- (2005) Volume 6, Issue 1
Ioannis T Virlos, H Priyantha Siriwardana, Yeliz Cemal, Ajith K Siriwardena
Hepatobiliary Unit, Department of Surgery, Manchester Royal Infirmary. Manchester, United Kingdom
Received September 11th, 2004 - Accepted November 30th, 2004
Objective This study examines clinical management pathways for patients with suspected pancreatic cancer within a singleUnited Kingdom Calman-Hine NHS cancer network with particular focus on referral patterns and the primary care-hospitalspecialist interface. Methods A questionnaire-based study appraising responses from three key groups (general practitioners, gastrointestinal physicians and gastrointestinal surgeons) practising within a cancer network. The questionnaire addressed caseload, referral pathways, multidisciplinary care teams and involvement of specialists. Participants The study population comprised 448 general practitioners, 14 gastroenterologists and 23 gastrointestinal surgeons. Results The mean number of new patients with suspected pancreatic cancer seen per general practitioner per annum was 0.4 (range: 0-1). Fifty-three percent of general practitioners refer to gastrointestinal physicians and 47% to gastrointestinal surgeons. In hospital, a relatively large number of physicians and surgeons see a small number of new patients each per annum. The involvement of multidisciplinary teams and referral of patients with nonresectable disease for chemotherapy is limited. Fourteen (60.9% out of 23 general surgeons) refer all patients to pancreatic specialists, 4 (17.4%) selectively refer and 5 (21.7%) never refer. Conclusion The findings suggest divergence in standards of care from those advocated in governmental cancer strategic plans. In particular, not all patients with suspected pancreatic cancer see specialists, many hospital specialists see small numbers of cases and multidisciplinary care is limited.
Cancer Care Facilities; Pancreatic Neoplasms
GP: general practitioners; MDT multidisciplinary care team; NHS: National Health Service
In 1994 there were 5,970 new registrations of pancreatic cancer in England and Wales giving an incidence of 11.7 per 100,000 for men and 12.0 per 100,000 for women [1]. As the prognosis of pancreatic cancer is poor, the mortality and incidence rates are approximately equivalent with a 1-year survival of 12% (95% confidence interval: 11-13) [1]. Noting that the equivalent 1-year survival for patients with pancreatic cancer in Europe is 15% (95% confidence interval: 14- 17), the current National Health Service (NHS) executive document on upper gastrointestinal cancer makes recommendations for improving outcome [1]. To help achieve these improvements in outcome, the current NHS plan targets additional resources for the management of patients with cancer. In order for resources to be used optimally, it is important to identify current pathways of care and the areas where such pathways may be modified. At the present time, there is a dearth of objective information on care pathways for patients with suspected pancreatic cancer and in particular on the primary care: hospital specialist interface. Detailed information on current care patterns can be obtained by analysis and matching of new diagnoses of pancreatic cancer, hospital discharge records and death registries. Similar information on referral pathways may also be gleaned by questionnaire survey. This approach has the advantages of providing a “snapshot” overview to offset the likely disadvantages such as incomplete response.
The aim of this study is to examine prevailing clinical management pathways for patients with pancreatic cancer within a single Calman-Hine NHS cancer network (the Greater Manchester and Cheshire network) [2]. The study assesses care pathways directly by focusing on three key groups of medical practitioners involved in the initial management of patients with suspected or proven pancreatic cancer: general medical practitioners, gastroenterologists and gastrointestinal (general) surgeons. The study uses questionnaire methodology to obtain a contemporary “snapshot” overview of the patient journey from initial presentation to point of contact with tertiary referral specialist and aims to highlight current referral pathways.
This study takes the form of a questionnairebased response appraisal. The study population that was targeted comprised all general practitioners (GPs), gastrointestinal physicians and gastrointestinal surgeons practising within a single United Kingdom Calman-Hine cancer network area (the Greater Manchester and Cheshire cancer network). Structured questionnaires were sent simultaneously to these three key groups of clinicians involved in the management of patients with pancreatic cancer. In addition, for general practitioners, a small subset of the group were interviewed directly using a faceto- face interview technique in order to ascertain information regarding GPs’ perceptions of the questionnaire and also as a reference population to compare GP response patterns.
Definition of Study Population
The Greater Manchester and Cheshire cancer network serves a population of approximately 3.5 million people living mainly within the Greater Manchester conurbation but also in rural and semi-rural areas.
