Key words
healthcare professional, lesbian couple,
planned parenthood, queer theory, relationships,
transition
Introduction
Historically, lesbian women parented children from
their past heterosexual relationships in stepfamilytype
formations (Bos et al, 2007). More recently,
lesbian couples have started to plan their own families
using donor insemination, with one member of the
couple being the biological parent (Golombok, 2000).
Such changes in family structures can be expected to
have an impact on the couple relationship.
This paper reports the findings from a wider study
(O’Neill et al, 2012) about lesbian women’s reports of
their interactions with healthcare professionals. This
study follows previous research, including lesbian
women’s experiences of maternity care in the UK
(Wilton and Kaufmann, 2001), their experiences of
childbirth (Buchholz, 2000), and heteronormative
communication with lesbian families over the transition
to parenthood (Ro¨ndahl et al, 2009). Although
this literature has acknowledged lesbian perspectives
on health and maternity care, the current study aimed
to add specific knowledge of the impact on their
couple relationships.
Transitioning to parenthood
The transition to parenthood commences at conception
and continues through the first few months
following a baby’s birth; it is a major occurrence in the
relationship (LeMasters, 1957; Goldberg, 1988). Heterosexual
couples struggle with issues related to role
polarisation post-birth (Katz-Wise et al, 2010). For
example, a study of relationship quality by Kurdek
(2008) found that heterosexual couples reported a
marked decline in their relationship following the
birth of their first child, with another decline towards
the end of the 10-year period surveyed. A quantitative
study by Goldberg and Sayer (2006) of 29 lesbian
couples revealed that these couples experienced similar
relationship changes and increases in conflict with
the transition to parenthood.
Lesbian-led families are seen as deviating from the
norm. For this reason they are researched from a perspective
which assumes that heterosexual families are
superior (Stacey and Biblarz, 2001).According to Golding
(2006), because lesbians are raising children in a society
where lesbians are perceived as deviant, this complicates
the process of becoming a parent. Research has
focused on the similarities between heterosexual and
lesbian mothers to avoid criticism of the lesbian-led
family (Vanfraussen et al, 2003).Dempsey(2010, p. 1151)
discussed the ‘reproductive relationship’ whereby
parenting responsibilities do not rely on biological
links. Lovelock (2010) affirmed that lesbian and gay
families reject the notion that biological connections
to children are important in the role of parenting.
The theme of heteronormativity and homophobia is
constant throughout the literature; differences between
lesbian-led families and heterosexual families relate to
the pressures that the former experience with regard to
heterosexual dominance (Bos et al, 2007; Ryan and
Berkowitz, 2009; Bos and van Balen, 2010). Although
the differences in terms of family functioning appear
to be minimal, the healthcare needs of lesbian women
and their families are unique, as they face stressors and
challenges that heterosexual families do not. Lesbian
couples undergo changes similar to those reported by
heterosexual couples, including lack of sleep, changes
in patterns of socialising, changes in sexual relationships,
and prioritising the role as a parent over that as a
partner (O’Neill et al, 2012). Heteronormativity featured
over the transition to parenthood and to the
detriment of their intimate relationship.
Heteronormativity and healthcare
Heteronormativity refers to embedded social, cultural
and institutional norms that affirm homosexuality as
abnormal and heterosexuality as natural and normal
(Warner, 1993). Assumptions that are made about
gender and heteronormativity negatively influence
the care of lesbian women (Beagan et al, 2012). For
instance, gay men and lesbians have higher rates of
mental health disorders, self-harm and suicide attempts
(King et al, 2008), due to the effects of homophobia
(Meyer, 2003; Meyer et al, 2007; Cochran et al, 2003;
Cochran and Mays, 2009; Kertzner et al, 2009; Lewis
et al, 2006). According to Weber (2008), gay men and
lesbians who experience high levels of homophobia also
have significantly higher rates of drug and alcohol abuse.
Despite relevant health-related factors among the
gay and lesbian population, Markus et al (2010)
suggested that health practitioners may be unaware
of their patients’ non-heterosexual identity. The fact
that lesbian women often ‘pass’ as heterosexual means
that their invisibility is perpetuated (Mohr and Daly,
2008, p. 990), and they have to make decisions about
whether to make multiple disclosures of their lesbian
identity to healthcare professionals at the time of
planning and conception, during pregnancy, at
childbirth and while parenting (Steele et al, 2008). St
Pierre (2012) has discussed the ways in which lesbian
women disclose their identity to healthcare professionals,
and she concluded that a lesbian woman
will be explicit in her disclosure of her identity if the
attitudes and behaviour of the health professional
make her feel that it is safe to do so.
The research aim
The overall study examined lesbians’ transition to
parenthood. This paper presents findings related to
lesbians’ perceptions of healthcare professionals.
