- (2007) Volume 8, Issue 1
Muhammad Wasif Saif*
Yale University School of Medicine. New Haven, CT, USA
Received September 9th, 2006 - Accepted September 23rd, 2006
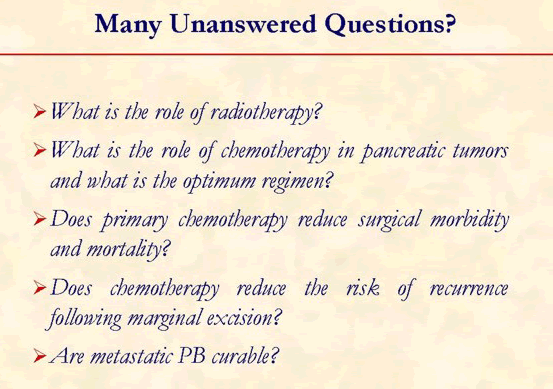
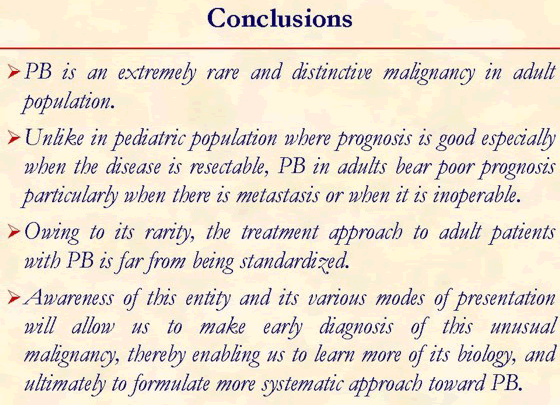
Pancreatoblastoma (PB), or infantile pancreatic carcinoma, is an extremely rare pancreatic tumor in childhood, comprising 0.5% of pancreatic non-endocrine tumors. Although PB mainly presents during childhood but can also occur in adults. PB tend to be less aggressive in infants and children compared to adults. Children with PB usually present late with upper abdominal pain and many have a palpable mass in the epigastrium. Mechanical obstruction of the upper duodenum and gastric outlet by tumor in the head of the pancreas may be associated with vomiting, jaundice and gastrointestinal bleeding. Histologically, PB is characterized with distinct acinar and squamoid cell differentiation. PB has been associated with alterations in the Wnt signaling pathway and chromosome 11p loss of heterozygosity (LOH), Beckwith-Wiedemann syndrome and familial adenomatous polyposis. The majority of these tumors arise in the head of the pancreas. Alpha-fetoprotein may be elevated in up to 68% of patients with PB. Ultrasound and CT scan may be useful but preoperative diagnosis is often quite difficult. The treatment of choice is complete resection, that may often be curative. The role of adjuvant chemotherapy or radiotherapy is still under discussion due to small number of patients treated as yet. Chemotherapy regimens consisting of cyclophosphamide, etoposide, doxorubicin, and cisplatin have been used in neoadjuvant setting with anecdotal benefit. Prognosis of this rare tumor is good, when resected completely. Prognosis is poorer, when there is metastasis or when it is inoperable. On the whole, PB is regarded to be a curable tumor; hence the clinical diagnosis should be made early. Awareness of this rare tumor of pancreas is essential for early detection and proper management. The author review the clinical presentation, etiology, diagnosis, treatment and prognosis of PB in this presentation.
