- (2015) Volume 16, Issue 5
Giulio Mari, Andrea Costanzi, Andrea Rosato, Jacopo Crippa, Alessandra De Scalzi, Elisa Galfrascoli, Michele Rossi, Angelo Miranda, Valter Berardi, Paola Sartori, Dario Maggioni
Department of General Surgery, AO Vimercate Hospital of Desio. Vimercate, MB, Italy
Received April 15th, 2015-Accepted May 25th, 2015
The placement of a stent in the Wirsung across the anastomosis is widely accepted to perform pancreaticojejunostomy during pancreaticoduodenectomy. Beyond being related to pancreaticojejunal anastomosis failure, stent placement can lead to other complications. Stent migration, stenosis of the pancreatic duct, obstruction, stent occlusion, intestinal obstruction, or fracture of the stent are reported as late complications after pancreaticoduodenectomy. Internal stents are supposed to pass spontaneously into and out of the bowel at a variable postoperative interval. However stent persistence in the gastrointestinal tract can be associated with subsequent complications. Their management is reported to be endoscopical when possible but also surgical when bowel perforation occurs. Despite the rarity of these complications, surgeons should be aware of their potential role in unclear post-operative abdominal pain when deciding whether to place a stent when performing a pancreaticojejunostomy.
Pancreaticojejunostomy; Pancreaticoduodenectomy; Stents
Pancreaticojejunostomy is one of the most challenging technical aspects of pancreaticoduodenectomy (PD). Avoidance of fistula formation is a major target for which a number of different surgical techniques to perform the pancreaticojejunal anastomosis have been proposed. The placement of a stent in the Wirsung across the anastomosis is widely accepted [1,2]. Stents may be useful in draining the pancreatic juice away from the anastomosis. They can also help in sustaining the anastomotic oedema especially in the immediate post-operative period [3,4]. Several analysis were conducted to determine the real anastomotic fistula rate after pancreaticojejunal anastomosis with or without stent placement [5,6]. Pancreatic fistula development has always been considered the main outcome to judge the use of stents on pancreatic surgery. However stent placement can also lead to other complications than pancreaticojejunal anastomosis failure. It has been reported from a retrospectively analyzed series by Kodawaky S. that even though internal short stent placed across the pancreaticojejunostomy usually passes spontaneously through the rectum, it remains unclear what happens to the stent after its placement. The same author refers that the median interval to stent defecation after PD was 454 days. A so long retained “foreign body” could therefore lead to early but also late post-operative complications [7]. However complications directly related to surgically placed internal stents in the pancreatic duct have only very rarely been reported. They include stent migration, stenosis of the pancreatic duct, obstruction, stent occlusion, intestinal obstruction, or fracture of the stent [8].
Methods
A systematic literature search was performed on PubMed, Embase, Cochrane. The following search strategies were used:
− Pancreaticojejunostomy [All Fields] AND Stent [all Fields]
− Pancreaticojejunostomy [All Fields] AND Stent Complication [all fields]
− Pancreatic Surgery [All Fields]) AND Stent Complication[All Fields]
− Pancreaticojejunostomy [All Fields] Stent Migration [All Fields]) AND Stent Retention [All Fields] AND Stent Occlusion
All titles and abstracts were assessed to select those focusing on stent related complications following PD. Fulltext of the selected trials were screened by the authors for eligibility. Google Scholar database was also used to search further articles. The references of the included studies were evaluated for other potential trials. We included comparative and non-comparative studies, case reports, retrospective series, irrespectively of their size.
The surgical issue about whether or not pancreaticojejunostomy should be tailored on a stent introduced in the Wirsung duct has been widely investigated [9,10]. Failure of pancreaticojejunostomy resulting in pancreatic leaks or, in particular, fistulas can lead to potentially life-threatening peritonitis, sepsis, or bleeding [11]. The use of pancreatic stent has therefore been judged in terms of anastomotic leak rates which usually occur as an early complication [12,13]. Very few studies nevertheless focused specifically on late complication after PD on patients and even fewer report either early or late stent related complications. The present study aim to collect and review the reported cases of pancreaticojejeunal stent related complications after PD. Data collected revealed how stent migration and stent retention are the clinical events closely and directly related to surgically placed pancreaticojejeunal stent.
Levy MJ reported 4 patients with retained pancreatic duct stents after PD for peripapillary tumor with creation of a pancreaticojejunal anastomosis by using an internal 8F Silastic stent [14]. 3 out of 4 patients had the onset of steatorrhea while one patient had recurrent pancreatitis. Steatorrhea significantly improved or resolved after stent removal. The patient with pancreatitis has not experienced another episode after stent removal. The retained pancreatic duct stent was identified during ERCP or EUS and endoscopically removed. It is important to point out how CT, and MRI failed to detect the stent in any patient. Ammori BJ reported a case of a patient who underwent pylorus preserving PD for Stage I ampullary carcinoma with a Roux-en-Y pancreaticojejunostomy constructed over a short stent. The patient was referred to ER complaining abdominal pain, steatorrhea, and weight loss 4 years after PD [15]. CT revealed a stent within the proximal pancreatic duct, with gross upstream ductal dilatation and parenchymal features of chronic pancreatitis. A laparotomy was required and the stent was removed through a jejunotomy. On-table pancreatogram demonstrated a 3-cm proximal duct stricture solved with a lateral pancreaticojejunostomy (Table 1).