Method
Ethical considerations
Lesbians are a vulnerable group, so care must be taken
to reduce susceptibility to harm during the research
process (James and Platzer, 1999). A participant information
sheet outlined the risks and benefits of the
research. Potential participants were given the opportunity
to ask questions about the research before
signing the consent form. In order to maintain confidentiality,
participants were assigned pseudonyms
by the researcher; these were used in all data collection
and transcripts. Confidentiality was maintained further
by excluding the names of the participants’ children,
their partners, their age and any other identifying information.
Data were stored on a password-protected
computer and only viewed by the researcher and her
supervisors. The University of Auckland Human Participants
Ethics Committee approved the study (Reference
number 2010/357).
Recruitment and participant
characteristics
In order to contact possible participants, an advertisement
was placed on an Internet site for female
same-sex parents, and in a local women’s centre. The
advertisement described the study and invited lesbian
women to contact the researcher for further information.
Eight women who identified as lesbian and as
having been in, or currently being in, a lesbian relationship
where they had chosen to have a family
together and conceived through artificial insemination,
agreed to participate. All of the women identified
themselves as being of European descent and had
completed university study; six had Diplomas and two
had Master’s degrees. Their ages ranged from early
thirties to late forties, and they lived in or around three
of New Zealand’s major metropolitan cities. Two of
the women were non-biological mothers, five were
biological mothers, and one woman was both a
biological and a non-biological mother. The age of
the participants’ children ranged from 9 months to 12
years.
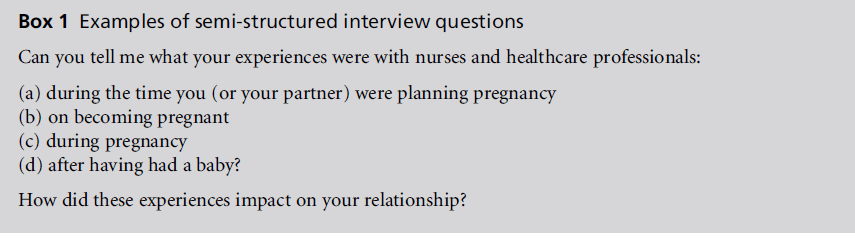
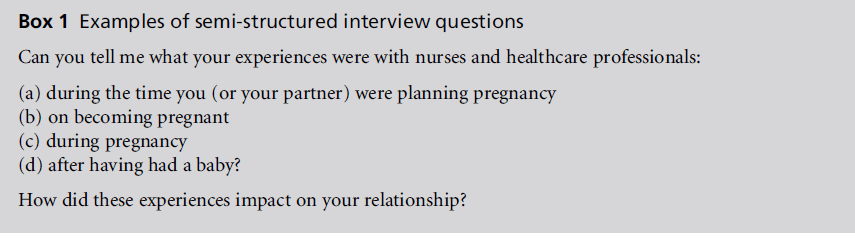
Data collection
The first author conducted the interviews in participants’
homes and in one workplace. The interviews
were semi-structured and the questions were openended
(see Box 1). This enabled the researcher to
obtain specific information and participants to provide
information from their own experiences and views
on the subject. Consent was sought for the interviews
to be recorded using a digital voice recorder. Interviews
were transcribed verbatim. The data reached
saturation after three interviews, and continued to be
replicated throughout the remaining interviews.
Data analysis
A general inductive approach (Thomas, 2006) was
used to analyse the data. This approach allows the
research findings to emerge from the data without the
restrictions associated with a specific methodology.
Each interview transcript was read several times and
sections of the text were assigned codes for easy
reference. All of the codes were placed into nine broad
categories. Data were further refined and finally three
main themes emerged, namely planning a family,
impact of baby on the relationship and responses of
others. The latter category particularly concerned the
way in which lesbian women perceived health professionals’
responses, and is the focus of this paper.
Queer theory
Queer theory was used as a theoretical framework to
interpret the findings. It originated from work by
Teresa De Lauretis (1991), and is characterised by a
number of different theories, all of which use the
description of queer. For this reason, queer theory
merges with other theoretical viewpoints, such as
feminist theory and its many earlier contributors
(Jagose, 1996). Queer theory embraces the complexity
of identity and rejects the idea that people can fall into
categories or be labelled, and it can assist in examining
ways in which sexual or gender differences are discussed
(Henderson, 2003) and in exploring power
dynamics (Watson, 2005). Oppression and identity
can therefore be viewed through the queer lens. For this reason, queer theory has a place in the agenda of
examining family, and the forging of social relationships
(Henderson, 2003), and as Minton (1997) has
suggested, it focuses on universalising issues within
the context of sexual diversity.
Queer theory aims to deconstruct and destabilise
the idea of fixed sexual and gender identities, thus
prompting examination of identity politics (Lovaas
et al, 2006). Butler (1990) suggested that women
perform in ways they believe they should because of
social stereotyping; sex and gender are a production of
heteronormativity (Lloyd, 2007). Two women who
choose to have children must involve a third party
who is then linked, biologically, to the family (Folgero,
2008). Genetic and biological parenthood, as well as
female and male roles, are disrupted. Lesbian couples
who transition to parenthood fall outside the dominant
construction of what is family.
