Review Article - (2017) Volume 18, Issue 2
Gastroenterology, Hepatology, and Nutrition, Virginia Commonwealth University, Richmond, VA, 23298, USA
Received December 2nd, 2016 - Accepted February 08th, 2017
Pancreas divisum, the failure of fusion of the dorsal and ventral pancreatic ductal systems in utero, is the most common congenital abnormality of the pancreas. The clinical significance of pancreas divisum is often considered when it is found in patients with idiopathic acute or recurrent pancreatitis. With increasing use of magnetic resonance imaging and magnetic resonance cholangiopancreatography in the past twenty years, the detection of pancreas divisum is increasingly common in patients undergoing cross-sectional imaging. Therapeutic interventions for patients with recurrent acute pancreatitis and pancreas divisum aim to relieve the relative obstructive pancreatopathy caused by a stenotic minor papilla. Developments in the study of the genetics of pancreatitis have fueled the debate as to whether pancreas divisum in itself causes pancreatitis. Some have argued that pancreas divisum is a bystander and that its role as an etiology of recurrent acute pancreatitis should be abandoned. Others have suggested that further study is needed in the understanding of the association of pancreas divisum with genetic mutations, such as cystic fibrosis transmembrane conductance regulator. Historically, the study of pancreas divisum has been limited to uncontrolled and observational studies with the level of evidence reviewed. This paper will review the anatomy, diagnostic and therapeutic modalities, and developments in the genetics of pancreas divisum to revive the discussion on this much-debated topic.
Gene Expression; Immunotherapy; Pancreatic Neoplasms
CFTR cystic fibrosis transmembrane conductance regulator; MRI magnetic resonance imaging; RAP recurrent acute pancreatitis; s-MRCP secretin enhanced magnetic resonance cholangiopancreatography
Pancreas divisum is the most common congenital anatomic abnormality of the pancreas. During the sixth week of gestation, the pancreas normally develops from the fusion of the dorsal and ventral pancreatic buds. The dorsal bud forms the head, body, and tail while the ventral bud develops into the uncinate process. In the majority of individuals, the union of these structures allows for a fusion of their ductal systems such that the main pancreatic duct serves as the path for emptying of pancreatic secretions into the duodenum via the major duodenal papilla. A normal variant anatomy is present in approximately 30% of individuals, where the proximal dorsal pancreatic duct persists as an accessory pancreatic duct and empties via the minor duodenal papilla [1]. On the contrary, in typical Pancreas divisum, the fusion of the dorsal and ventral ductal systems fails, forming two distinct conduits with the dorsal duct draining the majority of the pancreas via the minor papilla and the ventral duct draining only the inferior portion of the head of the pancreas via the major papilla [2]. The normal anatomy of the pancreas as well as anatomic variant findings in pancreas divisum is illustrated in Figure 1. Another anatomic variant, incomplete pancreas divisum, is infrequent, and presents as a narrow and often inadequate connection between the dorsal and ventral pancreatic ducts, with the majority of drainage occurring via the smaller minor papilla [3]. Autopsy series have reported the incidence of pancreas divisum to be in the order of 5-10% of the general population [4, 5]. Although pancreas divisum is a congenital anomaly present at birth, it is often not diagnosed until the fifth decade of life, when it becomes symptomatic [6, 7]. With increasing use of cross-sectional diagnostic imaging, pancreas divisum is being diagnosed earlier in asymptomatic patients.
The clinical significance of pancreas divisum is often considered when it is found in patients with idiopathic acute or recurrent pancreatitis. Cotton [6] first suggested a correlation between pancreas divisum and development of pancreatitis in a retrospective series of patients undergoing endoscopic retrograde cholangiopancreatography (ERCP). While the overall incidence of pancreas divisum was 3.6% in the series, patients with unexplained recurrent pancreatitis had a much higher incidence of 25.6%. Although this study was weakened by a referral bias and did not consider alternative etiologies for pancreatitis, such as genetic or autoimmune causes, it did lead to further interest in a potential role of pancreas divisum in the development of acute and recurrent pancreatitis. The proposed mechanism for pancreatitis in pancreas divisum is an obstructive pancreatopathy, with the narrow minor papilla bearing the responsibility for draining the majority of the pancreas by way of the dorsal pancreatic duct [6, 8].