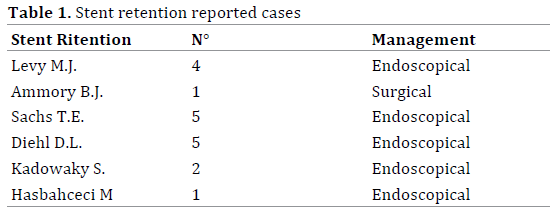
Sachs TE et al. described a large series of patients undergoing PD either with or without a stent guided pancreaticojejunostomy [8]. He referred 9 stents retained in situ beyond 6 weeks, 5 of which retained beyond 6 months. If stent retention beyond 6 weeks should not be considered pathological in the absence of clinical onsets, retention beyond 6 months cannot be seen as normal stent behaviour. Diehl DL et al. reported five patients who underwent pancreatic head resection (4 for adenocarcinoma, 1 for neuroendocrine tumor) and complained of abdominal pain several months after resection. CT detected the presence of retained stent in the pancreas extending to the jejunal limb. Endoscopic removal was successful in 3 of the 5 patients [16]. Kadowaky S et al. retrospectively analyzed 57 patients who had internal short stents placed across the pancreaticojejunostomy following PD. He reported two cases of acute pancreatitis due to retained stent [7]. Hasbahceci M et al. reported a 28 years old woman who underwent PD for pancreatic serous cystoadenoma of the head of the pancreas. 6 months after surgery CT scan was perform due to the onset of abdominal pain [17]. The internal pancreatic stent was retained within the dilated pancreatic duct. The stent was removed endoscopically.
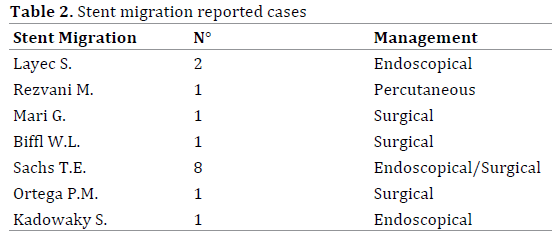
Layec S et al. reported two patients who underwent Whipple resection with Roux-en-Y reconstruction presented with migration of pancreatic stent tubes inserted in pancreaticojejunal anastomoses [18]. Both patients presented epigastric pain months away from surgery. CT scan detected a migrated stent stuck in a bowel loop. Removal was performed with double balloon enteroscopy. Rezvani M et al. reported a 61 years old woman underwent PD with internal stent across the pancreaticojejunostomy for adenocarcinoma of the pancreas. Four years after surgery patient was readmitted for abdominal and back pain associated to high temperature. A CT scan revealed liver abscess and identified the stent placed 4 years earlier across the pancreaticojejunostomy, which had migrated into an intrahepatic bile duct developing a hepatic abscess. A percutaneous approach achieved to remove the stent [19].
Mari et al. referred a case of a localized peritonitis occurred two years after PD for periampullary carcinoma due to a bowel perforation caused by a stent migration in a 53 years old man. Laparotomy was required to remove the migrated stent and bowel resection of the injured loops was performed [20].
Biffl WL et al. reported of 76 years old patients those 30 months after PD for neuroendocrine malignancy of the pancreas, developed progressive abdominal pain, nausea, vomiting, and costipation. Abdominal exploration, detected an intraluminal obstruction in the mid ileum. Enterotomy allowed extracting a bezoar that had formed around the migrated pancreatic stent [21].
Sachs TE et al. reported 8 case of stent migration after PD. In 4 cases stents migrated into the pancreatic-biliary limb and in 3 cases into the biliary tree. One stent eroded into the peritoneum causing a complete dehiscence of the pancreaticojejunal anastomosis [8]. Ortega PM et al. recently described a case of distal migration of a transanastomotic pancreatic stent resulting in bowel perforation 19 years after PD. Patient underwent surgery to remove the foreign body [22].
In his retrospective analysis Kadowaky S et al. also reported one case of a patient experienced acute cholangitis owing to migration of the stent across pancreaticojejunostomy to the bile duct [7] (Table 2).
The performance of PJ anastomosis during proximal pancreatic resections generally involves the use of stents according to surgeon’s discretion. Intra operative recognized risk factors for post-operative anastomotic leak formation usually indicate stent placement [14]. No precise guidelines for PJ anastomotic stenting have been developed. Internal stents are supposed to pass spontaneously into and out of the bowel at a variable postoperative interval [8]. However stent persistence in the gastrointestinal tract can be associated with subsequent complications. Radiological documentation of passage of internally placed stents, should therefore be considered, if internal stents are placed.
Pancreatic stents can be either free-floating or loosely tied to the Wirsung duct with a rapidly reabsorbable suture [20]. As underlined by this review stent related complications are very poorly reported. However, despite the rarity of these complications, surgeons should be aware of the possibility of stent retention and stent migration being the cause of unclear post-operative abdominal pain when deciding whether to place a stent during pancreaticojejunostomy. Management of stent retention, as reported, seems to be more endoscopical rather than surgical while stent migration has been treated endoscopically only when proximal. In the depicted cases of bowel perforation or bowel occlusion authors had to proceed with laparotomic exploration. No case of laparoscopic treatment of stent migration has been reported.
Trans-anastomotic pancreaticojejunal stent complications after PD are rarely reported. Stent migration and stent retention are mainly described. The management of such events can be either endoscopical or surgical when needed. Surgeons should be aware of the possibility of stent retention and stent migration playing a potential role in unclear post-operative abdominal pain at the time of the decision to place a stent when performing a pancreaticojejunostomy.
Authors declare to have no conflict of interest.