- (2004) Volume 5, Issue 5
Paolo Soliani1, Christian Franzini1, Stefanie Ziegler1, Paolo Del Rio1, Paolo Dell’Abate1, Davide Piccolo1, Gioacchino Giovanni Japichino1, Giulia Martina Cavestro2, Francesco Di Mario2, Mario Sianesi1
1Department of General Surgery and Organ Transplantation and 2Department of Clinical Sciences, Section of Gastroenterology, University of Parma. Parma, Italy
Received: 13 May 2004 Accepted: 26 May 2004
Context The natural history of pancreatic pseudocysts has become well known in recent years, but the choice of a proper treatment still remains controversial. Objective This study aims at establishing whether predictive factors influencing therapeutic outcomes exist. Setting Patients with pancreatic pseudocysts following an episode of acute pancreatitis treated from January 1980 to December 2001 at the Department of General Surgery and Organ Transplantation of the University of Parma, Italy. Patients :Seventy-four patients were studied: 12 had a spontaneous resolution, 37 patients were treated surgically, 15 were treated endoscopically and in 10, percutaneous drainage was used. Main outcome measures Epidemiological, clinical and pathological characteristics of patients with pancreatic pseudocysts were related to morbidity, recurrence rates and hospital stay. Results At univariate logistic regression, our data reveal a significant increase in morbidity related to age (P=0.013), etiology (alcoholic vs. biliary, P=0.024), Ranson score of previous pancreatitis (P=0.006), nutritional assessment (P=0.001), residual necrosis (P0.001) and modality of treatment (P=0.009), whereas none of these parameters has been shown to be significantly correlated to recurrence. At multivariate logistic regresion, only residual necrosis was significantly related to morbidity. Conclusions Some factors, such as epidemiological (age, etiology), clinical (severity of previous pancreatitis, malnourishment), pathological (residual necrosis), and therapeutical actors (emergency/urgency treatment) are predictive of worse outcomes for invasive treatment of pseudocysts. In particular residual necrosis appeared to be the most important factor influencing invasive treatment outcomes, confirming that this pathological aspect deserves particular attention from surgeons. No risk factors predicting pancreatic pseudocyst recurrence emerged.
Pancreatic pseudocysts (PPs) are a common complication of acute pancreatitis [1, 2, 3, 4, 5]; they occur as a consequence of an acute inflammatory attack in normal pancreatic tissue or in chronic pancreatitis [6, 7]. PP can resolve spontaneously or can cause symptoms and complications so that invasive treatment becomes necessary [8, 9, 10, 11, 12, 13, 14, 15]. Our knowledge about the natural history of PP has increased in recent decades, thanks to the improvement of imaging techniques [1, 3, 5, 6, 16, 17, 18]. Pseudocysts, which occur after acute pancreatitis, have a different course as compared to those appearing after chronic pancreatitis so that a distinct treatment is also needed [6, 19, 20]. The situation is somewhat confusing and some attempts have been made to made it clear by classifying PPs according to the pathological changes and duct abnormalities underlying acute or chronic processes [21, 22]. The absence of nosological distinction in most papers leads to a comparison between heterogeneous groups; thus, it is difficult to find consensus for a generally accepted clinical treatment. Moreover, only few data exist concerning the evaluation of specific risk factors influencing the outcome of treatment [8, 23, 24, 25, 26]. The aim of our study was to establish a possible correlation between epidemiological (sex, age), clinical (etiology, prognostic signs of pancreatitis, hospital stay after therapy for PPs, nutritional status, modality and type of invasive treatment), morphological characteristics (dimension of the PPs, localization, number, presence of residual endoluminal necrosis) and the onset of treatment complications or death. Only life-threatening complications, such as sepsis, hemorrhage or leakage, were taken into consideration but not minor morbidity (wound infection, urinary tract infection, etc.). Furthermore, we investigated whether predictive factors of recurrence exist, in order to accurately select these patients for a more intensive follow-up.