In an attempt to quantify this, Staritz et al. [9] performed ERCP with manometry on patients with pancreas divisum and found relatively increased pressures in the dorsal duct as compared to the ventral duct. However, the evidence is equivocal: Satterfield et al. [10] found no difference in both basal and phasic manometric pressures from the major and minor papilla in patients with pancreas divisum and acute pancreatitis. From an anatomic standpoint, Wang et al. [11] used magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) to support the dorsal obstructive hypothesis by showing that isolated dorsal pancreatic involvement was more common in patients with pancreatitis and pancreas divisum, 44.74% as compared to 22.22% in controls, with pancreatitis but without pancreas divisum.
With increasing use of MRI and MRCP in the past twenty years, the detection of pancreas divisum is increasingly common in patients undergoing cross-sectional imaging. MRCP has been shown to have the same diagnostic accuracy in the diagnosis of pancreas divisum as ERCP [12]. Furthermore, secretin-enhanced MRCP (S-MRCP) may enhance detection of pancreas divisum by stimulating bicarbonate and fluid secretion into the pancreatic ducts, allowing for improved visualization of anatomic features [13]. A meta-analysis of 10 studies with 1474 patients showed that secretin-enhanced MRCP had increased diagnostic performance with sensitivity of 86% as compared to 52% for standard MRCP, thus strengthening the role of non-invasive imaging for the diagnosis of pancreas divisum [14]. With increased access to radiology facilities with MRI/MRCP capabilities, these imaging modalities will continue to serve as the new standard in diagnosis of pancreas divisum.
Therapeutic Interventions
Therapeutic interventions for patients with recurrent acute pancreatitis (RAP) and pancreas divisum aim to relieve the relative obstructive pancreatopathy caused by a stenotic minor papilla. While surgical intervention such as minor papilla sphincteroplasty has been performed with some success [15, 16, 17], endoscopic therapy is favored as a less invasive treatment modality. Endotherapy for pancreas divisum may include dorsal duct pancreatic stent placement [18] or, more frequently, endoscopic minor papillotomy [19]. In a randomized controlled trial, patients with pancreas divisum were randomized to either dorsal duct stent placement (in 10 patients) or no intervention in controls (9 patients). With a mean followup of about 30 months, no patients in the stent group required hospitalization for abdominal pain but five out of the nine patients in the control group were readmitted for pain management. RAP was documented in one of the ten stented patients and seven of the nine control patients [20]. In a long-term efficacy study endoscopic therapy, twentyfour patients with RAP and underlying pancreas divisum were treated with sphincterotomy of the minor papilla (8 patients) or dorsal duct stent insertion (16 patients). Acute pancreatitis recurred in two of the eight patients treated with sphincterotomy of the minor papilla and there was no recurrence in patients that received a stent with a median duration of follow-up of 39 months. On the other hand, complication rate was less significant in the minor papillotomy group (25%) as compared to the dorsal duct stent group (44%) [21]. These endoscopic therapies have shown clinical benefits in patients with RAP associated with pancreas divisum, while patients with chronic pancreatitis associated with pancreas divisum, or abdominal pain without pancreatitis, may not be ideal candidates for these interventions [22, 23, 24]. Additionally, endotherapy in patients with RAP due to Pancreas divisum has been shown to decrease interval endosonographic findings of chronic pancreatitis, suggesting that earlier therapy may be warranted in these patients [25]. However, while the typical rate of post-ERCP pancreatitis is estimated at 3.5% [26], this risk is increased to as high as 10.6% with dorsal duct cannulation and minor sphincter papillotomy [27]. Therefore, the benefits must be weighed against the risks of endotherapy, with particular consideration to the added risk of post-ERCP pancreatitis with endoscopic minor papillotomy.
Is Endotherapy Alone the Answer?
Although patients with RAP and pancreas divisum undoubtedly benefit from minor papillotomy, there is ongoing debate about the true cause of the pancreatitis: is it the anatomy alone, or are other comorbidities responsible? Spicak et al. [28] used MRCP and ERCP to study the impact of pancreas divisum on the natural course of chronic pancreatitis. They found that pancreas divisum did not modify the age of onset of CP, and, despite the presence of pancreas divisum, a majority of their patients still had abnormalities of the ventral duct (75% in patients with, and 72% in patients without, a history of alcohol abuse), with a low frequency having dorsal duct involvement (25% and 28%, respectively). With these findings, the investigators theorized that pancreas divisum in itself does not modify the natural course of chronic pancreatitis.