Reflexivity
In terms of integrity, a clear and honest approach
towards research is imperative (Watts, 2008). Transparency
about holding multiple and shared positions
is essential for increasing rapport between the participant
and researcher (Almack, 2008). There is ongoing
debate about whether it is necessary for researchers to
identify their own sexual orientation in studies related
to sexuality (Almack, 2008). Given this debate, the
first author chose to declare, prior to interviewing,
that she was a lesbian, a nurse, and in the process of
planning a family. The participants commented that
this knowledge reassured them that their lesbian
cultural perspective was understood.
Reflexivity relates to the intentional or unintentional
influences that are involved in the research
process and influence research findings (Jootun et al,
2009). Queer theory’s role in reflexivity relates to complexities
associated with researcher identity (McDonald,
2013). Queer reflexivity requires the researcher to
consciously decide whether to disclose or hide their
sexual identity. This can change the research process
and the relationship between researcher and participant,
particularly in relation to power. In developing
reflexivity in the current study, the first researcher
explicitly identified assumptions relating to the research
topic, for instance, that ‘lesbian relationships
should be, but are not, valued equally to heterosexual
relationships.’ Such assumptions were used in the
reflexive analysis process to challenge interpretation
of data. The data analysis process was also overseen by
the second and third authors, who played a role in
linking queer theory to the participants’ experiences.
Findings
The findings are discussed in relation to five interrelated
themes, namely couple affirmation, seeking
allies, devaluing the couple, power and the full disclosure.
Couple affirmation
Although responses to the lesbian-led family by
healthcare professionals were varied, most of the
participants reported a positive experience. For
example, Alex reported that ‘in hospital during the
birth and that kind of thing, it was a real acknowledgement
that we’re both parents.’ Leah found it
helpful that her relationship was respected in that no
one referred to the ‘daddy’; she felt protective of her
partner being recognised as a parent despite being a
non-biological mother. It was important that participants
felt an acceptance of their lesbian relationship,
without it being examined or judged through the
imposition of healthcare professionals’ heteronormative
assumptions.
Alex emphasised that the recognition of both her
and her partner as being the parents made them feel
safe and comfortable. She acknowledged that this
‘safe’ response had been influenced by the steps taken
by other lesbians who had previously forged the way,
resulting in wider change and acceptance of their
identity as parents, not only in the health environment
but also in wider society. These women who had
started lesbian-led families or raised children within
lesbian relationships were felt to be instrumental in
making Alex’s more recent experience with healthcare
professionals acceptable and non-discriminatory: ‘And I
think it’s really changing, the world actually. And I
think we need to acknowledge people who have come
before us.’
Seeking allies
The participants noted that some healthcare professionals
were more lesbian-friendly than others. Some
responded naturally, creating a sense of safety:
We had a very good obstetrician, he was very up front and
supportive. ... I felt very comfortable with him. We had a
nurse there who was clearly against the idea and quite
quickly she made her feelings known. And we stopped
having anything to do with her.
(Karen)
Participants reported actively seeking healthcare professionals
who were known to be sensitive and friendly
towards lesbian couples, or who were out as lesbians
themselves. The proactive approach to finding lesbian friendly healthcare professionals was aimed at protecting
themselves from homophobia:
A friend of ours was a midwife, so she had mates who she
recommended. ... There’s actually quite a few of them out
there ... we had recommendations from [a family group
for gay parents], mums as well, who’d used lesbian
midwives.
(Natalie)
Other lesbian-friendly professionals were encountered
by chance. Karen and Laura accidentally came
into contact with empathic staff, having previously
encountered other healthcare professionals who had
been involved in unsatisfactory and judgemental care:
‘there was one woman there ... she was a lot more
friendly with me so we just worked through her’
(Karen).
Devaluing the couple
Three participants reported negative experiences of
healthcare. Another felt that her healthcare experience
had been positive since her relocation to New Zealand,
but nevertheless she had had experiences of inappropriate
or judgemental care in her country of origin.
The challenges associated with negative encounters
were demeaning and harmful:
And the nurses were awful. There were two in particular,
one who was very religious and I don’t know what the
other one’s excuse was. ... And then, by chance we got
a different nurse to do the procedure. And she was
gorgeous. She was just lovely. She was so the opposite of
[nurse who was hostile] and that was when I conceived.
(Laura)
The following quote illustrates a heteronormative
experience encountered when Laura and her partner
were interviewed by a social worker inNew Zealand to
decide whether they were suitable candidates for
becoming parents:
She had the most appalling ideas about lesbian relationships
... she said things during the interview like ‘It would
be better for the child if you found someone in the pub,
slept with them and got pregnant, because at least then
your child would know who the father was ... least then
your child would have a father.
(Laura)
To Laura and her partner, this experience was ‘appalling.’
