- (2009) Volume 10, Issue 2
Mehrdad Nikfarjam1,2, Kevin F Staveley-O’Carroll2, Eric T Kimchi2, Jeffrey M Hardacre1
1Department of Surgery, University Hospitals, Case Medical Center. Cleveland, OH, USA
2Penn State Milton S Hershey Medical Center, Penn State College of Medicine. Hershey, PA, USA
Received December 2nd, 2008 - Accepted January 24th, 2009
Context Roux-en Y gastric bypass surgery is the most common operation for treatment of morbid obesity. The approach to pancreaticoduodenal resection in patients with a history of Roux-en Y gastric bypass is not well described. Case reports Pancreaticoduodenal resection was performed in two patients with distal bile duct strictures, with a past history of Roux-en Y gastric bypass. In both cases the remnant stomach, distal bile duct, duodenum and pancreas were excised. The biliopancreatic limb was divided close to the ligament of Treitz and brought up into the supracolic compartment in a retromesenteric manner and pancreatic and biliary anastomoses performed. The previous enteroenterostomy and gastrojejunal anastomoses were left intact. Both patients had an uncompleted post-operative recovery. The mean operating time was 6.5 hours and mean estimated blood loss was 525 mL. They were discharged home by days 6 and 7 post-operatively. Conclusions Pancreaticoduodenal resection can be successfully performed following Roux-en Y gastric bypass with en-bloc excision of the remnant stomach, with the pancreas and bile duct anastomosed to the divided biliopancreatic limb.
Anastomosis, Roux-en-Y; Gastric Bypass; Obesity; Pancreaticoduodenectomy
Morbid obesity is the medical epidemic of the 21st century, with surgery the only proven method of achieving sustained weight loss [1]. Laparoscopic Roux-en Y gastric bypass is the preferred operative procedure in the majority of cases, with increasing reports of significant health benefits following surgery [2, 3, 4]. Recent reports also demonstrate improved long-term survival following Roux-en Y gastric bypass surgery for the treatment of morbid obesity [5, 6].
Improvements in overall survival following Roux-en Y gastric bypass surgery has meant that non-obesity related abdominal operations will be increasingly encountered in surgical practice, with a greater need to appreciate post Roux-en Y gastric bypass anatomy. Pancreaticoduodenal resection, in the setting of a previous Roux-en Y gastric bypass may present major difficulties during the assessment, resection and reconstruction phases of the operation, if the altered gastrointestinal anatomy is not fully appreciated. The approach to pancreaticoduodenal resection in patients following Roux-en Y gastric bypass surgery is not well described. One approach to pancreaticoduodenal resection in the patient with a history of Roux-en Y gastric bypass is described in two patients.
Patients
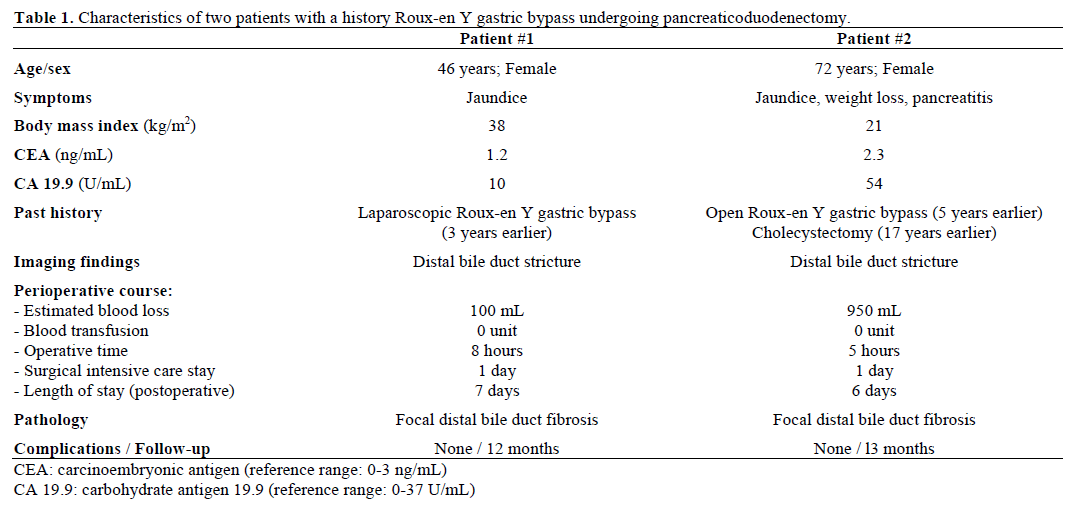
Two patients with distal bile duct strictures with a past history of Roux-en Y gastric bypass had a pancreaticoduodenal resection during the period July 2007 through August 2008. The patient details are shown in Table 1.
