Keywords
Obesity; Gastrointestinal system; Child obesity; Leptin; Diet
Generalities
Contextualization of obesity
Obesity is one of the most serious problems of the 21st century and today there is a record that about 2.1 billion people almost 30% of the world population are obese or overweight. The rise in obesity rates worldwide over the last three decades has been substantial and widespread, presenting a public health epidemic in both developed and developing countries [1].
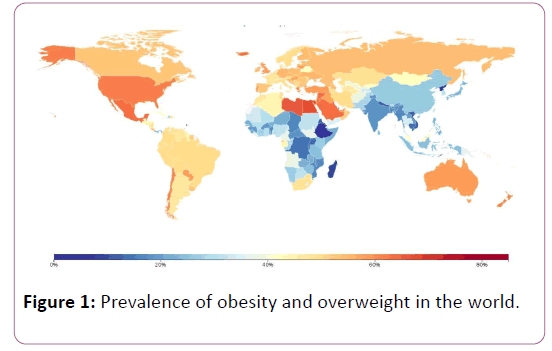
A systematic analysis of the Global Burden of Disease studies 2013 revealed that in Over the course of the study, overweight and obesity rates among adults have increased for both men (from 29% to 37%) and women (from 30% to 38%). In developed countries, men had higher rates of overweight and obesity, while women in developing countries showed higher rates, and in developed countries, the peak of obesity rates is moving at an earlier age presented in the following map (Figure 1) [2].
Figure 1: Prevalence of obesity and overweight in the world.
An important cause in the development of this disease is the increasing availability of foods rich in calories and High Fat Diet (HFD), supported by lack of physical activity to increase energy expenditure. Overweight and obesity significantly increase the risk of chronic non-communicable, premature mortality and the social cost of health. It is estimated that 90% of cases of type 2 diabetes mellitus are attributed to overweight and obesity. A child is considered obese when it exceeds 20% of its ideal weight, this problem not only triggers physical complications but also psychological.
More alarming is the fact that there is a strong correlation between the development of childhood obesity and its prevalence in adulthood. Likewise, children who do not present this disease have a high probability of staying within normal weight in adulthood [3]. Therefore, children who have an early obesity predispose a prevalence of this condition during adult stages.
Pharmacological Treatment
Obesity should be treated ideally with exercise and diet [4]. Indeed, the use of diets to control body weight in the long term makes the vast majority of overweight or obese individuals have to modify their type of diet to reduce daily energy intake.
However, very low-calorie diets (VLCD, fewer than 800 kcal per day) or hypocaloric diets should not be used routinely. This should only be contemplated as part of a multicomponent strategy with specialist clinical support, where there is a need for rapid weight loss (such as prior to surgery). They should not be undertaken for more than 12 weeks [5]. VLCDs may not be nutritionally complete and provide far fewer calories than most people need to maintain a healthy weight. In addition, VLCDs may not be nutritionally complete and provide far fewer calories than most people need to maintain a healthy weight. It is not an easy diet to follow. Apart from feeling hungry and low on energy, other side effects can include: dry mouth, constipation or diarrhea, headache, dizziness, cramps, hair thinning
While VLCDs can lead to short-term weight loss, most people tend to put the weight back on gradually after coming off the diet.
Therefore VLCDs are not a long-term weight management strategy and should only be used as part of a wider weight management plan.
Thus, it has been sought to promote the development of several pharmacological treatments to treat this disease. However, despite the discovery of the genetic basis of obesity [6] and the discovery of more than a dozen of hormones and peptides that regulate appetite, the obesity epidemic has not yet been halted [7].
Anti-obesity drugs developed so far
The Food and Drug Administration (FDA) in the United States has approved five long-term obesity drugs so far: Lorcaserin (Belviq®), Phentermine/Topiramate (Qsymia®), Naltrexone/ Bupropion (Contrave®), Liraglutide (Saxenda®) and Orlistat (Xenical®) for the long-term treatment of obesity. Medications like these can be used in combination with diet and exercise to help people lose weight [8].
However, two of these drugs (phentermine/topiramate and lorcaserin) did not obtain approval in Europe, due to safety concerns [9].
Medications approved for long-term obesity treatment, when used as an adjunct to lifestyle intervention, lead to greater mean weight loss and an increased likelihood of achieving clinicallymeaningful 1-year weight loss relative to placebo. Weight loss ≥ 5% is generally considered to be clinically meaningful [10]. Orlistat and Lorcaserine at 9% of the higher dose (15/92 mg) Phentermine plus prolonged release Topiramate at 1 year. The proportion of patients achieving at least 5% of clinically significant weight loss ranges from 37% to 47% for Lorcaserin, 35% to 73% for Orlistat, and 67% to 70% for the higher dose Of Phentermine plus extended release Topiramate. All medications produce greater improvements in many cardio metabolic risk factors than placebo. There are many other medications, but not approved for long-term use [11].