alpha-Fetoproteins; Beckwith-Wiedemann Syndrome; Cisplatin; Doxorubicin; Hepatoblastoma; Infant; Pancreatic Neoplasms
LOH: loss of heterozygosity; PB: pancreatoblastoma
Pancreatoblastoma (PB), or infantile pancreatic carcinoma, is an extremely rare pancreatic tumor in childhood, comprising 0.5% of pancreatic non-endocrine tumors. Although PB mainly presents during childhood but can also occur in adults. PB tend to be less aggressive in infants and children compared to adults. Children with PB usually present late with upper abdominal pain and many have a palpable mass in the epigastrium. Mechanical obstruction of the upper duodenum and gastric outlet by tumor in the head of the pancreas may be associated with vomiting, jaundice and gastrointestinal bleeding. Histologically, PB is characterized with distinct acinar and squamoid cell differentiation. PB has been associated with alterations in the Wnt signaling pathway and chromosome 11p loss of heterozygosity (LOH), Beckwith-Wiedemann syndrome and familial adenomatous polyposis. The majority of these tumors arise in the head of the pancreas. Alpha-fetoprotein may be elevated in up to 68% of patients with PB. Ultrasound and CT scan may be useful but preoperative diagnosis is often quite difficult. The treatment of choice is complete resection, that may often be curative. The role of adjuvant chemotherapy or radiotherapy is still under discussion due to small number of patients treated as yet. Chemotherapy regimens consisting of cyclophosphamide, etoposide, doxorubicin, and cisplatin have been used in neoadjuvant setting with anecdotal benefit. Prognosis of this rare tumor is good, when resected completely. Prognosis is poorer, when there is metastasis or when it is inoperable. On the whole, PB is regarded to be a curable tumor; hence the clinical diagnosis should be made early. Awareness of this rare tumor of pancreas is essential for early detection and proper management. The author review the clinical presentation, etiology, diagnosis, treatment and prognosis of PB in this presentation [1].
[1]
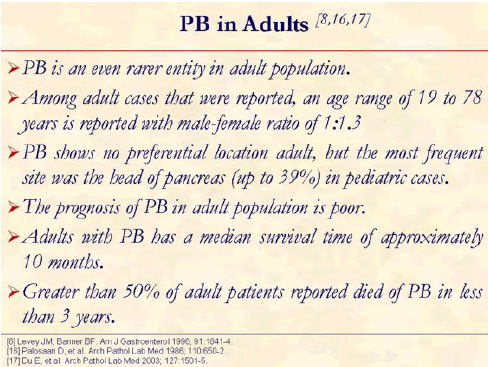
Pancreatoblastoma (PB), is an extremely rare pancreatic tumor of childhood, but can occur in adults. PB often exhibits elevated plasma levels of alpha-fetoprotein. PB, though not common, is said to be less aggressive in infants and children compared to adults [2, 3, 4].
PB is an extremely rare pancreatic tumor of childhood. The term PB was coined by Horie et al. in 1977 to describe tumors previously known as “infantile carcinoma of the pancreas” [5]. PB has several similarities to hepatoblastoma, including association with the Beckwith-Wiedemann syndrome and elevated plasma levels of alpha-fetoprotein (AFP) [6].
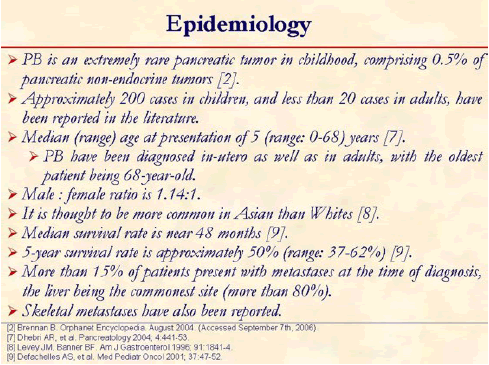
Pancreatic tumors are rare in children, and PB comprises only 0.5% of pancreatic non-endocrine tumors occurring in children. This tumor is more common in Asians than in the white population. They have also been diagnosed in-utero and in adults, with the oldest patient being 68-year-old. [2, 7, 8, 9]
The presenting complaints are varied (for instance we observed a patient who had no prior complaints and was identified following investigations after a motor vehicle accident). Children with PB usually present late with upper abdominal pain and many have a palpable mass in the epigastrium [1]. Mechanical obstruction of the upper duodenum and gastric outlet by tumor in the head of the pancreas can complicate with obstruction and gastrointestinal bleeding. Poor nutritional intake and the resultant weight loss may also be found.
Largest size reported in the literature reviews has been around 15 cm. Majority of the tumors are encapsulated, while the rest are partially encapsulated. Encapsulated tumors have a better prognosis. [1, 3]
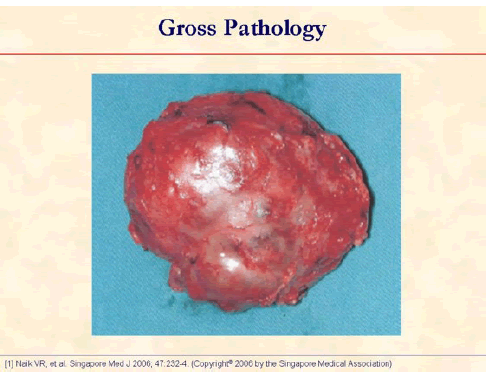
The specimen photograph shows an encapsulated tumor with a nodular surface. The capsule is complete [1].