The socialworker highlighted heteronormativity
by emphasising the importance of having a ‘father’
and encouraging conception through male–female
sexual intercourse, which was very offensive to the
couple. The emphasis on biology and genetic links was
seen to be more important than the parenting relationship.
This experience demonstrates howlesbians receive overt or subtle messages that their relationships
are substandard, inferior and unnatural.
Natalie gave another example of heteronormativity,
again in an interview with a social worker assessing her
suitability to adopt her own child. Natalie was not the
legal guardian at this time because she was not the
birth mother: ‘She asked us the most inappropriate
questions ... we felt like she was kind of, almost looking
for something that wasn’t there’ (Natalie).
Devaluing of the couple included inappropriate
questions and suggestions by the healthcare professionals
which participants were then forced to defend
and justify. The possible consequences of challenging
this heteronormative treatment could affect their
chances of beginning fertility treatment, conceiving
or adopting a child.
Heteronormativity was also apparent within the
hospital setting. Laura, a birth mother, described
feeling that she was devalued and not fully accepted
as a mother post-birth, at a time when both she and
her partner should have been receiving optimum care
and support:
At the hospital people were fine but abrupt. You know,
they were kind of like, ‘OK, what are you doing with a
baby? Oh. OK, all right then.’
(Laura)
For the participants who had reported negative or
harmful experiences of contact with healthcare professionals,
not acknowledging their partner or lesbian
status was found to be very unhelpful. This was a
denial of their sexuality and their identity, and ultimately
devalued the essence of their coupledom. This
was apparent in Lila’s recollection of her contact with
a doctor:
I said, [name of] my partner, but she’s not here, and
there’s just a blank, there’s just a blank and it’s nonexistent.
(Lila)
This type of response acted as a stressor for the couple
at a time when they were at their most vulnerable and,
at times, powerless.
Power
Despite the poor treatment that Lila was subjected to,
and a lack of acknowledgement of her partner, she was
unable to call this to the healthcare professional’s
attention. This was because she was struggling with
her child being ill and needed to prioritise the ‘fight’ to
focus on her child’s health. The power imbalance
meant that some participants were unable to voice
concerns about their treatment and the power thatwas
held over their reproductive opportunities. Thus they were effectively silenced. Laura, too, acknowledged
this power dynamic:
But it was just because [nurses] had so much power over
our lives that really mattered. You know right down to
whether we even conceived or whether we are allowed in
the programme.
(Laura)
Laura’s difficulties related to the nurses who were
‘awful’ in their treatment and care of her and her
partner; their relationship was not respected. Laura
also encountered homophobic attitudes from a social
worker who was assessing them for fertility assistance
at a clinic that they were hoping to use. Laura stated
that, for her, the balance of power led her to acquiesce
to poor treatment so as not to upset the process they
were trying to navigate:
And we just had to ride with that because if I’d fought
against it, she had too much power in the situation.
(Laura)
The sense that Laura and her partner were not ‘doing
things properly’ according to the heteronormative
world view added to a feeling of perpetual marginalisation,
placing undue stress on the relationship:
She [the social worker] was derogatory in ... just this sort
of attitude ... that I was a lesbian mum. It was kind of like I
wasn’t doing things properly ... it was kind of like we were
odd, but we were then more odd.
(Lila)
The process that Laura was navigating at the time
included invasive procedures, as well as reliance on
nurses for clear and honest information, which she
was not given. The added pressure for some participants
related to the feeling of undergoing constant
scrutiny and judgement by the heterosexual community,
and particularly by healthcare professionals.
The full disclosure
According to Rose, ‘We just have to go with the full
disclosure.’ For her, healthcare professionals’ assumptions
of heterosexuality meant having to be ‘quite up
front.’ The emphasis on ‘having to’ suggests the
inevitability of what Rose must do to ensure the care
of her family. The assumption of heterosexuality is
never more apparent than when a child is involved.
The participants had to stipulate and clarify their
relationship to their own child, with biology being a
specific part of their disclosure process. Most of them
adopted an upfront approach as a way of reclaiming
their personal power within a disempowering healthcare
system:
When we take our children to the doctor, we’re just really
up front – this is [name of child] and he’s got two mums
and [partner] gave birth.
(Alex)
There’s still that thing though, that you always have to
come out. It’s painful and boring.
(Leah)
A common thread in the findings was the emotional
energy required to constantly come out or remain
closeted. These experiences consistently undermined
couples, their relationship, and their relationship to
their child. Alex described how the heteronormative
responses desexualised their relationship when healthcare
professionals assumed that just one member of
the couple was the child’s parentwhen the couple were
of the same sex. Lila referred to being ‘eunuchified’,
saying ‘people turn you into a eunuch. They desexualise
your relationship.’ This was reported by other
participants, who stated that members of the public
and healthcare professionals assumed that the woman’s
partner was a friend, an aunt, a sister or, in one case,
the ‘nanny.’