The Intestine-Brain Axis
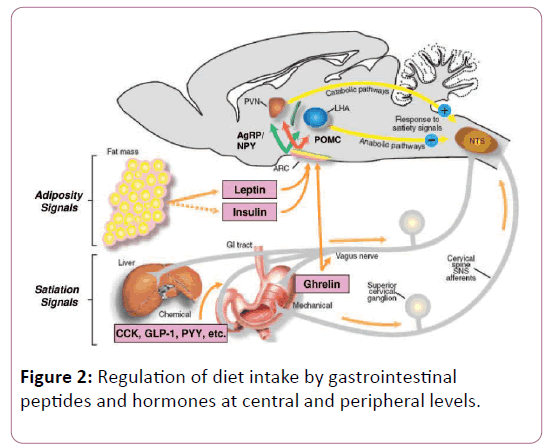
Figure 2 [12,13] shows how the signals that stimulate responses in the regulation of intake in the brain come from the digestive organs and adipose tissue; which are short-term indicators of the nutritional status (with the exception of leptin).
Figure 2: Regulation of diet intake by gastrointestinal peptides and hormones at central and peripheral levels.
Such peripheral signals may be nerve impulses of the vague nerve induced by a series of hormonal peptides secreted and generated just before and after meals (Table 1).
| Hormone |
Synthesis Site |
Main effects |
Developed drugs |
| They act in the CNS (ARC) of the hypothalamus |
| GIP |
K-cells of the duodenum and jejunum |
Incretin effect on insulin secretion; Increases the synthesis of fatty acids in adipose tissue; Effects on food intake: unknown |
|
| GLP-1: peptide like glucagon 1 |
Intestinal L cells |
Incretin effect on insulin secretion; Suppresses the release of glucagon; Inhibits gastric emptying; Inhibits gastric secretion; Inhibits energy intake |
Natural analog of GLP-1 4-exendin. Approved for the treatment of type 2 diabetes. Liraglutide (Novo Nordisk) this drug has been approved for use in diabetes |
| Oxyntomodulin (OXM) |
L-cells of the distal intestine; Post-prandial release after food intake
Stimulated by the presence of fatty acids |
Inhibits the production of gastric acid; Reduces gastric motility; Inhibits food intake; Decreased plasma levels of Ghrelin |
|
| PYY (1-36) |
Synthesized by L-type enteroendocrine cells, mainly in the distal intestine. The main circulating form of this hormone is PYY (3-36), which is formed from the partial rupture of PYY (1-36) by means of the enzyme dipeptidyl peptidase IV |
Inhibits food intake; Inhibits the secretion of the gallbladder; Reduces intestinal motility; Inhibits pancreatic secretion. |
In humans it has been shown that the application of an intravenous infusion (I.V) of PYY (3-36), decreases the food intake in a dose-dependent manner with a maximum inhibition of 35%; P <0.001 vs. control) Withdrawn in 2005 adverse effect dose-dependent nausea, which would not be a useful therapeutic strategy. |
| Act at the peripheral level (NTS) |
| Pancreatic Polypeptide (PP) |
Secreted in the pancreas and in a smaller amount, by the colon |
Relaxation of the gallbladder; Inhibition of exocrine pancreatic secretion; Inhibits food intake (inducing peripheral satiety) |
Synthetic analog of PPTM30339 showed in the preclinical studies a weight loss in mice that had diet-induced obesity and is now in clinical phase II studies |
| Amylin |
It is co-released with insulin into β-pancreatic cells after ingestion. The main sites of action are located in the brain stem and in the postrema area, where it presents central anorectic functions |
Regulation of the motor activity of the stomach; Maintenance of carbohydrate homeostasis; Amylin works together with insulin to regulate postprandial glucose levels. |
Recently the pharmaceutical company Amylin Pharmaceuticals developed a synthetic analog called pramlintide. It is under investigation as a potential anti-obesity drug |
| Acts at the peripheral level (NTS) |
Ghrelin
(Induce hunger) |
Gastric background cells A; Small and large intestine |
Promotes the release of GH and other hormones into the pituitary; Increases food intake; Promotes gastric motility; Promotes the release of PP |
|
Table 1: Gastrointestinal hormonal peptides that control appetite.
The hypothalamus and its role in controlling appetite
In the upper part the inside of the hypothalamus where we find the arcuate or arcuate nucleus (ARC) that is located at the base of the hypothalamus and has been established inside the neuronal circuit that acts as the main site of integration of the Signals from gastrointestinal peptides (ghrelin) and humoral factors (e.g. leptin and insulin). It shows how there are mainly two groups of neurons associated with appetite or with induction of satiety. Each substance that enters into circulating form can modify the activity of these two populations of neurons within the ARC. A population co-expresses CART (cocaine-amphetamine-related transcriptase) and proopiomelanocortin (POMC), precursor of the α-MSH (melanocyte-stimulating hormone) neuropeptide which has an appetite (or anorexigenic).
