential (37% vs. 31%, P>0.6). Overall, length of hospital stay was median 6 days (range 1 to 55 days).
In three patients the pathologist reported a positive microscopic margin, one with SCN and two with SPPN. The latter two patients have been subject to follow-up, and there have been no recorded recurrences of the neoplasms with an observation of 9 to 57 months. R0 resection was verified in the remaining patients.
The proportion of patients with malignant or premalignant cystic neoplasms was 39%; 61% had no malignant potential. The majority had SCNs or pseudocysts. These numbers illustrate the final outcome of the present selection criteria, ie, no preoperative endoscopic ultrasound examination and hence no analyses of cyst fluid for CEA and/or amylase. However, the morbidity after laparoscopic surgery on the distal pancreas was low, and the majority of the complications were mild.
In this study the majority of the patients underwent surgery for a benign lesion (83%). There are no previous Scandinavian reports on the results of laparoscopic surgery in cystic pancreatic lesions in this period of time. Our results are comparable to previous studies. In two larger studies by Song and Mabrut the proportion of patients with benign tumours was 75 and 87%, respectively [17, 18].
To avoid surgery in benign cystic lesions, the neoplasms must first be correctly identified. Contrast-enhanced triphasic CT has been the preferred modality both to localize and characterize a cystic lesion, and also because it properly defines the relationship to surrounding organs and identifies metastases. MRI has been considered most suitable to identify mural nodules and cysts communicating with the pancreatic ducts. Due to technological advances, CT now performs similarly [19]. Commonly, studies of cystic lesions are focused on the differentiation between mucinous and nonmucinous, or benign and malignant, analogous to the management algorithms. The accuracy of both CT and MRI has proven suboptimal in this respect [20-25]. Considering our patient cohort, it is of special concern that the sensitivity of CT in diagnosing SCNs has been reported as low as 25% [22, 26]. A central scar is commonly considered diagnostic, but is reported to be present in only 22% of cases [27]. EUS-FNA is now widely available, but whether the added information is of clinical use, is debated. The recently published International guidelines on the management of IPMN and MCN [1] recommends EUS in several clinical scenarios. One of these is the differentiation between an oligocystic SCN and MCN, but only 4 of our patients had an oligocystic SCN. The European guidelines on cystic tumours of the pancreas do not recommend EUS as part of the routine workup, but merely as an option in difficult cases [2]. Low levels of CEA (carcino embryonic antigen) in cyst fluid from SCNs was found by Tatsuta et al. in 1986 [28]. A pooled analysis by van der Waaij et al. demonstrated that a CEA <5 ng/mL suggested a SCN or pseudocyst with a specificity of 95% [29]. The sensitivity for a SCN was 75%. These findings suggest that many of the SCNs in our study cohort could have been diagnosed by EUS-FNA.
Overall morbidity in our study was 33%, and fistula rate was 10%. The literature on laparoscopic distal pancreatectomy for the subgroup of cystic lesions is limited [30]. The previously reported fistula rates in similar studies have ranged from 8 to 50%[ 10, 31]. Contrary to our findings, a higher proportion of grade A fistulas would be expected [17]. Mortality in laparoscopic distal pancreatectomy is low. When summarizing the data from similar studies (including more than 50 patients), there were 3 reported deaths in 950 patients (0.3%) who underwent laparoscopic distal pancreatic resections [17, 18, 32-36]. The occurrence of a postoperative cerebral haemorrhage in one patient is not specifically attributable to laparoscopic pancreatic surgery, but nonetheless highlights the overall risk of surgery and the principle that patient selection is essential in surgical practice in general.
In recent reports the most prevalent cystic neoplasm of the pancreas has been IPMN [17, 37, 38], but only 4 patients had this neoplasm in the present cohort. SCN was the predominant neoplasm (42%). A higher prevalence of SCN in the Western than the Eastern hemisphere has been suggested [39]. Resection of SCN is today restricted to patients with symptoms, which is correlated with size. Two studies have demonstrated that when tumour diameter exceeds 40 mm, SCNs are frequently symptomatic [40, 41]. In the present study, 19 of the 29 SCNs had a diameter less than 40 mm. We conclude that surgery most likely was avoidable in the majority of these patients.
Gaujoux et al. compared the management of patients with cystic lesions of the pancreas in two sequential time periods (1995-2005 and 2005-2010), and found significant differences[38]. The handling of the cystic lesions changed significantly between these two periods. During the first time period 43% of the patients underwent initial resection, decreasing to 33% in the second. Furthermore, the rate of resected SCNs decreased from 34% to 13%. The authors interpreted this as a result of an increased ability to identify lesions radiographically, the use of EUS-FNA with cyst fluid analysis of CEA and a general acknowledgement that serous lesions are benign.
In our study 11 patients had pseudocysts. The patients were included because there was an explicit suspicion of a cystic neoplasm after preoperative work-up. EUS with FNA might have changed the management of these patients, but there are no adequate cyst fluid markers to make a certain diagnosis of a pseudocyst [42]. Publications on radiology have frequently been biased by the exclusion of pseudocysts.
Only patients accepted for surgery were included in the database. Some lesions were both cystic and solid in appearance, and were mainly excluded from this study (and regarded as solid).
In some of these the cystic component was the dominant feature and histology revealed ductal adenocarcinomas, a constellation that should always be considered in cystic lesions of the pancreas [43].
The approach described in this paper means no followup group including the risk for developing cancer. We even must take into account what it means for the single patient to be in a follow-up group (QoL), even if the risk for developing cancer is very low. Based on improved technology and better knowledge of preoperative diagnostics, it is even important to evaluate the current approach based on existing guidelines.
In conclusion, most postoperative complications were mild after laparoscopic distal resection of cystic pancreatic lesions, but this fact does not justify the present high proportion of patients with benign lesions (61%). The death of one patient after postoperative intracerebral hemorrhage underlines that improved preoperative patient selection is mandatory. Endoscopic ultrasound examination (EUS), enabling aspiration of cyst fluid and fine needle aspiration (FNA) is an additional option for the preoperative workup.
The authors had no conflicts of interest