Patients
Seventy-four patients with PPs following an episode of acute pancreatitis were treated at the Department of General Surgery and Organ Transplantation of the University of Parma from January 1980 to December 2001. Only necrotic pseudocysts due to an attack of acute pancreatitis were chosen to have a homogeneous and comparable population of patients since “retentional pseudocysts” occurring in chronic pancreatitis are considered to have a different behavior. A distinction between acute and chronic pancreatitis was initially unclear only in alcoholic subjects who required further investigation with ERCP or nuclear MR. As defined in the Atlanta Consensus Conference, only mature cysts of more than 6 weeks duration after the onset of acute pancreatitis were considered. The average age was 55.1±9.5 years (range 33-79 years) and there were more male (n=50, 67.6%) than female (n=24, 32.4%) patients, the ratio being 2.1:1. The patients’ nutritional status was evaluated using anthropometric parameters (Quetelet's index: weight/height2; it was dichotomized according to a cut-off value of 20 kg/m2) and nutritional values indicating malnourishment (albumin less than 3 g/dL; thyroxin binding pre-albumin (TBPA) less than 24 mg/dL; transferrin less than 25 g/dL). Malnourishment was defined as the presence of all four of these conditions and was present in 19 (25.7%) patients. These criteria were chosen on the basis of our previous experience [27].
Most of the preceding pancreatitis cases were of biliary (n=52, 70.3%) or of alcoholic (n=18, 24.3%) nature, whereas a few of them were traumatic (n=2, 2.7%) and one (1.4%) was of iatrogenic origin; in one case (1.4%), the pancreatic etiology remained unknown (Figure 1). The mean size of the PPs, determined by US or CT measurement, was 11.6±5.2 cm (range 2.5-22.8 cm), and more than half of them (n=44, 59.5%) were “giant” (equal to or greater than 10 cm). Most of the PPs were located in the body-tail of the pancreas (n=53; 71.6%) and were single (n=57; 77.0%).
Fifteen patients (20.3%) had complicated PPs at admission: 6 with infection, 4 with jaundice, 2 with abscesses, 2 with intracystic hemorrhage, 3 with gastro-intestinal bleeding and 2 patients with splenic vein thrombosis. The mean Ranson score was 3.1±1.4 (range 1- 7).
All patients underwent medical therapy consisting of fluids, antibiotics and nothing by mouth for at least 8 to 10 days. Twelve patients (16.2%) were treated conservatively with medical therapy alone, whereas the remaining 62 (83.8%) were managed with invasive treatment. Indications for invasive treatment included persisting symptoms (such as pain and fever), hyperamylasemia, elevated white blood cells or complications (such as intracystic hemorrhage, jaundice and infection of the cysts) and PPs which did not resolve during an observation period of 8-10 weeks (beyond which spontaneous resolution was unlikely). Thirty-seven of the 62 patients managed with invasive treatment (59.7%) underwent a surgical approach; in most of the cases (35/37; 94.6%) internal derivation was performed (12 cystogastrostomies and 23 cystojejunostomies), whereas, in the remaining 2 patients (5.4%), a distal pancreatic resection was carried out. Endoscopic cystogastrostomy was carried-out in 15 (24.2%) patients; finally, 10 patients (16.1%) underwent cyst discharge through a CT-guided percutaneous drainage of the PP. The choice of invasive treatment was made in a non-randomized fashion by the managing surgeon. Most of the 62 invasive treatments took place in elective conditions (n=48, 77.4%) after a complete evaluation of the general status of the patient and the morphotopographic features of the PP. All 15 patients who had a complicated PP at admission (9 of whom came from other institutions) underwent invasive treatment immediately (emergency) or within 48 hours (urgency).
Morbidity, mortality, and recurrence rates were reported. Morbidity and recurrence rates were compared using some parameters which, according to most authors, seem to be of high prognostic value (age, gender, etiology and severity of previous acute pancreatitis, nutritional assessment, dimension, location and number of PPs, presence of residual necrosis, modality of treatment). Moreover, the various invasive treatments (percutaneous drainage, surgery, endoscopy) were compared to each other to establish efficiency, safety (morbidity and percentage of recurrence) and costs (mean hospital stay).