A second population of neurons co-expresses the neuropeptide-Y and the r-Agouti protein (AgRP) and their activation increases food intake (orexigenic effect). In the case of POMC, α-MSH binds to melanocortin MC3 and MC4 receptors. The importance of the melanocortin system stems from the fact that less than 6% of monkey obesity in humans has been observed to result from a defect in the MC4 receptor.
Humoral factors from adipose tissue or adiposity signals, leptin and insulin, are mostly involved in the long-term regulation of food intake and energy metabolism as dictated by energy needs and the amount of energy stores, and can act on both cell types simultaneously to produce satiety through appetite suppression or hunger when the body is in a negative energy state (hungry) [14,15].
In addition, endocrine signals bring information regarding the availability of energy and are integrated with signals of the brain centers (e.g. gratification, stress or motivational) to regulate appetite and energy expenditure.
Gastrointestinal tract are mostly short-term meal-related signals affecting the daily intake. Indeed, it secretes several peptide hormones that participate in the control of feeding behavior.
The release of these peptides is controlled by energy status and nutrients. In addition to food intake, gastrointestinal peptides control digestion and gastrointestinal motility. Meal ingestion results in gastric distension and production of peptide hormones by enteroendocrine cells, both of which can promote a feeling of fullness/satiety, and a desire to stop eating. Satiety per se limits the duration of the meal or the "meal size". Such termination is stimulated by circulating levels of glucose, amino acids (a.a) and lipids, which are detected by the brain or through peripheral receptors.
The main areas of the brain that coordinate the homeostatic regulation of energy and body weight are the hypothalamus and brainstem. Once food is consumed, vagal afferent pathways are activated by nutrient sensitive chemoreceptors and receptors for locally released intestinal hormones.
Satiety per se is involved in regulating the frequency of food. Thus, it prevents overconsumption during meals and occurs at the gastrointestinal (GI) level in multiple sites (stomach, proximal small intestine, colon, and pancreas) and the food evokes the feeling of satiety by two main effects in the gastrointestinal tract: Gastric distension and peptide release from entero-endocrine cells.
The brain stem is the main center and receives input inputs from satiety signals that act in the short term and are transmitted neural (projections to the vague nerve that reach the nucleus of the solitary tract or NTS). These peptides transmit "satiety" signals because they promote the termination of the food that is in progress and do not delay the subsequent initiation of the food and affect the food intake if it is released between meals [12].
Signs of satiety that reach the hypothalamus
At the intestinal level, we have a series of visceral responses from which hormonal peptides such as cholecystokinin or CCK are released, which is secreted in the small intestine and projects chemical signals at the peripheral level when foods rich in fats and proteins are consumed. Peripheral CCK induces satiety via the gastric receptors retransmitting the effect in the vagal afferent pathways to achieve such signaling to the hypothalamus; via NTS and the postrema area (AP).
The hormones released from the intestine have satietyinducing type actions, such as the hormones OXM and PYY that are released from the TGI in the lower part and the PP that is released from the islets of Langerhans. GLP-1, GIP, and OXM are incretin type (improving insulin sensitivity and reducing food intake) such hormones improve the pancreas's response to absorbed nutrients. GLP-1 and OXM also reduce food intake and induce satiety. Ghrelin is the only hormone at the gastrointestinal level that stimulates food intake (orexigenic) and this action increases as it is in a fasting state. In addition to releasing the AgRP/NPY neuropeptides and mediating the orexigenic effect in the lateral hypothalamus (LHA) (Table 1) [16].
Adipostatic signs that reach the hypothalamus: Leptin
Leptin [17] is a hormone of 146 a.a and whose name comes from the Greek "leptos" which means thin. It is the product of the OB gene, secreted by adipose tissue, and regulates both food intake and energy balance in normal weight subjects. When exogenous leptin was injected into rodents with genetic obesity [18] or diet-induced [19], body weight and adiposity decreased, improve metabolic control by central regulation or using peripheral effector pathways.
Leptin may act directly on the NTS, AP, or dorsal motor nucleus of the vague nerve and even influence the response of CCK [20], or finally induces satiety through the activation of POMC neurons in the VMH [12].
It has been observed that the serum concentrations of this hormone correlate positively with the mass of adipose tissue. Although leptin is a circulating signal that reduces appetite primarily by central action [21], obese subjects generally has unusually high levels of circulating leptin and thus, resistance to this hormone develops [22].