The Information Technology Department of the Central Manchester and Manchester Children’s University Hospitals NHS Trust identified general practitioners practising within the boundary of the Greater Manchester and Cheshire cancer network by using the Organisation Codes Service of the Department of Health. This produced a list of 1,417 GPs who were sent questionnaires. Following the mail shot, a small group of 60 GPs were selected at random from within the principal cohort of 1,417 for face-to-face interview. Randomisation was carried out using random number generation. Regional weighting was used so that these 60 GPs were selected evenly from across the network and respondents were excluded if they had already answered a postal questionnaire.
Consultant physicians and surgeons were identified from the University of Manchester Postgraduate Deanery website (www.pgmd.man.ac.uk), from which it was possible to recognise consultant physicians with a specialist interest in gastroenterology and gastrointestinal surgeons. This information was augmented by knowledge of existing referral patterns, so that consultants, who had retired, moved out of the district or who were currently suspended from clinical practice were excluded from the study. This process identified 23 consultant gastrointestinal physicians and 47 consultant gastrointestinal surgeons from 13 hospitals across the Greater Manchester and Cheshire cancer network. During the period of this study, specialist pancreatic cancer surgery was provided by 3 surgeons within the Greater Manchester and Cheshire cancer network. These individuals were excluded.
The GP questionnaire (Appendix 1) focused on the following aspects:
i) demographic data: list size and estimated number of new patients with suspected pancreatic cancer per annum;
ii) availability of systems for recording and retrieval of data on patients with pancreatic cancer;
iii) perceptions regarding modes of clinical presentation;
iv) investigation and referral practice;
v) referral pathways from GP to hospital;
vi) gating of care (gating is used as a term to define a barrier to onward referral);
vii) perceived requirements for practical service improvement for patients with suspected pancreatic cancer
The gastrointestinal physicians’ questionnaire (Appendix 2) followed a similar format. Questions put specifically to this group focused on the initial management of the patient with suspected pancreatic cancer: the involvement of a multidisciplinary care team, the decision making process involved in palliation of jaundice and criteria for onward referral for specialist intervention (three key goals of the current upper GI cancer guidance document) [1].
The gastrointestinal surgeons’ questionnaire (Appendix 3) also follows the same format. Specific issues for the surgeons’ questionnaire included the involvement of multidisciplinary teams, staging and patterns of referral of patients with non-resectable for chemotherapy [2]. Respondents had the opportunity to remain anonymous and the questionnaire incorporated a “free text” box for further comments.
The study was closed for recruitment 8 weeks after initial mailshot. Data from replies were entered into a computer database (Microsoft Excel 97, Microsoft Co., Washington, DC, USA) and results were analysed.
The study was approved by the Central Manchester Research Ethics Committee.
Data are presented as means, medians, modes, ranges, and frequencies. Contingency tables are analysed by Fisher’s exact and McNemar tests using the SPSS for Windows version 10 (SPSS Inc., Chicago, IL, USA).
General Practitioners’ Responses
Of the 1,417 questionnaires sent to GPs, 391 replied giving a response rate of 27.6%. Of the 60 GPs approached for direct interview, one was not available when visited and two had answered the postal questionnaire and were therefore excluded giving 57 additional GP responses obtained by direct interview and a total of 448 (31.6%) GP responses.
i) Demographics: Numbers of New Patients with Pancreatic Cancer per Annum
The mean number of new patients with pancreatic cancer seen per annum was 0.4 (range: 0-1) with a modal number of 1. This was similar to the responses given by the face-to-face interview cohort where the mean was 0.3 (range 0-1) and the mode was 1.
ii) Availability of Systems for Recording and Retrieval of Data
Two hundred and seventy GPs (69.1% of the 391 questionnaire respondents) stated that their system of record keeping would permit them to identify and retrieve the records of patients with pancreatic cancer. This compared with 48 (84.2%) of the direct interview group (P=0.333).
The most frequent modes of presentation were perceived as follows on postal questionnaire (331 responses to this question): painless jaundice 159 (48.0%), non-specific symptoms 91 (27.5%), abdominal and/or back pain associated with jaundice 49 (14.8%) and abdominal and/or back pain alone 32 (9.7%).
iv) Investigation and Referral Practice
There were 384 respondents to this question on postal questionnaire. The majority of GPs carried out baseline haematological investigations before referring patients to hospital specialists. Age was a significant factor in selecting those patients for immediate referral to hospital: 298 (77.6%) GPs would carry out investigations before referral in a patient under 40 whereas 191 (59.7%) would implement a similar policy in patients over 40 (P=0.009; McNemar’s test).
v) Referral Pathways from GP to Hospital
One hundred and forty seven (52.7% of 279 respondents) referred patients directly to hospital physicians and 132 (47.3%) referred to gastrointestinal surgeons. In direct interviews 26 (59.1% of 44) referred directly to physicians compared to 18 (40.9%) to surgeons. There was no significant difference between postal questionnaire respondents and direct interviewee responses (P=0.516; Fisher’s exact test).
vi) Gating of Care
There were 390 responses to this question: 295 (75.6%) would refer all with a diagnosis of suspected pancreatic cancer and 95 (24.4%) refer selectively. Reasons for nonreferral included patient preference (81 replies, 85.3%) and the presence of comorbidity (64 replies with more than one response permitted, 67.4%).
vii) Improvements to Services
There were 347 respondents to this question and the most frequently cited response was the need for rapid access to outpatients (158; 45.5%) followed by rapid access to a specialist pancreatic cancer centre (81; 23.3%).