And I think [doctor] kind of looked at us like ‘What are
you both doing sitting here, why are you both answering
those questions?’
(Alex)
Alex’s experience also reflected another aspect of her
contact with this doctor, the coming out experience.
As she explained, the monotony of coming out frequently
led her to feel that this was not necessary, yet
without disclosure the relationship with the doctor
would be compromised. There was also the potential
for tension between the couple with regard to their
biological parentage status and one parent being favoured
over the other by healthcare professionals.
In summary, lesbians experience institutional
heteronormativity and homophobia in their contact
with healthcare professionals who devalue their couple
relationship. Through attempting to acquire allies,
lesbians aimed to protect themselves and their family
when they had to constantly fully disclose their family
structure. Power was found to be an important factor
in lesbians’ experiences of healthcare.
Discussion
Participants with babies and children under 6 years
old generally reported positive experiences of care
during the transition to parenthood. The three participants
who experienced overt homophobia had
older children, ranging from 6 years to early teens.
This suggests that there have been improvements in healthcare professionals’ attitudes in recent years. Lee
et al (2011) examined the negative experiences in
maternity care of eight lesbian women. They noted
that changes in societal attitudes in the UK meant that
the women in their study had been generally treated in
a positive manner. None of the women experienced
explicitly homophobic views or inappropriate questioning.
In contrast, earlier research described overt
homophobia in maternity care (Wilton and Kaufmann,
2001). However, Ro¨ndahl et al (2009) found that
negative experiences in maternity care were more
likely to be related to personality clashes than to
homophobia.
Our participants reported that, because of the
homophobia within healthcare settings, they deliberately
sought out healthcare professionals who would
be responsive to their needs, either through their
personal navigation of the system or on the recommendation
of other lesbian couples. This purposeful
seeking was an attempt to find and secure the
involvement of healthcare professionalswho were able
to easily put to one side their heteronormative assumptions
and focus on being respectful and supportive
of the lesbian couple’s relationship and sexual
orientation. St Pierre (2012) found that lesbians used
referrals from others to avoid unsuitable practitioners,
and stated that lesbians assessed their safety in the
healthcare environment before revealing their sexual
orientation to healthcare providers. However, facilitating
disclosure is only the first step towards acceptable
care for couples in the transition to parenthood
(Chapman et al, 2012). Although the participants
deemed it monotonous to keep coming out, couples
who disclosed their relationship to others outside of
their family experienced increased satisfaction within
their couple relationships (Frost and Meyer, 2009;
Knoble and Linville, 2012).
Our findings highlighted the power differentials
between the healthcare professional and the couple.
The participants pointed out that they were often
unable to raise their concerns about poor treatment
due to heteronormativity within the healthcare environment.
The fear of judgement and subsequent
invisibility was a consequence of not explicitly stating
their sexual orientation. Goldberg et al (2009) recommend
that health professionals should orientate
themselves to resist the heteronormative world view
which they take for granted, and change their practice
to create inclusive and queer spaces for lesbian
parents.
Two of the three participants who used the services
of a fertility clinic to conceive had experienced problems
with healthcare professionals. Both of these
women felt discriminated against or judged, during
their process of becoming parents, by both nurses and
social workers. Fertility clinics may not currently
validate the importance of lesbians’ sexual orientation when accessing their services (Yager et al, 2010). The
healthcare professional is in a powerful position of
authority to approve couples as prospective parents.
The compulsory pre-insemination counselling that
partners have to undergo in the clinic can be difficult
and feel insulting when the interviewing social worker
is misinformed or holds negative opinions about the
nature of lesbian relationships. Feeling comfortable
with healthcare professionals during interactions is
extremely important (Harbin et al, 2012). Lesbians
want to ensure that practitioners recognise their right
to be parents and that they will provide them with
good care.
The participants reported a focus on the biological
aspects of conception, which queer theory challenges.
This illustrates an overarching ideology that emphasises
the interplay of gender and biology within the
heteronormative assumptions about conception. The
suggestion by one social worker in the pre-counselling
phase that a participant should go to a pub and find
‘a father to sleep with’ is an example of biologism,
viewing life from a biological perspective, which
resonates with debates about lesbian women having
children. These largely revolve around heteronormative
assumptions about fatherhood (Short, 2007). Anxiety
about the lack of a father is associated with the
emphasis on the perceived heterosexual family’s
superiority and the presence of a male figure in the
family structure, thus undermining the lesbian-led
family (Goldberg, 2010a).
All of the couples in our study wished to be the
primary caregivers for their child(ren). Dempsey
(2010) found that partnered lesbian couples prefer
to keep their reproductive relationship with the donor
separate to their own couple relationship. Our participants
described how experiences of healthcare
professionals’ failure to recognise the non-biological
mother as a true parent to the child could lead to
feelings of insecurity in their role and the need for
reassurance from their partner. Healthcare professionals
need to have an awareness of the changing
structures of families and of how they may, often
unwittingly, perpetuate the social stigma that can
have a negative impact on the lesbian couple.