Leptin is not only secreted in the placenta and adipose tissue, but also in the gut. Leptin mRNA and leptin have been detected in the main cells of the stomach mucosa and in the gastric fundus [23]. Leptin acts through its receptors. They are generally referred to as (OB-R). Thus these can be classified into three classes: short, long and soluble. The soluble form of the receptor (OB-Re) has a high affinity for leptin and is thought to regulate plasma concentrations of leptin as it mediates the transport of leptin to plasma and also through the blood-brain barrier. So this receptor modulates the biological activity of this hormone [24].
Mechanism of regulation of intake at the neuroendocrine level
Leptin, like serotonin and in the particular case Belviq®, exert control over the neuronal populations that control the appetite in the hypothalamus, specifically in the ARC [25]. Leptin also affects the lateral hypothalamus (LH), as in this area is a protein called the hormone melanin (MCH), which is a neuropeptide which induces food intake as it acts as a type signal Anabolic activity in energy regulation and increasing stress [26]. Leptin has been shown to inhibit the production of this hormone as an anorexigenic mechanism [27]. Leptin also reduces the levels of orexin, which is another peptide located in the same region and like MCH, induces hunger [28].
Hyperleptinemia
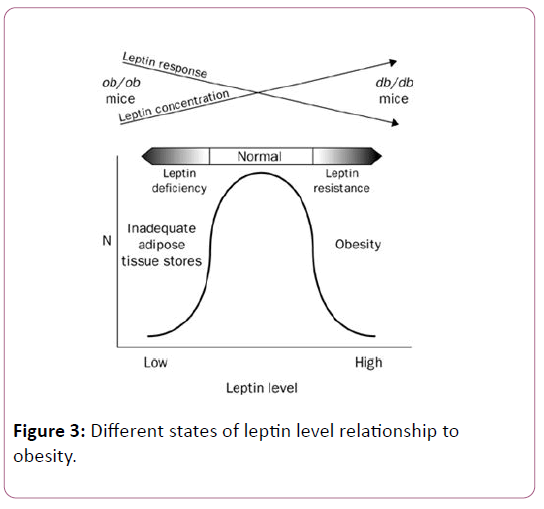
In animals it has been observed that in those where defects in the leptin signaling pathway are present, either because they produce no functional hormone (ob/ob mice) [29] or because they express defective forms (fa/fa rats) or that do not express their receptor (db/db mice), are characterized by hyperphagia and massive early-onset obesity, in addition to diabetes, hypothermia and infertility.
In humans, however, it is common for obese individuals to have the highest levels of circulating leptin, since they have more adipose tissue and develop resistance to the satiety effects of leptin, which is paradoxical since despite that obese subjects have elevated levels of leptin the supply of leptin does not produce a substantial loss of weight, which is attributable to the development of "leptin resistance". Their resistance could be due to defects in the system that transports it to the CNS or in the post-receptor transduction pathways of leptin (Figure 3) [30,31].
Figure 3: Different states of leptin level relationship to obesity.
What causes leptin resistance?
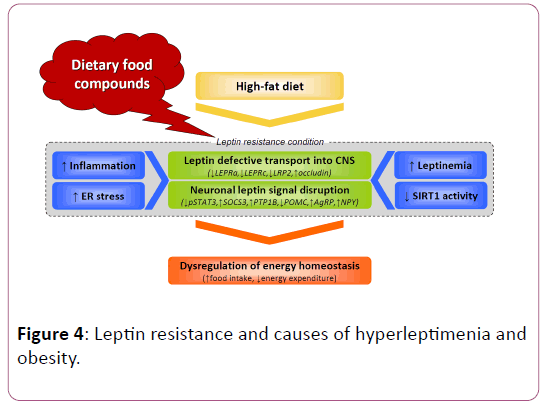
According to Stephan J Guyenet, PhD, who is a specialist in Obesity Neurobiology and creator of the Whole Health Source Web site, three causes of leptin resistance has been identified [32,33]:
• Inflammation: Inflammatory signaling in the hypothalamus is likely to be a significant cause of leptin resistance in animals and humans.
• Free fatty acids: Elevated levels of free fatty acids in the bloodstream can increase your metabolites in the brain and interfere with leptin signaling.
• Present high levels of Leptin: Having high levels of leptin seems to be the leading cause of leptin in the first place.
What science knows about reversing resistance to leptin
If one has a lot of body fat, especially in the abdominal area, then it is almost certainly a leptin-resistant case. Therefore, a key to reversing resistance to leptin is the reduction of dietinduced inflammation. There are several things you can do:
• Avoid processed foods: Highly processed foods can endanger the integrity of the intestine and lead to intestinal inflammation [34].
• Eating Soluble Fiber: Soluble fiber can help improve bowel health and may protect against obesity [35].
• Exercise: Physical activity can help reverse leptin resistance [36,37].
• Sleep: Lack of sleep has been implicated in problems with leptin [38].
• Lowering your triglyceride levels: Having high triglycerides in the blood can prevent the transport of leptin from the blood to the brain [39]. The best way to reduce triglycerides is to reduce your carbohydrate intake.