Molecular investigation has disclosed a mosaic paternal 11p15 uniparental disomy in the tumor cells of PB. Recently genetic alterations also have been characterized and the commonest change is allelic loss of 11p. Familial adenomatous polyposis and Beckwith-Wiedemann syndrome have also een associated with PB. [6, 10, 11, 12, 13]
It is said to be that hamartomatous or dysembryogenic development of ductal cells of ventral portion of primordial pancreas lead to the development of PB. PB contains pluripotent cells capable of differentiating along the pathway of all three pancreatic cell types: acinar, endocrine and ductal. [14]
PB can exhibit acinar, endocrine and ductal differentiation. Histopathological features that are readily seen include hemorrhage, capsule formation and necrosis. [14, 15, 16]
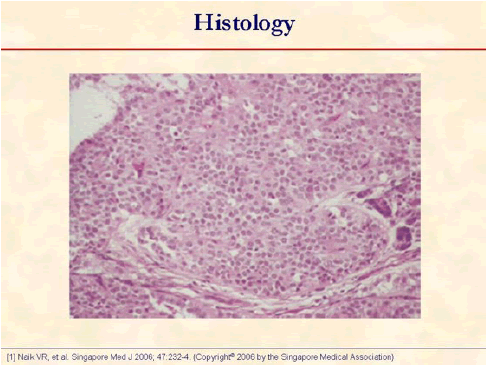
Photomicrograph shows a cellular tumor with uniform epithelial cells arranged in nests and acini (hematoxylin and eosin, x250) [1].
Immunohistochemistry is usually strongly positive for alpha-1-antitrypsin and glucose-6-phosphatase, in addition acid phosphatase, esterase and enteroprotease activity may be demonstrated using histochemistry. Stains for chromogranin, synaptophysin and neuron-specific enolase are often positive. Trypsin and chymotrypsin are usually found in acinar regions but positivity for specific peptide hormones is rare. Immunohistochemistry for AFP may be positive within solid regions of the epithelial component. Electron microscopy reveals multiple cytoplasmic neurosecretory zymogen granules. [15, 16]
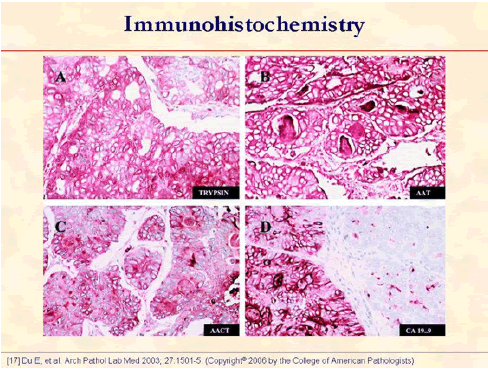
The tumor cells show strong positive immune reaction for trypsin (A), alpha1-antitrypsin (B), alpha1-antichymotrypsin (C), and CA 19-9 (D). Note that the luminal contents are positive for alpha1-antitrypsin (B), alpha1-antichymotrypsin (C), and CA 19-9 (D) (original magnifications x400) [17].
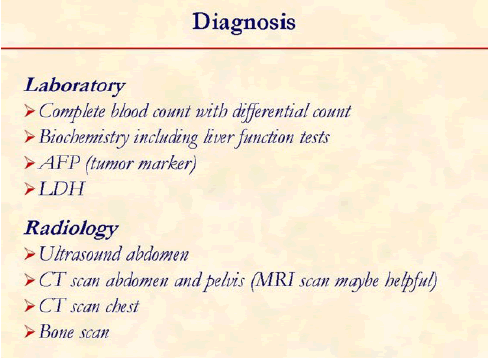
Biochemistry and radiology are the main diagnostic tools in PB.