Gastrointestinal Physicians’ Responses
Of 23 gastrointestinal physicians, 14 responded giving a response rate of 60.9%.
i) Demographics: Numbers of New Patients per Annum
The median number of new cases seen per annum was 5 (range: 3-11).
ii) Availability of Systems for Recording and Retrieval of Data
Five (35.7% of 14 respondents) had systems of record keeping that allowed them to identify and retrieve data on patients with pancreatic cancer.
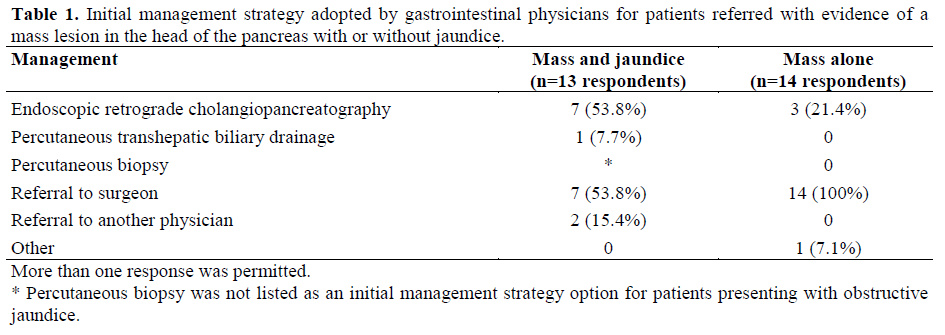
iii) Initial Management
Initial management strategies are seen in Table 1. Eight (57.1%) incorporate a multidisciplinary care team (MDT) in the decision-making pathway. The composition of these 8 MDTS was as follows: gastrointestinal physician 8 (100%), gastrointestinal surgeon 7 (87.5%), radiologist 7 (87.5%), oncologist 7 (87.5%) and a histopathologist in 4 (50.0%).
iv) Palliation of Jaundice, Pain and Referral for Chemotherapy
Preferred options for palliation of jaundice was given by 12 physicians only and was as follows: endoscopic metal stent 6 (50.0%), endoscopic plastic stent 5 (41.7%) and percutaneous transhepatic stent 1 (8.3%). No gastrointestinal physician referred patients for surgical biliary bypass as a primary option for palliation of jaundice. In terms of pain relief (more than one option was permitted in response to this question) 8 (57.1%) refer to a specialist pain team, 7 (50.0%) commence analgesia with opiates and 6 (42.9%) with non-opiates. Two (14.3%) utilise coeliac plexus blockade. Following initial treatment, 7 (50.0%) referred patients for chemotherapy.
Of 47 gastrointestinal surgeons, 23 responded giving a response rate of 48.9%.
i) Demographics: Numbers of New Patients per Annum
The median number of new patients seen per annum was 3 (2-5).
ii) Availability of Systems for Recording and Retrieval of Data
Ten (43.5%) had systems of record keeping that allowed them to retrieve data
iii) Initial Management, Referral to Pancreatic Cancer Specialists and Involvement of Multidisciplinary Care Teams
Fourteen (60.9%) referred all patients to a specialist pancreatic cancer team, 4 (17.4%) only refer selected cases and 5 (21.7%) never refer to a specialist pancreatic cancer team. Six (26.1%) involved a multidisciplinary team in decision-making
iv) Staging of Potentially Resectable Disease
Fifteen (68.2%) utilised computed tomography and 5 (22.7%) undertake laparoscopy. Laparoscopic ultrasound was available to two (9.1%) while one respondent did not answer. None of these respondents would ordinarily undertake pancreatic resection.
v) Palliation of Jaundice, Referral for Chemotherapy
For patients with non-resectable disease an endoscopically placed metal stent was the preferred option for 8 (34.8%) and a plastic stent for 4 (17.4%). No surgeons use surgical biliary bypass as first option for palliation of jaundice. However, if surgical biliary bypass was eventually utilised 8 (80.0% of 10 respondents to this question) combined prophylactic gastroenterostomy with biliary diversion. Ten (43.5%) referred patients with unresectable pancreatic cancer for chemotherapy.