Preoperative Assessment
Complete work-up of patients for a possible periampullary malignancy was undertaken. This included computed tomography (CT) of the abdomen to assess for a mass lesion, exclude metastatic disease and aid in assessment of Roux-en Y gastric bypass anatomy. The presence of gallbladder stones was determined by transabdominal ultrasound. Carcinoembryonic antigen levels (CEA) and carbohydrate antigen 19.9 (CA 19.9) were undertaken. Transhepatic biliary stenting was performed in both cases to relieve jaundice and for further diagnostic workup. Biliary brushings were performed. Endoscopic access to the biliary tree was not attempted given the history of Roux-en Y gastric bypass surgery. Both patients had distal bile duct strictures concerning for malignancy (Figure 1).
Surgical Technique
Patients were placed supine on the operating table and prophylactic antibiotics were administered. Sequential compression stockings were utilized throughout the case. A midline laparotomy was performed and the abdominal cavity explored for signs of metastatic disease and determination of Roux-en Y gastric bypass anatomy. Local tumor resectability was assessed in standard manner.
An extended Kocher maneuver was performed to fully mobilize the duodenum with an effort to palpate a clear plane between any tumor and the pulsation of the superior mesenteric artery. The lesser sac was entered in the embryologic plane between the anterior leaf of the transverse mesocolon and the gastrocolic omentum. The gastoepiploic vein was divided as it entered the superior mesenteric vein. The superior mesenteric vein was identified and a tunnel was created in the plane anterior to it and the portal vein behind the neck of the pancreas. A retrograde cholecystectomy was performed if the gallbladder was present. Next, isolation and retraction of the distal common bile duct and ligation of the gastroduodenal artery was performed. The portal vein was exposed and a tunnel created anterior to it and traced to the tunnel made previously inferiorly. A Penrose drain was inserted in this groove.
Once resectability was determined, the Roux-en Y gastric bypass anatomy was further delineated (Figure 2). A standard Roux-en Y gastric bypass was identified, with a retrocolic Roux limb passing to the gastric pouch. The remnant stomach was further mobilized by dividing the short gastric vessels. Discontinuity of the remnant stomach from the gastric pouch was determined. The right and left gastroepiploic and left gastric arteries were divided. The greater omentum was not preserved. The proximal jejunum was divided approximately 5 cm from the ligament of Treitz, and the mesenteric vessels ligated close to the intestinal wall. The bile duct was divided at this time. The pancreatic neck was then transected across the tunnel previously formed anterior to the portal vein. Portal vein braches arising from the uncinate were divided and ligated. The specimen was then removed from the operative field. Intra-operative frozen section was performed on the pancreatic and bile duct resection margins.
Figure 2. a. Schematic diagram of classic roux-en Y gastric bypass configuration. The roux limb measures approximately 100 cm, while the biliopancreatic limb from the ligament of Treitz to the enteroenterostomy measures 40-50 cm. b. Reconstruction after pancreaticoduodenal resection en-bloc with the remnant stomach. The biliopancreatic limb is divided close to the ligament of Treitz and brought up in the same position as the duodenum for pancreatic and biliary anastomoses.