ETHICS
Our study was retrospective and the data were obtained from the clinical archives. Therefore, no institutional review committee was consulted
Continuous data are expressed as mean, standard deviation (SD) and range. Absolute and relative frequencies are reported for categorical variables. The hospital stay was log-transformed before analysis (Kolmogorov-Smirnov test for normal distribution: P<0.001 and P=0.135 before and after transformation, respectively). Simple contrast one-way ANOVA as well as univariate and stepwise multivariate logistic regression were applied.
A commercial statistical software kit (SPSS for Windows version 8.0, Chicago, IL, USA) was used for data analysis. Two-tailed P values of less than 0.05 were considered statistically significant.
In our study, the overall morbidity rate was 16.2% (12 cases: 4 fistulas, 2 hemorrhages, 6 abscesses) and the overall recurrence rate was 8.1% (6 cases). We observed 2 deaths (2.7%) and both of these patients had abscesses.
The evaluation of possible predictive factors influencing treatment outcomes is summarized in Table 1. The comparison between patients who achieved therapeutic success and those who showed major complications (life threatening: infection/sepsis, hemorrhage, leaks) or died reveals a significant rise in morbidity and mortality rates related to some parameters such as age (P=0.013), Ranson score (P=0.006; OR=1.79, 95% CI: 1.18-2.71), etiology of previous pancreatitis (P=0.024; alcoholic vs. biliary, OR=4.70, 95% CI: 1.22- 18.0), malnourishment (P=0.001; OR=9.27, 95% CI: 2.37-36.3), residual necrosis (P<0.001; OR=39.3, 95% CI: 7.41-209) and emergency/urgency treatment (P=0.006; OR=6.75, 95% CI: 1.74-26.1. Multivariate logistic regression showed that residual necrosis only entered the procedure, suggesting that residual necrosis is the main independent risk factor for morbidity.
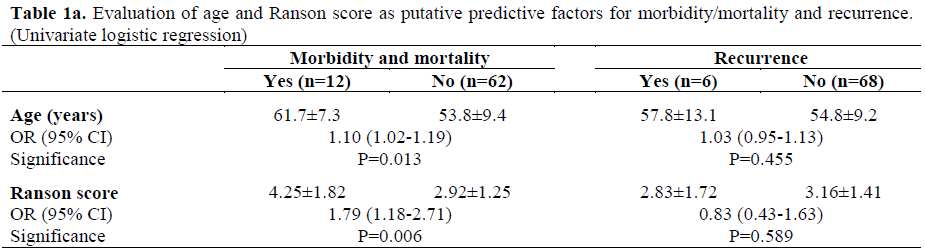
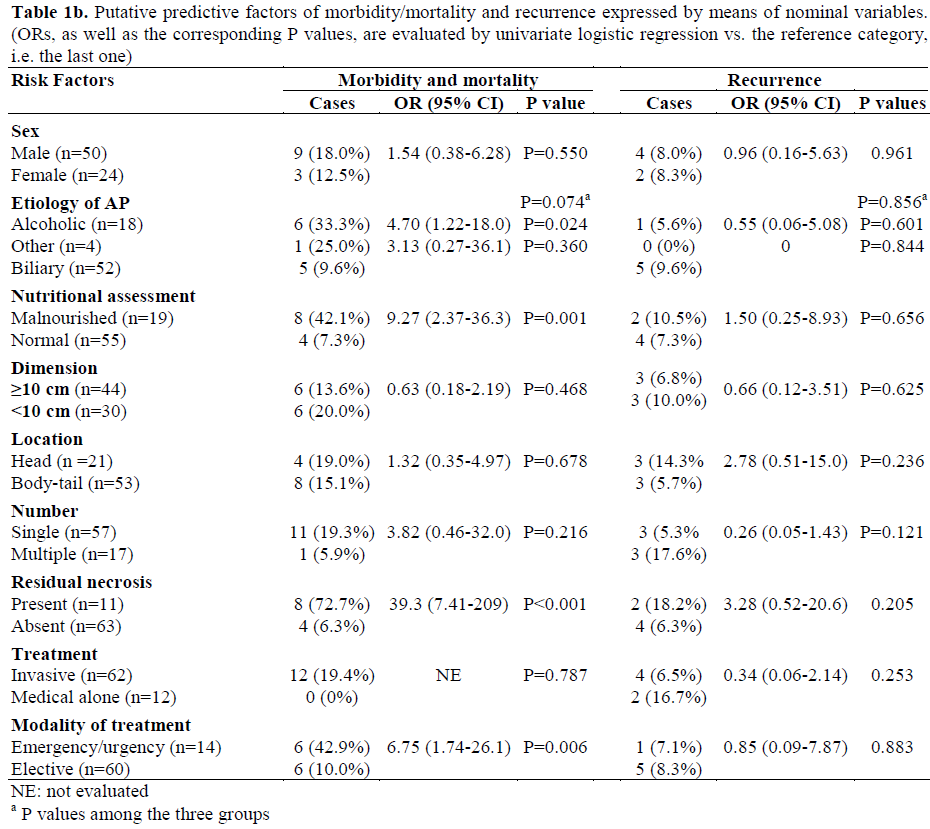