A recent study in the UK found that non-biological
mothers felt respected by staff and regarded their
treatment positively, despite structures, language
and practice environments which were predominantly
heteronormative (Cherguit et al, 2013). Goldberg
(2010b) argued that a non-biological mother’s role
is not easily defined, nor is it recognised within society.
According to Ben-Ari and Livni (2006), nonbiological
mothers are not necessarily regarded as
mothers at all. This failure to recognise the nonbiological
mother has implications for coping with
feelings of displacement and the lack of a clear role.
Healthcare professionals are in a position to help couples by accepting and acknowledging their coupledom.
Queer theory offers an alternative lens to deemphasise
the dominant heteronormative focus on
sex and gender (Walters, 2005). For example, the
exploration by Abes and Kasch (2007) of the multiple
dimensions of identity in lesbian university students,
and the study by Eves (2004) of butch/femme identity,
have both highlighted the role that queer theory can
play in examining queer identity and subsequent
challenges to heteronormative environments. In our
study, queer theory facilitated insight into the lesbian
couple’s journey through the health system and the
responses of the healthcare professionals whom they
encountered.
Strengths and weaknesses of the
study
The qualitative research design allowed the generation
of rich data. The use of queer theory was relevant
in examining issues of power within the healthcare
context and in deconstructing the emphasis on
biologism in healthcare settings. It allowed the lesbian
relationship to be viewed without the constraints of
gender, and therefore enabled openness in interpretation.
Queer theory also facilitated critical interpretation
of the findings and consideration of the impact
of heteronormativity on the participants’ relationships.
The small number of participants and the homogeneity
of their ethnic identity could be regarded as a
weakness. All of the participants had received tertiary
level education, and at least one partner in each couple
was in paid employment. Lesbian women in lower
socio-economic groups were not represented. However,
the findings show that lesbian women continue
to experience marginalisation and invisibility which
would not necessarily be expected to differ as a function
of demographic characteristics.
Implications of the study
This research has implications for lesbian couples who
are considering parenthood and seeking an understanding
of some of the barriers they may face within
antenatal and healthcare services, including fertility
clinics. It also has implications for professionals,
including nurses, midwives and physicians, and allied
health professionals who work in fields of familyrelated
care and reproductive health. Further research
is recommended to explore the tenacity and resilience
of lesbian couples during the transition to parenthood
in the spectrum of healthcare environments for pregnancy,
birthing and postnatal care.
Specific recommendations
Healthcare professionals need to recognise and understand
the roles of both women in the lesbian-led
family. Lesbian-led families are valid, important and
diverse, and are not shaped by biological links to one
another. Inherent in achieving this is the need for
professional preparation, at both undergraduate and
postgraduate levels, to meet the needs of lesbian
couples and their children.
Creating a suitable clinical environment for the
disclosure of sexual orientation is important. This
includes consideration of the impact of language
needs, for example, naming of the non-biological
mother and the use of gender-neutral terms. An
inclusive approach is required in both verbal communication
and documentation.
Human rights and anti-discrimination policies
need to be emphasised within clinical practice environments.
Conclusion
This paper has reported lesbian women’s experiences
of dealing with healthcare professionals while transitioning
into parenthood. To our knowledge this is the
first study to have included an exploration of the
effects that healthcare professionals can have on the
couple. The focus on healthcare professionals is also
timely, given recent changes in family formation, and
could be relevant to a range of other health settings,
given that lesbian-led families are increasing in numbers.
Healthcare professionals still appear to lack knowledge
and awareness of the lesbian-led family as a
legitimate family structure. They need to be aware of
factors that affect the lesbian-led family in relation to
the transition to parenthood. By acknowledging the
lesbian couple and paying attention to the dominance
of the biological emphasis, power dynamics, the
influence of gender and heteronormative assumptions,
healthcare professionals can have a positive
impact on lesbian couples’ relationship and on the
lesbian-led family as a whole.
ACKNOWLEDGEMENTS
The first year of this Masters study was funded
through Te Pou, the National Centre for Mental
Health Research in New Zealand, as part of Kristal
O’Neill (Roache)’s participation in the Clinical Leadership
programme.
CONFLICTS OF INTEREST
None.
References
- Abes ES and Kasch D (2007) Using queer theory to explore lesbian college studentsÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ multiple dimensions of identity. Journal of College Student Development 48: 619ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â36.
- Almack K (2008) Women parenting together: a reflexive account of the ways in which the researcherÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s identity and experiences may impact on the processes of doing research. Sociological Research Online 13:4ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â10.
- Beagan BL, Fredericks E and Goldberg L (2012) NursesÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ work with LGBTQ patients: ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âTheyÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢re just like everybody else, so whatÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s the difference?ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ Canadian Journal of Nursing Research 44:44ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â63.