• Eat Protein: Eating lots of protein can cause automatic weight loss. There are many reasons for this; one of them may be the improvement in the sensitivity to leptin [40].
In general hyperleptinemia coexists with the loss of responsiveness to leptin in common obese conditions (Figure 4) [41]; we can see several mechanisms have been attributed to this loss of responsiveness to the hormone.
Figure 4: Leptin resistance and causes of hyperleptimenia and obesity.
Obesity treatment in children
The treatment of obesity in children is largely based on the same principles as adults by combining a controlled calorie diet with regular exercise.
It is important to encourage your children to increase their levels of physical activity and to make sure they continue to exercise regularly. Even if they do not lose weight immediately, there are many other health benefits that can be obtained from regular exercise, such as a lower risk of developing type-2 diabetes and cardiovascular disease.
Your child may be treated to a specialist in the treatment of childhood obesity if they develop an obesity-related complication, have a learning disability, or if an underlying medical condition is believed to be causing obesity. Treatment and support of children will be offered on the specific needs and requirements.
Use of medications for the treatment of obesity is generally not recommended for children under 12 years. Orlistat is only recommended for use in children in exceptional circumstances Currently, only one agent (orlistat) has FDA approval for the treatment of obesity among adolescents 12-16 years of age [42], for example if a child is severely obese and has an obesityrelated complication such as a problem with bones or joints or sleep apnea.
In cases where Orlistat is prescribed for the treatment of a child with obesity, the child will be closely monitored by a specialist pediatrician experienced in treating children with this specific medication and who is working as part of a multidisciplinary team.
Surgery is generally not recommended for the treatment of obese children or a young person unless there are exceptional circumstances, such as if a child is severely obese and as a result, has comorbidities related to obesity [43].
Biomarker that predisposes children and adolescents to adult obesity Childhood
Obesity is a serious medical condition associated with significant comorbidities during childhood and adulthood. When FDA approves a medication for a specific indication in adults, the minimum age for authorized use is usually set at age 16. No weight loss medications are approved for use in children less than 12 years.
Therefore the discovery of Leptin has been received with great expectation as a potential anti-obesity therapy due to its ability to reverse excess adiposity in animal models (rodents) characterized by a deficiency of the hormone, in fact, leptin reduces body weight dramatically, suppresses appetitive behaviors and improves other endocrine-sensitive and metabolic leptin abnormalities in children and adults with congenital hormone deficiency.
Open clinical trials in adults and pediatric patients with leptin deficiency due to congenital lipodystrophies also demonstrated long-term improvements in metabolism as well as placebocontrolled trials in leptin-deficient women with hypothalamic amenorrhea. However, studies conducted in non-deficient leptin adults have found relatively few effects on body weight limiting the utility of this hormone as an anti-obesity drug in those patients who do not have leptin insufficiency.
On the other hand, in adults who have undergone substantial weight reduction there is evidence suggesting that leptin treatment restore serum levels of this hormone to pre-weight loss values may reverse the subtle, neuroendocrine and autonomic muscle adaptations of individuals who reverts weight loss. There have been no trials of the effect of leptin on non- hormone deficient children during weight reduction or in a state of weight reduction [44].
Studies show that leptin and exogenously injected insulin cause a considerable reduction in intake, and leptin and insulin also have additive effects (synergism) when given concurrently. In fact, it has been observed that exogenous administration of Leptin in patients with congenital lipodystrophy or absence of focal or generalized adipose tissue and insulin resistance decreases insulin resistance, suppresses hepatic gluconeogenesis, improves hyperlipidemia and reverses hepatic steatosis or fatty liver.
Insulin concentrations correlate directly with body weight and, above all, with body adiposity [45]. Unlike leptin, plasma insulin concentrations reflect more acute alterations in energy metabolism, as well as body fat Leptin.
Leptin and its relationship with the development of the metabolic syndrome in obese children
Five characteristics generally accepted of the metabolic syndrome are: Hypertension, Hyperglycemia, Hypertriglyceridemia, Reduced high-density lipoprotein cholesterol (HDL-C) and abdominal obesity. Among children and adolescents, the metabolic syndrome is associated with the subsequent risk of type 2 diabetes mellitus and cardiovascular diseases in adulthood [46].
A recent and comprehensive study conducted on 120 with a body mass index (BMI) greater than the equivalent of 30 kg/m2 for an adult. To which they were assigned at random (N=60) a low-carbohydrate diet (L-CHO) or (n=60) a low-fat (L-F) for 2 months. Fifty-three (88.3%) subjects on a low-carbohydrate diet and 45 (75%) on a low-fat diet completed the study. Anthropometric measurements and leptin levels were measured before and after the intervention.