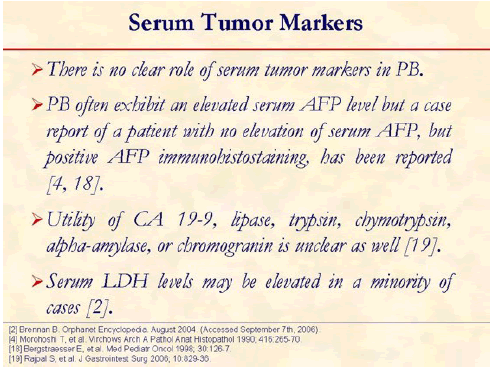
AFP is the most commonly used tumor marker in PB. Other tumor markers do not show any significant correlation. [2, 4, 18, 19]
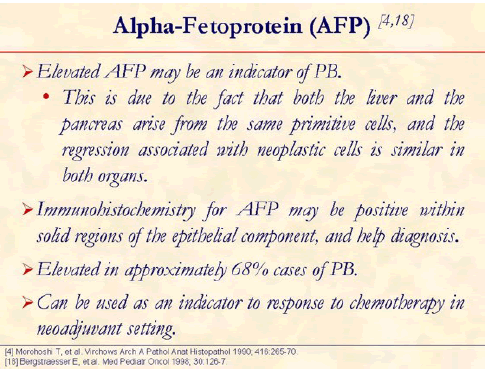
Elevated serum AFP levels have been reported in up 68% of cases. AFP level comes down once the tumor is resected. [4, 18]
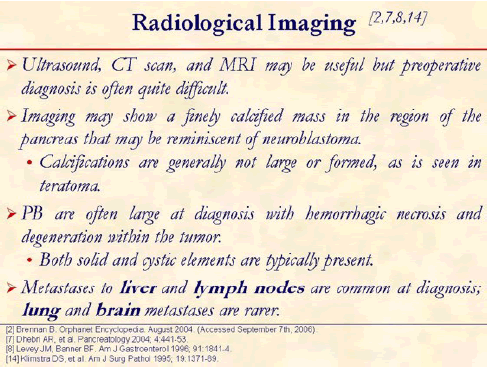
Radiological staging include a CT scan of abdomen, pelvis and chest. Bone scan or a brain MRI may be performed if clinically indicated. [2, 7, 8, 14]
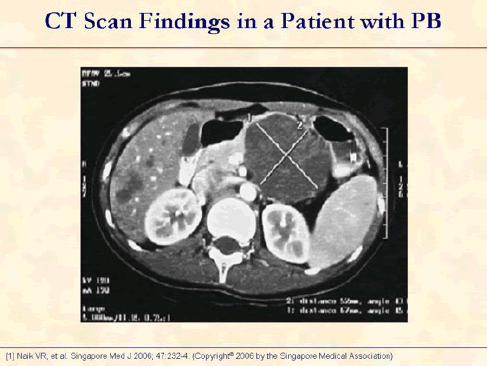
Enhanced axial CT image shows a large well-defined cystic tumor in the tail of pancreas and multiple small nodules in the liver [1].
The most common cystic pancreatic tumors in children are microcystic adenomas and cystadenocarcinomas.
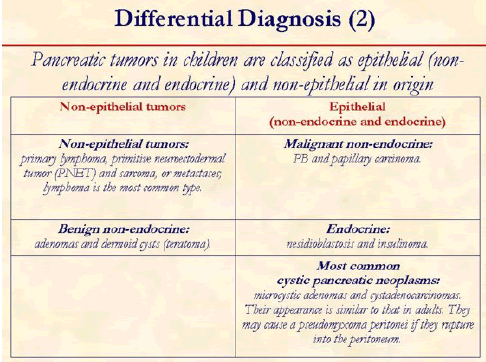
Differentiation of PB from other tumors is extremely important as prognosis of this rare tumor is good, when resected completely.
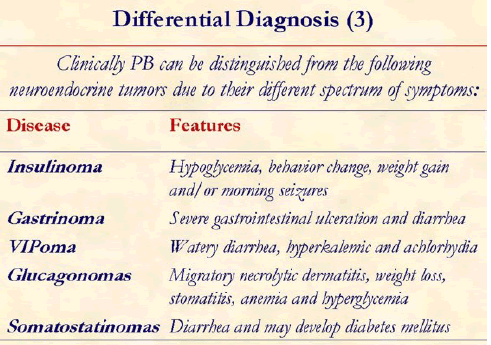
Clinically PB can be distinguished from the following neuroendocrine tumors due to their different spectrum of symptoms. Insulinoma: hypoglycemia, behavior change, weight gain and/or morning seizures; Gastronoma: severe gastrointestinal ulceration and diarrhea; VIPoma: watery diarrhea, hyperkalemic and achlorhydia; Glucagonomas: migratory necrolytic dermatitis, weight loss, stomatitis, anemia and hyperglycemia; Somatostatin-omas: diarrhea and may develop diabetes mellitus.
