- (2009) Volume 10, Issue 4
Jai Dev Wig, Ashwinikumar Kudari, Thakur Deen Yadav, Rudra Prasad Doley, Kishore Gurumoorthy Subramanya Bharathy, Naveen Kalra
Department of General Surgery, Postgraduate Institute of Medical Education and Research. Chandigarh, India
Received April 5th, 2009 - Accepted May 14th, 2009
Context To assess the feasibility and safety of a pancreas-preserving total duodenectomy in the management of severe duodenal injury caused by abdominal trauma. Case report Two patients with both extensive injury of the duodenum and diffuse peritonitis underwent pancreas preserving total duodenectomy at our tertiary care centre. These two young male patients (age 20 and 22 years) presented 2 days and 6 hours respectively following blunt abdominal trauma. The duodenum was almost completely separated from the pancreas. Ampulla was seen as a button on the pancreas. Following total duodenectomy, reconstruction was performed by suturing the jejunum to the head of the pancreas anteriorly and posteriorly away from the ampulla (invagination of the pancreas into the jejunum). There were no complications attributable to the procedure. Both patients are well on follow up. Conclusion A Pancreas-preserving total duodenectomy offers a safe alternative to the Whipple procedure in managing complex duodenal injury. This procedure avoids unnecessary resection of the adjacent pancreas and anastomosis to undilated hepatic and pancreatic ducts.
Abdominal Injuries; Duodenum; Wounds and Injuries
Abbreviations PD: pancreaticoduodenectomy; PJ: pancreaticojejunostomy; PPTD: pancreas preserving total duodenectomy
Severe duodenal injury is rare and remains a challenging problem [1, 2, 3, 4, 5]. The major concern is failure of the repair with resultant abdominal septic complications and fistula formation [2, 3, 4]. Complex enteric reconstruction and drainage procedures [5] have been employed for extensive damage to the duodenum: duodenal diverticulization [6], pyloric exclusion [7, 8], duodenal resection and anastomosis (duodenoduodenostomy, duodenojejunostomy) [9], ampullojejunostomy [10], duct reimplantation [11], pancreaticoduodenectomy [12, 13], pancreas preserving total duodenectomy [14, 15, 16] and bioprosthetic repair of enteric wall defects [5] Successful management depends on an appropriately selected procedure. Duodenum related morbidity ranges from 12% to 63% and the mortality rates range from 6% to 29% [1]. This paper reports our experience with pancreas-preserving total duodenectomy (PPTD) for complex duodenal injury.
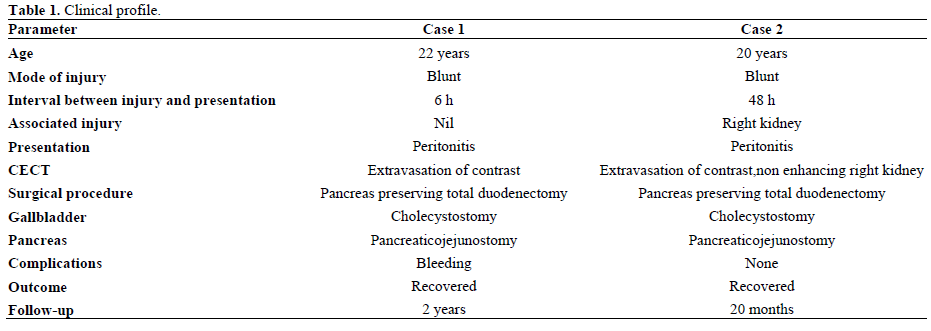
The details of two patients are presented in Table 1. Both patients had diffuse peritonitis. Contrast enhanced computed tomography (CECT) revealed pneumoperitoneum and extravasation of contrast from the duodenum (Figure 1). In one patient (Case 2), CECT revealed a non-enhancing right kidney.
At laparotomy, there was complete disruption of the duodenum (Figure 2). The ampulla was visible as a button on the pancreatic head .The duodenum was completely mobilized and carefully separated from the pancreas. Bleeding from the pancreatic surface was carefully secured. The viability of the ampulla was not in doubt. Reconstruction was achieved by end-to-side invagination pancreaticojejunostomy without duct to mucosa suturing of ampulla. The jejunum was fixed to the intact head of the pancreas anteriorly and posteriorly by interrupted nonabsorbable sutures beyond the ampulla. The head of the pancreas and the ampulla rested neatly within the jejunal C and this made the pancreaticojejunostomy easy to perform. Gastrointestinal continuity was restored by end-to-side gastrojejunostomy. Biliary decompression was achieved through a cholecystostomy. A feeding jejunostomy tube was placed distal to the gastrojejunostomy to decompress the pancreatico jejunostomy (Figure 3). A 16F portex tube drain was placed adjacent to the pancreatic-enteric anastomosis. In one patient (Case 2), a right nephrectomy was also performed as renal vessels were thrombosed.