In this paper, fibroblast growth factor 21 (FGF21) is also mentioned. FGF21 is a product of liver and adipose tissue with important roles in food intake and energy expenditure [47]. FGF21 mediates the metabolic response to starvation [48]. FGF21 improves insulin sensitivity, decreases triglyceride concentrations, and improves Hyperglycemia and hyperlipidemia associated with obesity.
FGF 21 is proposed as a mediator of the regulation of glucose and glucagon, of lipid metabolism and is an independent predictor of metabolic syndrome in adults but not in children [49].
Results of this reports showed that children decreased their total caloric intake by an average of 2436 kJ/day (582 kcal) after 8 weeks. L-CHO diet group decreased 2,554 kJ/day (616 kcal). It is very interesting to observe that a comparison of the changes between the two dietary interventions was made. Total LDLcholesterol levels decreased significantly with the L-F diet. Using the multiple regression procedure, it was found that prior to diet; FGF21 was positively associated with total cholesterol, triglycerides and body mass index.
After dietary treatment with the L-CHO and L-F diets, the association with BMI remained significant. The researchers concluded among other things that the results indicate that the feeding behavior in children is modified favorably with both diets. Besides that Leptin decreased with both diets, and this hormone was positively associated with BMI. The release of leptin depends on both mass and adipose nutrient flux, which is mainly represented by hexosamines in the adipocyte.
Insulin levels show a tendency to decrease that is not significant. In adults, short-term food restriction induces a decrease in insulin levels [50]. In children, a significant decrease in insulin has been reported with only 6 months and 16 weeks of diet [51]; however, in children decreased insulin can be observed after 2 weeks of diet and exercise. This finding may indicate that in children, leptin is more sensitive to calorie restriction than insulin levels [52].
Leptin and physical activity in the development of childhood obesity
Regular physical activity is an important contributor to good overall health, including promoting healthy weight and reducing chronic disease risk in Children. For instance, studies from Australia revealed that on average, children and young people aged 5-17 years spent one and a half hours (91 minutes) per day on physical activity and over two hours a day (136 minutes) in screen-based activity with physical activity decreasing and screen-based activity increasing as age increased [53].
The studies considered a pediatric population around 12 years of age, and we sought in this study to associate the effects of physical exercise on the metabolic variables associated with childhood obesity. The main physiological and metabolic effects that result from both acute and chronic exercise in general are: increased skeletal muscle mass, strength and proprioception of gain, decreased fat stores, increased caloric expenditure, increased resting metabolic rate, increased glucose tolerance to be used as energy substrate, improved insulin sensitivity, decreased inflammatory status, among others.
Moderate-intensity and fun-filled leisure activities for 12 weeks were effective in attenuating dyslipidemia and hemodynamic factors associated with worsening health status of obese children with an average body mass index (BMI) of 40 kg/m2.
In another study conducted by Escalante et al., reported that physical exercise can reduce low-density lipoprotein (LDL) by 35% and triglycerides by 40%, and increase high-density lipoprotein (HDL) by up to 25%. Therefore, exercise is considered by many authors as the main tool to mitigate the damage associated with childhood obesity [54].
On the other hand, the association between serum leptin and physical activity level was evaluated in 59 obese students. Boys who spent at least two hours a day in physical activity were considered active. It was concluded that among active students, serum leptin was three times lower than sedentary leptin, suggesting an improvement in the sensitivity of leptin to active girls [55].
In addition, exercise increases the uptake of glucose by muscle cells and therefore increases the oxidation of glucose [56].
Conclusions
There are five drugs that Available agents are able to help patients achieve, on average, 5%-15% weight loss, which usually leads to significant improvements in many comorbid conditions, including hyperglycemia and diabetes, hyperlipidemia, hypertension, and others. There are: Qsymia, Belviq, Contrave, Xenical and Saxenda®.
The attenuation of the hyperphagia in children is done through an adequate management of a food diet, aerobic physical activity and regular sleep; these factors induce the anorexigenic effect of leptin. At the pharmacological level, orlistat have been used in teenagers to improve the state of abdominal obesity.
References
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, et al. (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 384: 766-781.
- https://www.eldia.com/informacion-general/la-oms-publico-el-mapa-interactivo-del-sobrepeso-y-la-obesidad-en-el-mundo-69869
- Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, et al. (2015) Childhood obesity: Causes and consequences. J Family Med Prim Care 4: 187-192.
- Clark JE (2015) Diet, exercise or diet with exercise: Comparing the effectiveness of treatment options for weight-loss and changes in fitness for adults (18–65 years old) who are overfat, or obese; systematic review and meta-analysis. J Diabetes Metab Disord 14: 31.
- National CGCU (2014) Obesity: Identification, assessment and management of overweight and obesity in children, young people and adults: Partial update of CG43.