- Ben-Ari A and Livni T (2006) Motherhood is not a given thing: experiences and constructed meanings of biological and nonbiological lesbian mothers. Sex Roles 54:521ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â31.
- Bos H and van Balen F (2010) Children of the new reproductive technologies: social and genetic parenthood. Patient Education and Counseling 81:429ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â35.
- Bos H, van Balen F and van den Boom D (2007) Child adjustment and parenting in planned lesbian-parent families. American Journal of Orthopsychiatry 77:38ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â48.
- Buchholz SE (2000) Experiences of lesbian couples during childbirth. Nursing Outlook 48:307ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â11.
- Butler J (1990) Gender Trouble: feminism and the subversion of identity. New York: Routledge.
- Chapman R, Wardrop J, Zappia T et al (2012) The experiences of Australian lesbian couples becoming parents: deciding, searching and birthing. Journal of Clinical Nursing 21:1878ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â85.
- Cherguit J, Burns J, Pettle S et al (2013) Lesbian co-mothersÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ experiences of maternity healthcare services. Journal of Advanced Nursing 69:1269ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â78.
- Cochran SD and Mays VM (2009) Burden of psychiatric morbidity among lesbian, gay, and bisexual individuals in the California Quality of Life Survey. Journal of Abnormal Psychology 118:647ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â58.
- Cochran SD, Sullivan JG and MaysVM(2003) Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of Consulting and Clinical Psychology 71:53ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â61.
- De Lauretis T (1991) Queer Theory: lesbian and gay sexualities. Bloomington, IN: Indiana University Press.
- Dempsey D (2010) Conceiving and negotiating reproductive relationships: lesbian and gay men forming families with children. Sociology 44:1145ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â62.
- Eves A (2004) Queer theory, butch/femme identities and lesbian space. Sexualities 7:480ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â96.
- Folgero T (2008) Queer nuclear families? Reproducing and transgressing heternormativity. Journal of Homosexuality 54:124ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â49.
- Frost DM and Meyer IH (2009) Internalized homophobia and relationship quality among lesbians, gay men, and bisexuals. Journal of Counseling Psychology 56:97ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â109.
- Goldberg A (2010a) Lesbians and gay men as parents. In: Lesbian and Gay Parents and Their Children: research on the family life cycle. Washington, DC: American Psychological Association. pp. 89ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â124.
- Goldberg A (2010b) From partners to parents: the transition to parenthood for lesbians and gay men. In: Lesbian and Gay Parents and Their Children: research on the family life cycle. Washington, DC: American Psychological Association. pp. 49ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â88.
- GoldbergAandSayerA(2006) Lesbian couplesÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ relationship quality across the transition to parenthood. Journal of Marriage and Family 68:87ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â100.
- Goldberg L, Ryan A and Sawchyn J (2009) Feminist and queer phenomenology: a framework for perinatal nursing practice, research and education for advancing lesbian health. Health Care for Women International 30:536ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â49.
- Goldberg W (1988) Introduction: perspectives on the transition to parenthood. In: Michaels GY and Goldberg WA (eds) The Transition to Parenthood: current theory and research. Cambridge, UK: Cambridge University Press. pp. 1ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â20.
- Golding AC (2006) Redefining the nuclear family: an exploration of resiliency in lesbian parents. In: ProutyLyness AM (ed.) Lesbian FamiliesÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ Challenges and Means of Resilience: implications for feminist family therapy. New York: The Haworth Press. pp. 35ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â66.
- Golombok S (2000) Parenting: what really counts? Hove, UK: Routledge.
- Harbin A, Beagan B and Goldberg L (2012) Discomfort, judgement, and health care for queers. Journal of Bioethical Inquiry 9:149ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â60.
- Henderson L (2003) Queer theory, new millennium. Journal of Homosexuality 45:375ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Jagose A (1996) Queer Theory: an introduction. New York: New York University Press.
- James T and Platzer H (1999) Ethical considerations in qualitative research with vulnerable groups: exploring lesbiansÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ and gay menÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s experiences of health care ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â a personal perspective. Nursing Ethics 6:73ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â81.
- Jootun D, McGhee G and Marland GR (2009) Reflexivity: promoting rigour in qualitative research. Nursing Standard 23:42ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Katz-Wise SL, Priess HA and Hyde JS (2010) Gender-role attitudes and behaviour across the transition to parenthood. Developmental Psychology 46:18ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â28.
- Kertzner RM, Meyer IH, Frost DM et al (2009) Social and psychological well-being in lesbians, gay men, and bisexuals: the effects of race, gender, age, and sexual identity. American Journal of Orthopsychiatry 79:500ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â10.
- King M, Semlyen J, Tai SS et al (2008) A systematic review of mental disorder, suicide, and deliberate self-harm in lesbian, gay and bisexual people. BMCPsychiatry 8:70ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â87.
- Knoble NB and Linville D (2012) Outness and relationship satisfaction in same-gender couples. Journal of Marital and Family Therapy 38:330ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â39.