Genetic Mutations
This argument was further advanced by the observation that genetic mutations associated with pancreatitis may be seen in higher frequencies in patients with pancreas divisum. Pramod et al. [29] found SPINK-1 mutations were more common in patients with pancreas divisum with RAP (41.6%) as compared to healthy controls without pancreas divisum (2%). The mutation was present in similar frequency in patients without pancreas divisum who had idiopathic chronic pancreatitis (43.3%) and idiopathic RAP (35.7%) suggesting that in this population, SPINK-1 mutation and not pancreas divisum may be a common factor leading to development of pancreatitis.
Anomalies of the CFTR gene have also been associated with development of pancreatitis in patients with pancreas divisum. Dray et al. [30] reported two cases of young female patients with pancreas divisum and RAP who were found to have a mildly abnormal CFTR genotype (IVS8- 5T-TG12) which led to RAP with only mild upper airway manifestations. They theorized that the mild CFTR protein dysfunction and resulting impaired epithelial ion transport results in abnormal pancreatic fluid secretion, leading to RAP in pancreas divisum. Gerlud et al. [31] showed that patients with pancreas divisum and RAP had a decrease in CFTR function intermediate between patients with cystic fibrosis and healthy controls. They hypothesized that in addition to increased viscosity of pancreatic fluid, CFTR dysfunction may also cause an excessive host inflammatory response that may further narrow the already smaller pancreatic duct orifice in pancreas divisum, predisposing patients to pancreatitis. In a recent MRCP study, Bertin et al. [32] enrolled consecutive patients with acute recurrent and chronic pancreatitis and found that the frequency of pancreas divisum was greater in patients with CFTR associated pancreatitis (47%), as compared to healthy controls (7%) and alcohol-induced pancreatitis (7%). With these findings, the investigators suggested CFTR mutations or other polymorphisms in patients with pancreas divisum might explain why only a subset of patients with this disorder develops pancreatitis. On the other hand, in their editorial for the Bertin et al. study, DiMagno and DiMagno [33] caution that ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¦Ã¢â¬Åcorrelation does not equal causationÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâàand suggest that CFTR mutations and pancreas divisum may co-exist without influencing genetic susceptibility to pancreatitis. Recently, Ballard et al. [34] found that in individuals with adult-onset pancreatic disease, the discovery of high risk mutations may be facilitated with using complete gene sequencing. Further study into the association of CFTR mutation and pancreas divisum, perhaps using complete gene sequencing, will be needed to settle this debate.
Summary
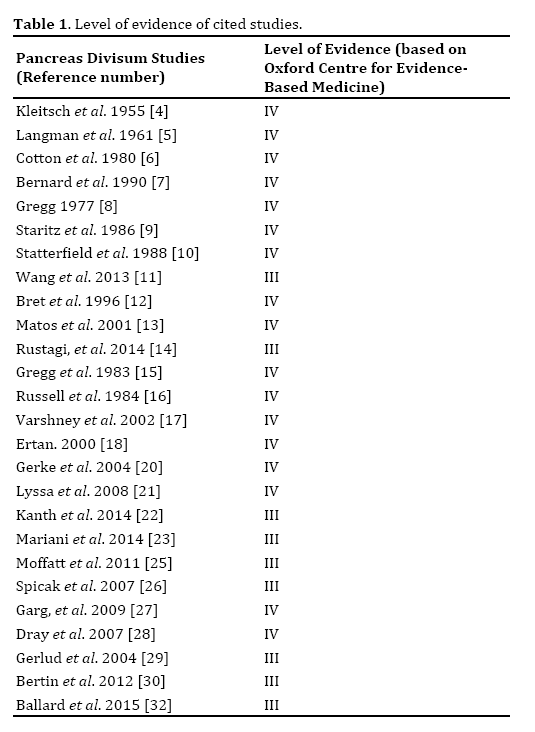
Although pancreas divisum has been an anatomic finding described in the literature for since the 19th century, the debate as to whether it causes pancreatitis, or is simply a bystander, lives on to this day. Historically, the study of pancreas divisum has been limited to uncontrolled and observational studies as evidenced in this paper (Table 1). Clinicians should be aware of this entity: given the prevalence of close to 10% in the general population, with the increasing use of cross-sectional imaging it will become a more common incidental finding. When encountered in a patient with idiopathic RAP, genetic testing should be considered. Research into the outcomes of minor papilla endotherapy in the subset of patients with pancreas divisum and genetic anomalies, such as CFTR mutation, should be pursued in the future.
Conflict of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.