One patient (Case 1) was re-explored 36 hours later for bleeding from the drain placed near the pancreas. There was diffuse ooze from the retroperitoneum. The anastomoses were intact.
Jejunostomy tube feeding was started after 5 days. An upper gastrointestinal gastrografin study ten days later revealed no anastomotic leak and the patients were then put on oral feeding.
A tube cholecystogram carried out 3 weeks later revealed a normal common bile duct and free flow of contrast into the jejunum (Figure 4). The Cholecystostomy tube was subsequently removed. The patients are well at the two-year follow-up with no symptoms; liver function tests are normal
The surgical management of duodenal injury is complex and options vary from external drainage to complex reconstruction procedures to pancreaticoduodenectomy. Each of these procedures has its own limitations. Primary repair is associated with high duodenum related morbidity [1]. Duodenal fistula rates range from 0 to 16.2% [17, 18], and the mortality rate ranges from 10% to 29% [2, 18]. The role of pyloric exclusion is controversial [1, 2, 7, 8]. Recent studies found no difference in morbidity or mortality rates in patients undergoing pyloric exclusion versus primary repair [8, 19]. Dubose et al. [4] (results from the National Trauma Data Bank) reported no statistically significant difference in mortality or occurrence of abdominal septic complications in those undergoing pyloric exclusion versus primary repair. They further reported that pyloric exclusion contributes to longer hospital stays and confers no survival or outcome benefit. Pancreaticoduodenectomy (PD) for trauma is a formidable procedure with the attendant risks of anastomosis to the undilated bile and pancreatic ducts and soft pancreas [13, 19].
PPTD has been introduced as an alternative to PD for familial adenomatous polyposis, benign villous tumours of the duodenum and isolated duodenal injury [14, 15, 16, 20, 21]. PPTD was introduced as an alternative to PD on the basis of lower morbidity and mortality rates [16]. In a study comparing PPTD with classical PD for patients with familial adenomatous polyposis, no clear advantage was reported as PPTD was not associated with lower morbidity and mortality rates [20]. Another recent study reported that the morbidity of PPTD is similar to PD, but PPTD preserves the whole pancreas and reduces the number of anastomoses [21]. Muller et al. [22] have reported that PPTD is a safe surgical procedure which avoids pancreatic head resection, and shows advantages over the pylorus preserving Whipple procedure. They reported a hospital mortality of 4.3% and a 30% morbidity rate after PPTD.
PPTD is a relatively new procedure for complex traumatic injury of the duodenum. Advantages of PPTD over classical PD include preservation of the entire pancreas and avoidance of anastomoses to undilated biliary and pancreatic ducts and the cut surface of a soft pancreas. Anastomosis in unfavorable situations is associated with a high risk of anastomotic leakage [23].Various methods of reconstruction following PPTD include anastomosis between the papilla and the small bowel, sphincteropapillotomy and an opened major papilla anastomosed to an opening in the small intestine [15] and no pancreatic enteric anastomosis [24]. We used the dunking procedure: the head of the pancreas was fixed with the jejunum by interrupted nonabsorbable sutures. The entire common bile duct and pancreatic duct were preserved. In the two patients reported, no morbidity resulted from PPTD.
Biliary diversion is a useful addition for the management of duodenal injuries [25]. Decompression via a quadruple tube technique to protect the duodenal repair is reported to reduce the risk of duodenal fistula [26]. Biliary diversion, in our study, was possibly helpful in protecting the pancreaticojejunostomy (PJ) in the immediate postoperative period by reducing the amount of bile entering the jejunum. A cholecystocholangiogram revealed adequate biliary drainage. Both patients are well on follow-up.
The role of prophylactic octreotide administration remains controversial. Though there are reports suggesting the use of prophylactic octreotide in pancreaticoduodenal injuries [27, 28], most of the studies have not mentioned its use in duodenal injuries [1, 3, 15, 19]. Moreover, the selective use of octreotide to prevent postoperative complications and mortality in patients undergoing pancreatic surgery also remains debatable [29, 30].
The ampulla was preserved in both of our patients and we did not institute external drainage of pancreatic duct with a stent. The use of a pancreatic duct stent for the drainage of pancreatic duct though an attractive strategy remains debatable: some report a reduced leakage rate [31], while others have not found it effective in significantly reducing the leak rate [32, 33].
The present report demonstrates the usefulness of PPTD for complex duodenal injury. PPTD is an organ preserving and problem-focused technique which avoids the hazards of anastomosing undilated bile and pancreatic ducts. The duodenum is removed and the entire pancreas is preserved. PPTD thus is a protective strategy which provides adequate treatment for complex duodenal injury and prevents duodenum and pancreas related morbidity.
Conflict of interest The authors have no potential conflict of interest