On the other hand, none of these parameters appear to be correlated to a higher recurrence rate (Table 1). It should be pointed-out that 12 patients were conservatively treated with medical therapy alone without any complications and 2 of them developed a recurrence, but, because of the small size of the cyst (4.5 and 4.8 cm) and the lack of symptoms, they did not require invasive management.
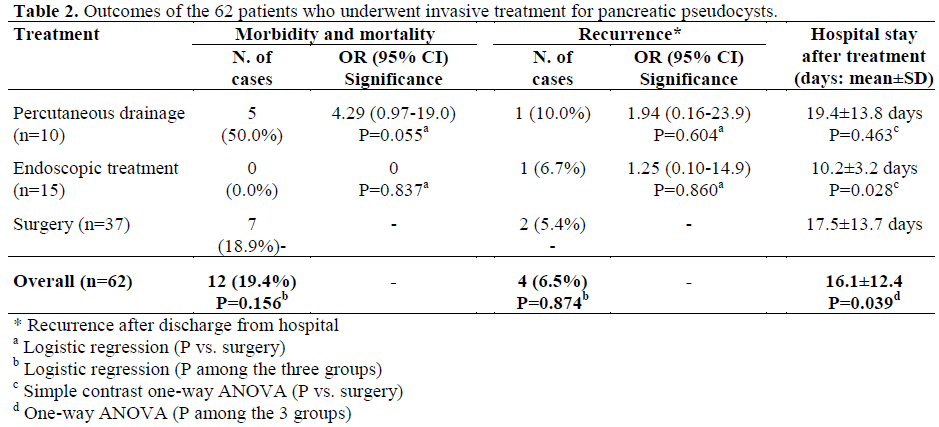
As far as invasive treatment is concerned, the small number of complications does not allow us to make a reliable comparison between the predictive factors of morbidity and each invasive treatment. However, taking into consideration the complication as a whole (Table 2), surgical treatment led to postoperative complications in 7 cases (18.9%): 4 bleeding, 2 pancreatic leakage and 1 infection. Two patients developed a new PP (recurrence rate: 5.4%) and no death occurred in this group. In these patients, the mean hospital stay was 17.5±13.7 days. Five out of 10 patients (50.0%) treated with percutaneous drainage had complications (2 leakages, 2 infections and 1 hemorrhage) showing a tendency to a higher morbidity vs. surgery (P=0.055; OR=4.29, 95% CI: 0.97-19.0). One of these patients (10.0%) had recurrence. We point out that, in this group, we observed two deaths due to sepsis (20.0%). The mean hospital stay of patients who underwent percutaneous drainage was 19.4±13.8 days. No significant difference in recurrence and hospital stay were observed between these patients and those who underwent surgery. Endoscopic treatment was performed with the procedure of cyst-gastrostomy in giant PPs presenting endoluminal gastric bulging. No complications and no death occurred. In one case, a stent obstruction caused a recurrence treated endoscopically with substitution of the drainage. The mean hospital stay of patients who were treated endoscopically treated was significantly shorter than those who were treated surgically (10.2±3.2 days; P=0.028). Invasive treatments as a whole required a mean hospital stay of 16.1±12.4 days.