The divided jejunum adjacent to the ligament of Treitz was then traced to the site of previous jejunojejunostomy. In both cases this biliopancreatic limb was approximately 40-50 cm in length. The divided jejunum was brought up to the supracolic compartment through the defect created after dividing ligament of Treitz, in a retromesenteric, retrocolic position. Care was taken to insure that the previous jejunojejunostomy was not kinked and that there would be no tension on the pancreatic and biliary anastomoses (Figure 3). A few interrupted sutures were placed between the jejunum, retroperitoneum and small bowel mesentery to close small gaps and prevent further jejunal migration into the supracolic compartment.
Figure 3. a. Intraoperative photograph of completed reconstruction following pancreaticoduodenal resection. The pancreatic (P) and biliary (B) anastomoses to the remnant biliopancreatic limb in a retromesenteric position is shown. The original Roux limb to the gastric pouch is marked (*). b. Infracolic view of the previous enteroenteric anastomosis. The Roux limb (*) passing up to the gastric pouch in a retrocolic position. The biliopancreatic (BP) limb is also seen passing cranially to occupy the position of the resected duodenum. Kinking at the level of the enteroenteric anastomosis is avoided.
Pancreatic and biliary anastomoses were performed in a standard fashion, in the supracolic compartment (Figures 2 and 3). An end-to-side, duct to mucosa pancreaticojejunostomy was performed. No pancreatic stents were used. An end-to-side biliary anastomosis was formed using interrupted sutures. The previously placed transhepatic biliary stents were positioned across the anastomosis prior to complete reconstruction. Abdominal drains were placed adjacent to the biliary and pancreatic anastomoses. Feeding jejunostomy tubes were not utilized. The previous gastrojejunal anastomosis was checked at the end to ensure to there was no damage to this area. In one case gastroscopy was performed prior to abdominal closure to confirm the integrity of the previous gastrojejunal anastomosis.
Perioperative Management
Complications were recorded according to previously defined criteria [7]. Octreotide was not administered in these cases. Nasogastric tubes were not inserted. Patients were managed in an intensive care setting for 24 hours. A liquid diet was commenced on day 1 post operatively and progressed as tolerated. Drain amylase levels were measured on day 4 post operative and drains removed accordingly thereafter. Percutaneous transhepatic biliary stents were removed at the time of first office visit at 2 weeks post operatively.
Consent was obtained for each patient for the operative procedures performed. Review of charts was performed with institutional review committee approval. The study protocol conforms to the ethical guidelines of the Declaration of Helsinki.
Descriptive statistics: mean.
There were no complications in the two patients and outcomes are summarized (Table 1). The mean operative blood loss was 525 mL. The mean operative time was 6.5 hours. There were no intra-operative blood transfusions. The mean length of surgical intensive care stay was one day and patients were discharged home by days 6 and 7 post-operatively. The final pathology in both cases was a benign distal biliary stricture with no evidence of malignancy. Both patients were well at last follow-up.
Morbid obesity is a major cause of morbidity and mortality in modern society with surgery the only proven solution offering long-lasting weight loss [8]. With the success of Roux-en Y gastric bypass surgery for the treatment of morbid obesity, the long-term survival of these patients is likely to approach that of the general population [2, 5, 6]. This means that the likelihood of operating for non-obesity related abdominal problems in patients with a history of Rouxen Y gastric bypass will become more common in the future. There is naturally an increasing need to understand Roux-en Y gastric bypass anatomy and how it relates to other abdominal operations. The approach to pancreaticoduodenectomy in patients with a history of Roux-en Y gastric bypass requires a modified surgical approach, which has not been clearly defined.
