Liufen Pan1 and Hui Zhi2*
1Department of Ultrasound, Longgang People’s Hospital, Jianshedong Rd, Shenzhen 518118, China
2Department of Ultrasound, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, 107 Yanjiangxi Rd, Guangzhou 510120, China
Corresponding Author:
Hui Zhi, MD
Department of Ultrasound, Sun Yat-sen Memorial Hospital
Sun Yat-sen University, 107 Yanjiangxi Rd
Guangzhou 510120, China
Tel: +86-20-8133-2516
E-mail: zhihui18123@163.com
Received Date: March 10, 2017; Accepted Date: April 03, 2017; Published Date: April 08, 2017
Citation: Zhi F, Pan L. Polyorchidism: A Case Report and Review. Br J Res 2017, 4:8. doi:10.21767/2394-3718.100008
Copyright: © 2017 Pan L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Polyorchidism; Ultrasound; Ultrasound elastography
Introduction
Polyorchidism is an uncommon congenital anomaly, defined as the presence of more than two testis. To date, more than 180 cases have been reported in the literature, but only a few cases were diagnosed by ultrasound [1] and there was no relevant report about the physical properties of the supernumerary testis according to ultrasound elastography. We report on an interesting case of polyorchidism in a 22-year-old man diagnosed by ultrasound and discuss the literature and the physical properties of the entire testis by ultrasound elastography.
Case report
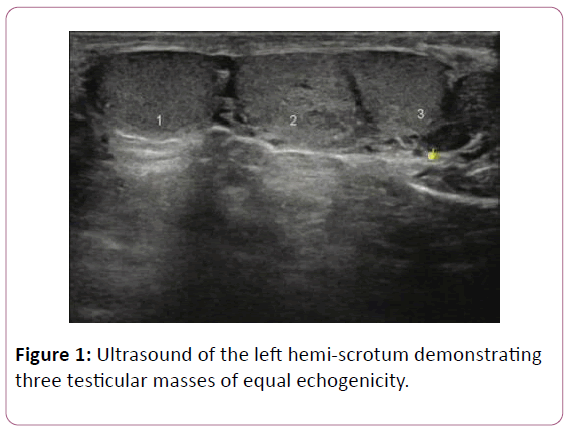
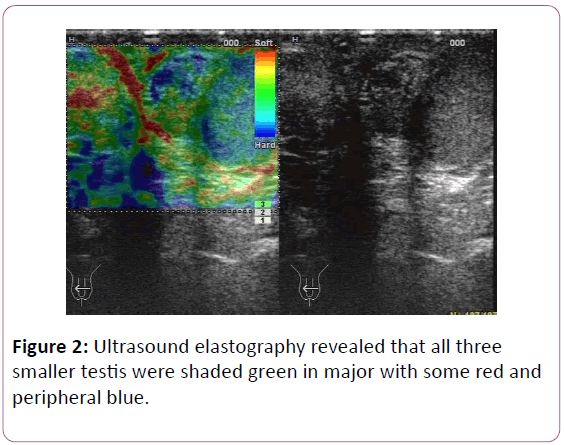
A 22-year-old man was referred to our department because of varicocele. He presented with inguinal swelling without any other symptoms. On palpation, left epididymis presented with a small mass which is around the same size as two fingers. Scrotal ultrasound with a 13.5-MHz linear transducer revealed a normal testicular gland on the right side and three smaller testis in the left scrotum (Figure 1). The right testis measured 44.6 × 17.0 mm, and the three left glands measured 16.5 × 11.5 mm, 15.8 × 12.5 mm and 14.8 × 11.0 mm, respectively. Ultrasound image also showed classic testicular microlithiasis of all four testis. Right testis was covered with its own tunica as well as connected to an epididymis. Three left testis were covered with an epididymis. Ultrasound examination of the scrotum also revealed significant left spermatic vein reflux and left varicocele. Ultrasound elastography revealed that all three smaller testis and the normal testis were shaded green in major with some red and peripheral blue (Figure 2).
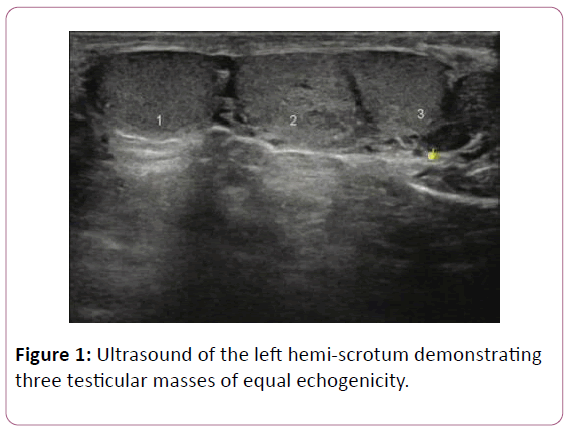
Figure 1: Ultrasound of the left hemi-scrotum demonstrating three testicular masses of equal echogenicity.
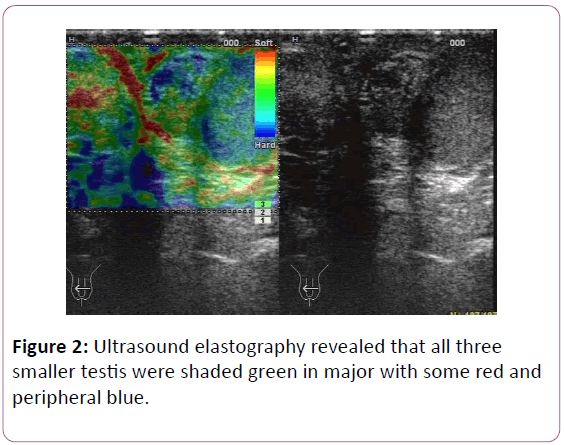
Figure 2: Ultrasound elastography revealed that all three smaller testis were shaded green in major with some red and peripheral blue.