The key to interpretation of the findings of this study is the avoidance of overinterpretation. The results of this nongovernmental, voluntary questionnaire should not be regarded as representative of the views of general practitioners (or their hospitalbased colleagues) within the Greater Manchester and Cheshire cancer network. The results simply represent the views of a cohort of respondents. Further, as with all questionnaire surveys, replies may be prone to biased and/or idealised response patterns [3, 4, 5]. Nonetheless, bearing these limitations in mind, this study represents one of the largest cohort responses from general practitioners on care pathways for the management of pancreatic cancer in the era of cancer networks and is possibly unique in targeting three tiers of clinician simultaneously.
As expected, the number of new patient presentations with pancreatic cancer per annum to GPs is low. GPs are critically involved in decision-making regarding referral to hospital and also on gating of referrals. The response patterns of the direct GP interview cohort were reassuring in that they tended to support the views of GP respondents to postal questionnaire. Referral patterns incorporating physicians and surgeons (for patients with suspected pancreatic cancer) may reflect local service provision issues and uncertainties in diagnosis but are likely also to reflect the lack of implementation of a cohesive referral policy. The need for cancer network strategies to incorporate GPs in decision-making and care pathways is highlighted by those practitioners who elect not to refer patients with suspected pancreatic cancer. Current United Kingdom Department of Health guidance is that all patients with pancreatic cancer should have the benefit of a specialist opinion [1]. Whilst frail patients with major co-morbidity should be spared un-necessary intervention [6], the decision makers must be aware of the existence of cancer networks and in turn, networks must reach the primary care level. The study sample elicits responses from greater proportions of hospital physicians and surgeons than GPs yet the collated replies show evidence of considerable variation in management. Examining the responses of gastrointestinal physicians (accepting that other physicians will also receive these patients and that physicians may refer outwith the network) it is apparent that a relatively large number of gastroenterologists see a small number of patients per individual doctor with just over half the physicians having some form of multidisciplinary team involved in decision-making. The composition of these teams appears variable. Use of chemotherapy in non-resectable patients is not widespread and there is considerable variation in methods of symptom-palliation. These trends are also present in the responses of gastrointestinal surgeons. However, the finding that 14 (60.8%) referred all patients to pancreatic surgical specialists is encouraging in the light of data on surgeon volume and outcome [7]. This study does not address the controversial areas of centralisation and resource distribution. The use of staging laparoscopy and laparoscopic ultrasound by surgeons who will not undertake resection was an interesting and unexpected finding. Although the availability of this equipment may be indicative of surgical expertise in a related discipline of gastrointestinal oncology such as oesophago-gastric surgery it is difficult to understand why 5 surgeons state that they undertake laparoscopy in these patients (presumably prior to referral). In conclusion, this study presents the results of a questionnaire survey into referral pathways for patients with suspected pancreatic cancer amongst clinicians practising within a single United Kingdom Calman-Hine cancer network. The responses should not be interpreted as a representative statement from this network and although the variations in care highlighted by this study are likely to be present across the United Kingdom (and also in other healthcare systems) direct extrapolation to other networks or health care systems may not be appropriate. Nonetheless, the cohort of 448 GPs represents one of the largest surveys to date of attitudes to the management of pancreatic cancer amongst primary care physicians. Given that patients with pancreatic cancer often present first to their GP, that not all GPs refer on to a specialist and taking into consideration that the mean number of new diagnoses per GP per annum is low (i.e., equal to 0.4) it can be observed firstly, that cancer networks must reach the primary care level and secondly, that it may be difficult to elicit active participation by GPs in the care of a condition which these doctors see extremely infrequently. The findings suggest that there is considerable divergence in standards of care from those suggested in governmental cancer strategic plans. In particular, not all patients with suspected pancreatic cancer have the opportunity to see a pancreatic specialist, there is wide variation in initial referral patterns, many hospital specialists see small numbers of cases and multidisciplinary care teams are not universally utilised. Although these findings are predominantly based on responses to postal questionnaires and thus must be interpreted with caution, the results constitute a valid and important observation with potential implications for the structuring of cancer specialist subgroups.
The authors acknowledge the time and effort taken by colleagues across the Greater Manchester and Cheshire cancer network to complete these questionnaires. The authors are indebted to Dr. Gavin Thoms of the Manchester Royal Infirmary for his input into the design of the study. A poster based on this study was presented at the American Gastroenterology Association, San Francisco, CA, May 2002 (abstract in Gastroenterology 2002; 122 (Suppl.):185).