We identified one previous report of pancreaticoduodenal resection in a patient with Roux-en Y gastric bypass surgery [9]. Others have also reported on pancreatic resection in patients with previous Roux-en Y gastric bypass surgery, in the form of distal pancreatectomy or duodenal preserving pancreatic head resection, but not pancreaticoduodenectomy [10]. In the report by Rutkoski et al. a classic pancreaticoduodenectomy was performed in a patient with pancreatic cancer and a history of Roux-en Y gastric bypass [9]. The remnant biliopancreatic limb was anastomosed to the remnant stomach. The small intestine was divided distal to the previous enteroenterostomy and a second Roux limb constructed for anastomosis to the pancreas and bile duct. The patient made an uneventful recovery. The authors claimed that retaining the remnant stomach may provide an access point for the introduction of a feeding tube in the future if nutritional concerns were to arise.
Retaining the remnant stomach in our opinion potentially increases operative morbidity following Roux-en Y gastric bypass, necessitating at least one extra anastomosis and usually a second, when a new Roux limb is formed. There is also significant literature showing that the remnant stomach is potential source of increased morbidity [11]. Gastrointestinal bleeding from the remnant stomach is well reported and the remnant is potentially at increased risk of malignancy. The remnant stomach was fully excised in our series, accepting that the remnant stomach may serve as a reservoir in case of malnutrition and has potential protective roles for certain vitamin deficiencies. In the case of a non-divided remnant stomach, this would require proximal division, with care to avoid damage to the gastric pouch and previous gastrojejunostomy. Retaining the remnant stomach when such a dissection is difficult may be justifiable. If the stomach is divided, then on table gastroscopy can be performed to further assess the integrity of the gastric pouch.
Reconstruction after a pancreaticoduodenectomy following a standard Roux-en Y gastric bypass can be safely performed using the remnant biliopancreatic jejunal limb alone. In standard Roux-en Y gastric bypass the biliopancreatic jejunum traced from the ligament of Treitz to the site of enteroenteric anastomosis measures approximately 40 to 50 cm. Division of the jejunum 5 to 10 cm from the ligament of Treitz allows the jejunum to be passed up into the supracolic compartment behind superior mesenteric vessels, in the position that the duodenum normally occupies, without tension. Importantly, in this position kinking at the site of previous enteroenterostomy appears to be avoided. Attempts at bringing the remnant biliopancreatic jejunal limb into the supracolic compartment through a separate defect created in the transverse mesocolon is more likely to result in tension and produce kinking at the previous enteroenterostomy. Under these circumstances a greater length of jejunum may need to be resected to provide enough mesenteric length for the intestine to reach the pancreatic and biliary anastomoses without tension. This may pull up the previous enteroenteric anastomosis and result in kinking. In both our cases the remnant biliopancreatic jejunal limb was divided close to the ligament of Treitz and could easily be used for biliary and pancreatic anastomosis in a retromesenteric position. Both patients made an uncomplicated surgical recovery and were tolerating a full diet at the time of hospital discharge.
In circumstances when the divided proximal jejunum cannot be safely anastomosed to the pancreas and bile duct without tension, we would favor modification of the Roux limb. The jejunum can be divided just proximal to the enteroenteric anastomosis, allowing the more distal small bowel, including the remnant biliopancreatic jejunal limb to be anastomosed to the pancreas and bile duct without tension. This same limb can be anastomosed to the remnant stomach, if it is to be left in-situ. A new enteroenterostomy can then be created more distally. This technique would preserve small bowel length and avoid formation of a blind pouch.
We have shown that pancreaticoduodenectomy can be safely performed following Roux-en Y gastric bypass. In most circumstances the gastric remnant should be excised en-bloc with the remaining specimen, with care to ensure gastric pouch integrity. The proximal jejunum is divided close to the ligament of Treitz and passed in a retromesenteric fashion for pancreatic and biliary anastomoses, avoiding tension and kinking at the site of the original enteroenterostomy. Although there are possible alternative methods for reconstruction after pancreaticoduodenal resection in the setting of Roux-en Y gastric bypass, the method described appears simple and effective.
Pancreaticoduodenal resection can be successfully performed following Roux-en Y gastric bypass with en-bloc excision of the remnant stomach, with the pancreas and bile duct anastomosed to the divided biliopancreatic limb.
The authors have no potential conflicts of interest