- Kurdek LA (2008) Change in relationship quality for partners from lesbian, gay male, and heterosexual couples. Journal of Family Psychology 22:701ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â11.
- Lee E, Taylor J and Raitt F (2011) ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âItÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s not me, itÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s themÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢: How lesbian women make sense of negative experiences of maternity care: a hermeneutic study. Journal of Advanced Nursing 67:982ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â90.
- LeMasters EE (1957) Parenthood as crisis. Marriage and Family Living 19:352ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â5.
- Lewis RJ, Derlega VJ, Clarke EG et al (2006) Stigma consciousness, social constraints, and lesbian well-being. Journal of Counseling Psychology 53:48ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â56.
- Lloyd M (2007) Judith Butler: from norms to politics. Cambridge, UK: Polity Press.
- Lovaas KE, Elia JP and Yep GA (2006) Shifting ground(s): surveying the contested terrain of LGBT studies and queer theory. In: Lovaas KE, Elia JP and Yep GA (eds) LGBT Studies and Queer Theory: new conflicts, collaborations, and contested terrains. New York: The Haworth Press, Inc. pp. 1ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â18.
- Lovelock K (2010) Conceiving reproduction: new reproductive technologies and the redefinition of the kinship narrative in New Zealand society. Anthropological Forum 20:125ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â46.
- McDonald J (2013) Coming out in the field: a queer reflexive account of shifting researcher identity. Management Learning 44:127ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â43.
- Markus EB, Weingarten A, Duplessi Y et al (2010) Lesbian couples seeking pregnancy with donor insemination. Journal of Midwifery & WomenÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s Health 55:124ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â32.
- Meyer IH (2003) Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin 129: 674ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â97.
- Meyer IH, Dietrich J and Schwartz S (2007) Lifetime prevalence of mental disorders and suicide attempts in diverse lesbian, gay, and bisexual populations. American Journal of Public Health 98:1004ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Minton HL (1997) Queer theory: historical roots and implications for psychology. Theory and Psychology 7: 337ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â53.
- Mohr JJ and Daly CA (2008) Sexual minority stress and changes in relationship quality in same-sex couples. Journal of Social and Personal Relationships 25:989ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â1007.
- OÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢Neill KR, HamerHPand Dixon R (2012) ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âA lesbian family in a straight worldÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢: the impact of the transition to parenthood on couple relationships in planned lesbian families. WomenÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s Studies Journal 26:39ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â53.
- RoÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâèndahl G, Bruhner E and Lindhe J (2009) Heteronormative communication with lesbian families in antenatal care, childbirth and postnatal care. Journal of Advanced Nursing 65:2337ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â44.
- Ryan M and Berkowitz D (2009) Constructing gay and lesbian parent families ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âbeyond the closet.ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ Qualitative Sociology 32:153ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â72.
- St Pierre M (2012) Under what conditions do lesbians disclose their sexual orientation to primary healthcare providers? A review of the literature. Journal of Lesbian Studies 16:199ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â219.
- Sedgwick EK (2008) Epistemology of the Closet, revised edn. Berkeley, CA: University of California Press.
- Short L (2007) ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âIt makes the world of differenceÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢: benefits for children of lesbian parents of having their parents legally recognised as their parents. Gay and Lesbian Issues and Psychology 3:5ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â15.
- Stacey J and Biblarz TJ (2001) (How) does the sexual orientation of parents matter? American Sociological Review 66:159ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â83.
- Steele LS, Ross LE, Epstein R et al (2008) Correlates of mental health service use among lesbian, gay, and bisexual mothers and prospective mothers. Women and Health 47:95ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â112.
- Thomas DR (2006) A general inductive approach for analysing qualitative evaluation data. American Journal of Evaluation 27:237ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â46.
- Vanfraussen K, Ponjaert-Kristoffersen I and Brewaeys A (2003) Family functioning in lesbian families created by donor insemination. American Journal of Orthopsychiatry 73:78ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â90.
- Walters SD (2005) From here to queer: radical feminism, postmodernism, and the lesbian menace. In: Morland I and Willox A (eds) Queer Theory. Basingstoke: Palgrave Macmillan. pp. 6ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â21.
- Warner M (1993) Fear of a Queer Planet: queer politics and social theory. Minneapolis, MN: University of Minnesota Press.
- Watson K (2005) Queer theory. Group Analysis 38:67ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â81.
- Watts JH (2008) Integrity in qualitative research. In: Given LM (ed.) The Sage Encyclopaedia of Qualitative Research Methods. Thousand Oaks, CA: Sage Publications. pp. 440ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 41.
- Weber GN (2008) Using to numb the pain: substance use and abuse among lesbian, gay, and bisexual individuals. Journal of Mental Health Counseling 30:31ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â48.
- Wilton T and Kaufmann T (2001) Lesbian mothersÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ experiences of maternity care in the UK. Midwifery 17:203ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â11.
- Yager C, Brennan D, Steele LS et al (2010) Challenges and mental health experiences of lesbian and bisexual women who are trying to conceive. Health & Social Work 35:191ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 200.