Only few authors have investigated which predictive factors can influence the outcomes in treating PP [8, 23, 24, 25, 26]. Most of the studies focused on parameters influencing the natural history of PP [13, 17, 18, 19, 20] or the treatment outcomes of previous pancreatitis. Furthermore, the various reports differ when considering the pancreatic etiology and the pathological background upon which PPs develop, namely, normal pancreatic tissue or tissue with features of acute or chronic pathology [7].
For these reasons, in the present retrospective study, we selected only those patients affected by PPs which followed an episode of acute pancreatitis and we investigated the role of possible predictive factors and their influence on treatment outcomes.
Age is an important epidemiological factor in the prognosis of acute pancreatitis and is one of the most important parameters of the Ranson score [28]. Nevertheless, Lankisch et al. report a marginal role of age in the course of acute pancreatitis and its complications [29]. In our study, age is a significant prognostic factor; in particular, we found an increase in the morbidity rate of about 10% for each year of age. Gender was not a significant predictive factor. The role of etiology in the course of PPs is controversially discussed in the literature [19, 20, 30]. Our data show that etiology of previous acute pancreatitis exerts an influence on the outcome, since a higher risk of complications in alcoholic vs. biliary pancreatitis was recorded (approximately 5 times). Nguyen et al. also found such a result in post-ethylic pancreatitis [19], whereas Pitchumoni and Agarwal have not reported any increased predisposition to PPs in this group of patients [17].
Fourteen out of 18 alcoholic patients examined (77.8%) were malnourished, and malnourishment was shown to be a negative prognostic factor in our study. In fact, the risk of morbidity was approximately ten times higher in malnourished patients. This datum is determinant in the decision to counteract hypercatabolism following the inflammatory process with proper therapy. According to this, several authors have emphasized the fundamental role of total parenteral nutrition and/or enteral nutrition, to improve outcomes in terms of complications, mortality and success rates [27, 31, 32, 33, 34, 35, 36, 37].
The Ranson criteria as an indicator of early unfavorable prognostic signs of preceding pancreatitis has been proven to be correlated with increasing pseudocyst size (giant PPs) and to predict the clinical and prognostic evolution of PPs identifying a group of patients who are at high risk due to the failure of non-operative therapy [30]. In our experience, the degree of the severity of previous acute pancreatitis is associated with worse outcomes, also after invasive treatment of the PP. In fact, an increase in the Ranson score by one degree entails an increase in the morbidity rate by approximately 80%. However, the recurrence rate is not significantly influenced.
The impact of size, number and location on the natural history of PPs is well known, but their role in the results of different treatments remains unclear [5, 13, 17, 18, 19, 26]. We were not able to find any relationship between these three factors and the success of the treatment. In particular, we did not confirm any data reporting worse outcomes in giant PPs (equal to or greater than 10 cm) [17, 30], confirming the data of an our previous study in which we reported that the size of the PP did not influence the outcome of invasive treatments [26].