After lengthy discussion and counseling of the patient, abdominal laparotomy was explored. During abdominal laparotomy, three testicles of approximately equal size were found connected to a single vas deferens. The patient recovered well and was satisfied with the outcome. Then ultrasound was performed after three months and showed no alterations compared with the original findings.
Discussion
Polyorchidism is a rare malformation and it was our first case of polyorchidism diagnosed by ultrasound in our hospital.
Most cases of polyorchidism are found incidentally during evaluation for other symptoms and our patient present with inguinal swelling. In polyorchidism, triorchidism is the most common type. Most cases of polyorchidism had been reported on the left side [2]. Our case also occurred on the left side, but there were three testis in left scrotum. Classifications of polyorchidism have been described [3]. The previous study reported that the most common type of polyorchidism was A3, followed by A1 and A2, which was classified for functional taxonomy of polyorchidism [1]. The type of our case was A3: when there were more than one testis, the drained supernumerary testis can share a common epididymis with its neighbor. The presence of accessory testis may be associated with other anomalies, including cryptorchidism, indirect inguinal hernia, and torsion of testis [4], hydrocele, epididymitis, varicocele and malignancy [1]. Our patient had varicocele and conventional sonography revealed it.
Careful diagnosis is necessary in every suspicious testicular finding. Ultrasound can rule out polyorchidism, so surgical exploration or biopsy may be not necessary. It has been reported that polyorchidism can be diagnosed by magnetic resonance imaging [5]. The diagnosis of polyorchidism was made by ultrasound and a simple scrotal exploration suffices in our patient. Because the patient took the surgical treatment in hospital for the left varicocoele and a simple scrotal exploration suffice of the scrotum was performed along the way. Furthermore, close follow-up should be performed in our patient because masses were not been completed excluded [6-8]. Our plan was to examine it by ultrasound and other clinical examinations every three months.
We also studied the physical properties of the accessory testis. We found that the ultrasound elastography of the three small testis were similar to that of the normal testis. The typical distribution of elasticity of a normal testis shows mainly green (intermediate), some linear red (arrow heads) and peripheral light blue [9]. The “blue” structures are related to coated effect. The linear “red” structures are related to fluid component. Several studies had found that ultrasound elastography is helpful in differentiating malignant from benign lesions of the testicles [9-11]. Schurich et al. had reported that ultrasound elastography demonstrates different elasticity values dependent on testicular volume and function [12]. In 2012, Li et al. reported that ultrasound elastography is a promising imaging method for the differential diagnosis between non-obstructive and obstructive azoospermia [13]. The next interesting question is whether the smaller testis had the same or reduced spermatogenesis. Maybe ultrasound elastography reflected the transformation of spermatogenesis by measuring the hardness of testis and biopsy may be not necessary.
Conclusion
We reported on an interesting case of polyorchidism in a 22- year-old man diagnosed by ultrasound and discuss the physical properties of the entire testis by ultrasound elastography and we concluded that the three accessory testis had the same hardness with the normal one.
References
- Bergholz R, Wenke K (2009) Polyorchidism: A Meta-Analysis. Pediatric Urology 182: 2422-2427.
- Leung AK (1988) Polyorchidism. Am Fam Physician 38: 153-156.
- Bergholz R, Koch B, Spieker T, Lohse K (2007) Polyorchidism: a case report and classification. J PediatrSurg 42: 1933-1935.
- Ibrahim H, Roberts MJ, Hussey D (2016) Quadruple Orchidopexy for Torsion Testis in an Adolescent With Polyorchidism: A Case Report. Urology87:196-199,
- Myers A, Morganstern B, Fine R (2017) A Unique Case of Pentaorchidism. Urology S0090-4295: 30270-30274.
- Zuppa AA, Nanni L, Di Gregorio F, Visintini F, Buonuomo V, et al. (2006) Complete epididymal separation presenting as polyorchidism. J Clin Ultrasound 34: 258-260.
- Mor Y, Leibovitch I, Duvdevani M, Jacobson J, Fridman E, et al. (2004) Scrotal epidermal inclusion cyst clinically mimicking polyorchidism in a child: ultrasonic characteristics. PediatrRadiol34: 175-176.
- Akbar SA, Sayyed TA, Jafri SZ, Hasteh F, Neill JS(2003) Multimodality imaging of paratesticular neoplasms and their rare mimics. Radiographics23: 1461-1476.
- Goddi A, Sacchi A, Magistretti G, Almolla J, Salvadore M (2012) Real-time tissue elastography for testicular lesion assessment. EurRadiol22: 721-730.
- Grasso M, Blanco S, Raber M, Nespoli L (2010) Elastosonography of the testis: preliminary experience. Arch ItalUrolAndrol82: 160-163.
- Trottmann M, Marcon J, D'Anastasi M, Karl A, Stief CG, et al. (2014) The role of VTIQ as a new tissue strain analytics measurement technique in testicular lesions. Clinical Hemorheology and Microcirculation 58: 195-209.
- Schurich M, Aigner F, Frauscher F, Pallwein L (2009) The role of ultrasound in assessment of male fertility. Eur J ObstetGynecolReprodBiol 144(Suppl 1): S192-S198.
- Li M, Du J, Wang ZQ, Li FH (2012) The Value of Sonoelastography Scores and the Strain Ratio in Differential Diagnosis of Azoospermia. The Journal of Urology 188: 1861-1866.