- Pigeyre M, Yazdi FT, Kaur Y, Meyre D (2016) Recent progress in genetics, epigenetics and metagenomics unveils the pathophysiology of human obesity. Clin Sci (Lond) 130: 943-986.
- Apovian CM (2016) The obesity epidemic-Understanding the disease and the treatment. N Engl J Med 374: 177-179.
- Kahan S (2017) Quick Takes: What You Need to Know About The 5 FDA-Approved Obesity. Medscape. https://www.medscape.com/viewarticle/876411
- Siebenhofer A, Jeitler K, Horvath K, Berghold A, Posch N, et al. (2016) Long-term effects of weight-reducing drugs in people with hypertension. Cochrane Database Syst Rev 3: CD007654.
- Yanovski SZ, Yanovski JA (2014) Long-term drug treatment for obesity: A systematic and clinical review. Jama 311: 74-86.
- Coelho RC (2015) Anti-Obesity drugs: A necessary part of treatment. J Obes Weight-Loss Medic 1: 001e.
- Morton GJ, Meek TH, Schwartz MW (2014) Neurobiology of food intake in health and disease. Nat Rev Neurosci 15: 367-378.
- Woods SC, D'Alessio DA (2008) Central control of body weight and appetite. J Clin Endocrinol Metab 93: s37-s50.
- Schneeberger M, Gomis R, Claret M (2014) Hypothalamic and brainstem neuronal circuits controlling homeostatic energy balance. J Endocrinol 220: T25-T46.
- Suzuki K, Jayasena CN, Bloom SR (2012) Obesity and appetite control. Exp Diabetes Res 2012: 824305.
- Müller TD, Nogueiras R, Andermann ML, Andrews ZB, Anker SD, et al. (2015) Ghrelin. Mol Metab 4: 437-460.
- AL-Jumaily EF, Zgaer SH (2014) A Review: “Leptin structure and mechanism actions”. Bull Env Pharmacol Life Sci 3: 185-192.
- Yan J, Mei FC, Cheng H, Lao DH, Hu Y, et al. (2013) Enhanced leptin sensitivity, reduced adiposity, and improved glucose homeostasis in mice lacking exchange protein directly activated by cyclic AMP isoform 1. Mol Cell Biol 33: 918-926.
- Vasselli JR, Scarpace PJ, Harris RB, Banks WA (2013) Dietary components in the development of leptin resistance. Adv Nutr 4: 164–175.
- Heldsinger A, Grabauskas G, Song I, Owyang C (2011) Synergistic Interaction between leptin and cholecystokinin in the Rat Nodose Ganglia is mediated by PI3K and STAT3 signaling pathways: Implications for leptin as a regulator of short term satiety. J Biol Chem 286: 11707-11715.
- Morabito MV, Ravussin Y, Mueller BR, Skowronski AA, Watanabe K, et al. (2017) Weight perturbation alters leptin signal transduction in a region-specific manner throughout the brain. PloS one 12: e0168226.
- Von Schnurbein J, Heni M, Moss A, Nagel SA, Machann J, et al. (2013) Rapid improvement of hepatic steatosis after initiation of leptin substitution in a leptin-deficient girl. Horm Res Paediatr 79: 310-317.
- Inagaki-Ohara K, Okamoto S, Takagi K, Saito K, Arita S, et al. (2016) Leptin receptor signaling is required for high-fat diet-induced atrophic gastritis in mice. Nutr Metab (Lond) 13: 7.
- Paz-Filho G, Mastronardi C, Franco CB, Wang KB, Wong ML, et al. (2012) Leptin: molecular mechanisms, systemic pro-inflammatory effects, and clinical implications. Arq Bras Endocrinol Metabol 56: 597-607.
- Londoño-Lemos ME (2012) Pharmacological treatment against obesity. Rev Colomb Cienc Quim Farm 41: 217-261.
- Sobrino Crespo C, Perianes Cachero A, Puebla Jiménez L, Barrios V, Arilla Ferreiro E (2014) Peptides and food intake. Front Endocrinol 5: 58.
- Dalamaga M, Chou SH, Shields K, Papageorgiou P, Polyzos SA, et al. (2013) Leptin at the intersection of neuroendocrinology and metabolism: Current evidence and therapeutic perspectives. Cell Metab 18: 29-42.
- Kotz C, Nixon J, Butterick T, PerezÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡ÃâÃÂLeighton C, Teske J, et al. (2012) Brain orexin promotes obesity resistance. Ann N Y Acad Sci 1264: 72-86.
- Samuelsson AM, Clark J, Rudyk O, Shattock MJ, Bae SE, et al. (2013) Experimental hyperleptinemia in neonatal rats leads to selective leptin responsiveness, hypertension, and altered myocardial function. Hypertension 62: 627-633.
- Zhou Y, Rui L (2013) Leptin signaling and leptin resistance. Front Med 7: 207-222.