In the group of patients in which the presence of intracystic residual necrosis was radiologically demonstrated (CT), the complication rate was particularly elevated (72.7% vs. 6.3%) suggesting a highly significant correlation between this condition and morbidity (P<0.001; OR=39.3). Several articles showed that intrapancreatic necrosis leads to severe complications such as sepsis and multi-organ failure and is responsible for death in many patients with acute pancreatitis [38, 39, 40, 41, 42, 43]. Furthermore, the risk of PP occurrence increases dramatically with the extent of the necrosis. This fact was demonstrated by Neoptolemos et al. who divided their patients into two groups (those who had either clinically mild pancreatitis or severe disease but with less than 25% necrosis on contrast-enhanced CT and no surgery for local complications and those who had clinically severe pancreatitis and/or had at least 25% necrosis on CT or underwent surgery for local complications) and showed that the incidence of PPs was 10% and 56%, respectively [44]. Other authors [23, 45, 46] also reported poor outcomes in patients with PPs containing necrotic debris. Twelve patients out of 74 (16.2%) achieved complete resolution of the PP with conservative management, 9 of them had a PP smaller than 5 cm and the remaining 3 patients had a PP of 5-10 cm. This rate is comparable to other studies reporting spontaneous resolution in 9- 40% of cases, particularly in those with smaller PPs [10, 12, 13, 19]. Invasive treatment was necessary for symptomatic or complicated pseudocysts and for PPs which did not resolve during an observation period of 8-10 weeks, beyond which spontaneous resolution was unlikely [17].
The complication rate between the two treatment groups, conservative or invasive, did not differ significantly whereas the condition of treatment, either elective or urgent, proved to significantly influence outcomes in terms of morbidity and mortality. Patients treated urgently (14/74) developed complications in 42.9% of cases as compared to 10.0% in elective treatment (P=0.008). Of the 10 patients treated through percutaneous drainage, 6 were treated for a quick discharge of the infected fluid and 2 due to poor general conditions (ASA IV; American Society of Anesthesiologists’ Physical Status for Preoperative Evaluation [47, 48]) which discouraged any surgical approach. In the remaining 2 patients the decision to drain the benign lesion was taken on patient's request who refused other surgical options. Percutaneous drainage was the procedure with the highest morbidity (50.0%) and the two deaths occurred in this group of treatment (20.0%). Unfortunately, the low number of cases does not allow us to draw a definitive conclusion about an increased risk of mortality. This preventive, but mandatory, selection of patients with specific (infected PP) or generic (ASA IV) high risk is probably the reason for such a poor outcome. In fact, several authors report better results in postnecrotic PPs in unselected patients treated percutaneously [6, 49, 50]. In contrast Heider et al. had worse results for mortality, morbidity and hospital stay in a similar group of patients as compared to those treated surgically [51].
Open surgery, including internal derivation and distal pancreatic resection, was performed in 37 patients with uncomplicated and mature PPs. Our post-operative results were comparable to those found in the literature [17, 52, 53]. Moreover, although distal resection is often considered a high-risk procedure in comparison to internal derivation, particularly in patients with hemorrhagic complications (intracystic or gastrointestinal bleeding), it has been proven to be safe when Intensive Care Unit support is available.
Endoscopic cyst-gastrostomy was carried out in PPs with visible endoluminal bulging, with a well-established maturation of the wall. All these cases were giant PPs (equal to or greater than 10 cm) and an endoscopic approach was often used in patients at high anesthesiological or surgical risk. In all 15 patients treated endoscopically, we achieved good results in agreement with other authors who reported excellent success rates [54, 55, 56, 57]. The endoscopic procedure also required only a short hospital stay (mean: 10.2 days) so that patients showed an increasing compliance towards this treatment. None of the risk factors we evaluated in our study was proven to be predictive for recurrence and, to the best of our knowledge, no predictive factors of recurrence have been identified in the literature.
In conclusion, our study points out that some epidemiological (age, etiology), clinical (severity of the pancreatitis, malnourishment), pathological (presence of residual necrosis), and therapeutic factors (emergency/urgency treatment) are indeed predictive, especially in patients in whom worse outcomes are expected when treating PPs invasively. In particular the presence of residual necrosis appeared to be the most important factor influencing invasive treatment outcomes, confirming that this pathological aspect deserves particular attention from surgeons. Building on these data, it would be advisable to lay down therapeutic guidelines for riskprone patients with the aim of improving the prognosis. However, no risk factors predicting recurrence emerged, so our study failed in selecting groups of treated patients who might benefit by a more careful follow-up.