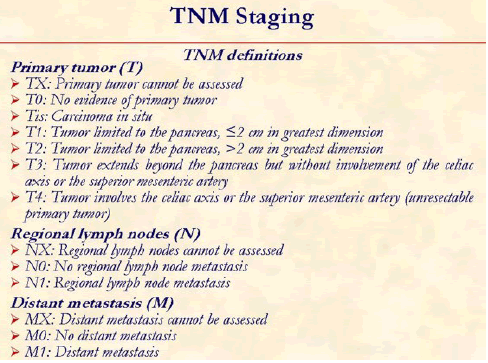
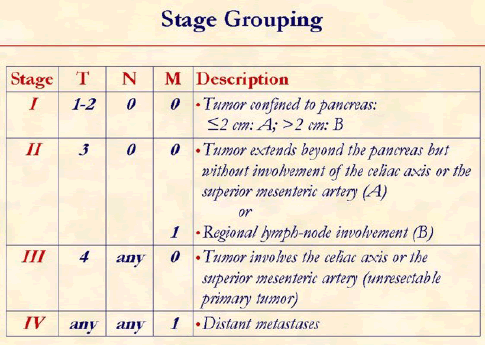
The tumor, node, metastasis (TNM) classification of the American Joint Committee on Cancer is usually used to determine the tumor staging [20].
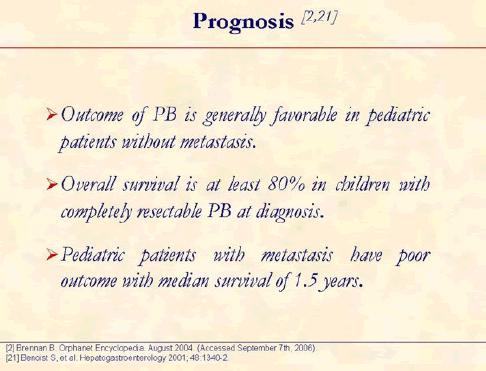
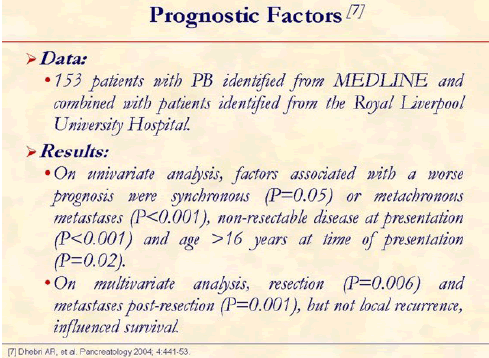
PB is less aggressive in infants and children compared to adults. Prognosis of PB is good, when resected completely. Prognosis is poorer, when there is metastasis or when it is inoperable. [2, 7, 21]
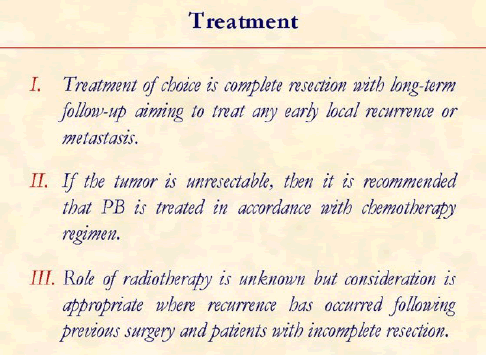
PB has an indolent course and is amenable for various modes of treatment but surgery is the most optimal treatment.