- Friedman J (2012) Leading the charge in leptin research: An interview with Jeffrey Friedman. Dis Model Mech 5: 576-579.
- Guyenet SJ, Schwartz MW (2012) Regulation of food intake, energy balance, and body fat mass: Implications for the pathogenesis and treatment of obesity. J Clin Endocrinol Metab 97: 745-755.
- Thaler JP, Yi CX, Schur EA, Guyenet SJ, Hwang BH, et al. (2012) Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest 122: 153-162.
- https://www.health.harvard.edu/staying-healthy/foods-that-fight-inflammation
- De Vadder F, Kovatcheva-Datchary P, Goncalves D, Vinera J, Zitoun C, et al. (2014) Microbiota-generated metabolites promote metabolic benefits via gut-brain neural circuits. Cell 156: 84-96.
- Kang S, Kim KB, Shin KO (2013) Exercise training improve leptin sensitivity in peripheral tissue of obese rats. Biochem Biophys Res Commun 435: 454-459.
- Sakurai T, Ogasawara J, Kizaki T, Sato S, Ishibashi Y, et al. (2013) The effects of exercise training on obesity-induced dysregulated expression of adipokines in white adipose tissue. Int J Endocrinol 2013: 801743.
- Venancio DP, Suchecki D (2015) Prolonged REM sleep restriction induces metabolic syndrome-related changes: Mediation by pro-inflammatory cytokines. Brain Behav Immun 47:109-117.
- Banks WA (2012) Role of the blood–brain barrier in the evolution of feeding and cognition. Ann N Y Acad Sci 1264: 13-19.
- Pesta DH, Samuel VT (2014) A high-protein diet for reducing body fat: Mechanisms and possible caveats. Nutr Metab (Lond) 11: 53.
- Aragonès G, ArdidÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡ÃâÃÂRuiz A, Ibars M, Suárez M, Bladé C (2016) Modulation of leptin resistance by food compounds. Mol Nutr Food Res 60: 1789-1803.
- https://www.ptcommunity.com/news/20170421/fda-approves-orlistat-use-teenagers
- https://patient.info/doctor/obesity-in-children
- Sherafat-Kazemzadeh R, Yanovski SZ, Yanovski JA (2013) Pharmacotherapy for childhood obesity: Present and future prospects. Int J Obes (Lond) 37: 1-15.
- Steyn FJ, Xie TY, Huang L, Ngo ST, Veldhuis JD, et al. (2013) Increased adiposity and insulin correlates with the progressive suppression of pulsatile GH secretion during weight gain. J Endocrinol 218: 233-244.
- O'Neill S, O'Driscoll L (2015) Metabolic syndrome: A closer look at the growing epidemic and its associated pathologies. Obes Rev 16: 1-12.
- Potthoff MJ (2017) FGF21 and metabolic disease in 2016: A new frontier in FGF21 biology. Nat Rev Endocrinol 13: 74-76.
- De Sousa-Coelho AL, Relat J, Hondares E, Pérez-Martí A, Ribas F, et al. (2013) FGF21 mediates the lipid metabolism response to amino acid starvation. J Lipid Res 54: 1786-1797.
- Ko BJ, Kim SM, Park KH, Park HS, Mantzoros CS (2014) Levels of circulating selenoprotein P, fibroblast growth factor (FGF) 21 and FGF23 in relation to the metabolic syndrome in young children. Int J Obes (Lond) 38: 1497-1502.
- Gower BA, Goss AM (2015) A lower-carbohydrate, higher-fat diet reduces abdominal and intermuscular fat and increases insulin sensitivity in adults at risk of type 2 diabetes. J Nutr 145: 177S-183S.
- Armeno ML, Krochik AG, Mazza CS (2011) Evaluation of two dietary treatments in obese hyperinsulinemic adolescents. J Pediatr Endocrinol Metab 24: 715-722.
- Ibarra-Reynoso Ldel R, Pisarchyk L, Pérez-Luque EL, Garay-Sevilla ME, Malacara JM (2015) Dietary restriction in obese children and its relation with eating behavior, fibroblast growth factor 21 and leptin: A prospective clinical intervention study. Nutr Metab (Lond) 12: 31.
- https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.004Chapter1002011-12
- Escalante Y, Saavedra JM, García-Hermoso A, Domínguez AM (2012) Improvement of the lipid profile with exercise in obese children: A systematic review. Prev Med 54: 293-301.
- Plonka M, Toton-Morys A, Adamski P, Suder A, Bielanski W, et al. (2011) Association of the physical activity with leptin blood serum level, body mass indices and obesity in schoolgirls. J Physiol Pharmacol 62: 647-656.
- Sylow L, Kleinert M, Richter EA, Jensen TE (2017) Exercise-stimulated glucose uptake-regulation and implications for glycaemic control. Nat Rev Endocrinol 13: 133-148.