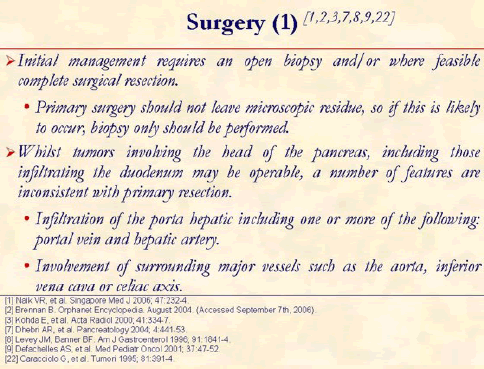
Complete resection of the tumor offers the best prognosis. However, in the presence of metastatic disease, it is of limited value. [1, 2, 3, 7, 8, 9, 22]
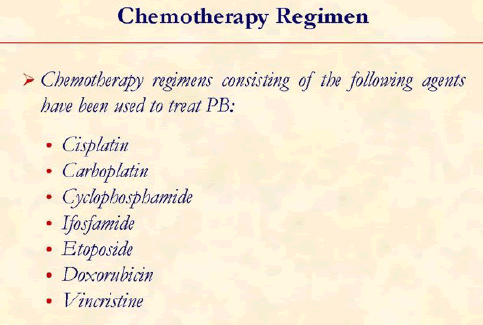
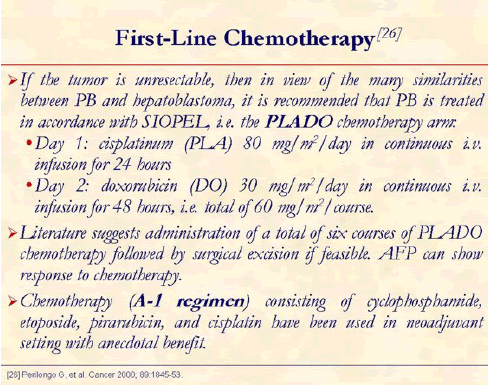
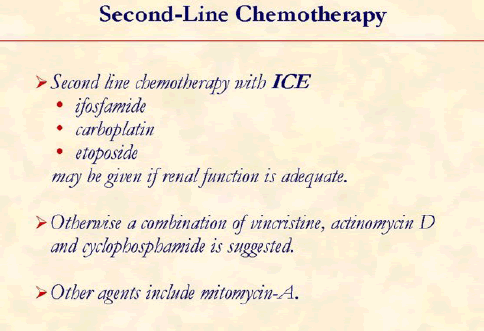
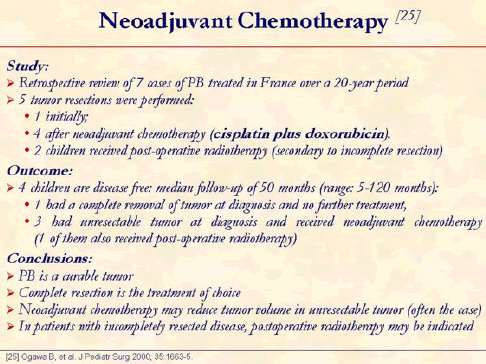
In these situations where there are suspected or documented metastatic lesions, empirical chemotherapy regimens that include cisplatin and doxorubicin have been used. A higher rate of metachronous metastasis has been reported in patients undergoing chemotherapy. [1, 2, 3, 7, 8, 9, 23, 24, 25, 26]
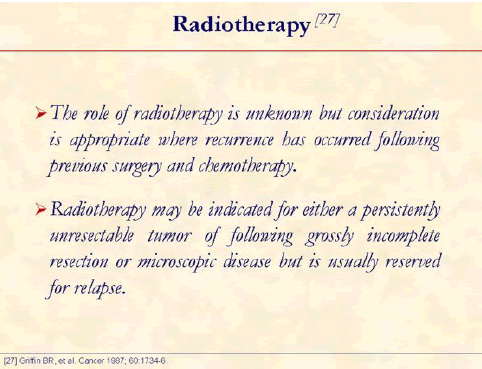
When the tumor is unresectable and the patient is non-responsive to chemotherapy, radiotherapy is given. Shrinkage of PB has been reported after treatment with radiotherapy [27].
We thank Dr. Naik [1] and Dr. Shabaik [17] for allowing us to reproduce figures from their publications. The figures have been reprinted with permission from: Singapore Medical Journal (SMJ), Copyright© 2006 by the Singapore Medical Association [1]; and Archives of Pathology and Laboratory Medicine, Copyright© 2006 by the College of American Pathologists [17]