- (2013) Volume 14, Issue 3
Edward Sun*, Mathew Tharakan, Sumit Kapoor, Rajarshi Chakravarty, Aladin Salhab, Jonathan M Buscaglia and Satish Nagula
Division of Gastroenterology and Hepatology, Department of Internal Medicine, Stony Brook University Medical Center, State University of New York at Stony Brook. Stony Brook, NY, USA
Received May 18th, 2012 – Accepted May 31st, 2012
Context Despite recent updates in the treatment of acute pancreatitis emphasizing enteral nutrition over parenteral nutrition as well as minimizing antibiotic usage, mortality rates from acute pancreatitis have not improved. Data has been limited regarding physician compliance to these guidelines in the United States. Methods A 20 question survey regarding practice patterns in the management of acute pancreatitis was distributed to physicians at multiple internal medicine and gastroenterology conferences in North America between 2009 and 2010. Responses were analyzed using the chi-square test and multivariate logistic regression. Results Out of 406 available respondents, 43.3% of physicians utilize total parenteral nutrition/peripheral parenteral nutrition (TPN/PPN) and 36.5% utilize nasojejunal (NJ) feedings. The preferred route of nutrition was significantly related to practice type (P<0.001): academic physicians were more likely to use NJ tube feeding than private practice physicians (52.1% vs. 19.9%) while private practitioners were more likely to utilize TPN/PPN than academic physicians (70.2% vs. 20.5%). Gastroenterologists and primary care physicians were equally non-compliant as both groups favored parenteral nutrition. Multivariate logistic regression demonstrated that practice type (P<0.001) was the only independent predictor of route of nutrition. Most survey respondents appropriately do not routinely utilize antibiotics for acute pancreatitis, but when antibiotics are initiated, they are for inappropriate indications such as fever and infection prophylaxis. Conclusions Many North American physicians are noncompliant with current ACG practice guidelines for the use of artificial nutrition in the management of acute pancreatitis, with overuse of TPN/PPN and underutilization of jejunal feedings. Antibiotics are initiated in acute pancreatitis for inappropriate indications, although there are conflicting recommendations for antibiotics in severe acute pancreatitis. Improved compliance with guidelines is needed to improve patient outcomes.
Anti-Bacterial Agents; Health Planning Guidelines; Nutritional Status; Pancreatitis
ACG: American College of Gastroenterology; BSG: British Society of Gastroenterology; IAP: International Association of Pancreatology; JSAEM: Japan Society of Abdominal Emergency Medicine; NJ: nasojejunal; PPN: peripheral parenteral nutrition; TPN: total parenteral nutrition
Acute pancreatitis remains a significant problem in the United States, with an estimated 210,000 admissions for acute pancreatitis each year, with evidence to suggest a global trend toward an increasing incidence of disease [1, 2]. Multiple studies over the past decade have updated the treatment of acute pancreatitis with regards to nutrition and antibiotics which are reflected in the 2006 American College of Gastroenterology (ACG) practice guidelines [3].
Current guidelines on feeding emphasize the use of enteral nutrition over total parenteral nutrition (TPN) or peripheral parenteral nutrition (PPN) [3]. Clinical studies have demonstrated enteral nutrition to be associated with a decreased risk of infection and a decreased hospital length of stay when compared to TPN [4]. Furthermore, parenteral nutrition has been associated with central line infections, metabolic complications, electrolyte imbalances, increased cost, and ultimately increased mortality [5, 6, 7]. Jejunal feeding via nasojejunal (NJ) tubes (placed at least 40 cm past the ligament of Trietz) is preferred as it minimizes pancreatic stimulation [8, 9].
Current guidelines do not endorse the use of antibiotics in the management of acute pancreatitis. However, the literature has been conflicting regarding the role of antibiotics in severe acute pancreatitis. Although early studies favored the use of imipenem for infection prophylaxis in severe acute pancreatitis [10, 11], some studies since that time have demonstrated an increased rate of fungal infection and infection with antimicrobial resistant organisms [12]. Current ACG guidelines advise against the routine use of prophylactic antibiotics in both acute pancreatitis and severe acute pancreatitis. Empiric antibiotics are warranted in cases of severe acute pancreatitis when there is pancreatic necrosis and suspected sepsis with fever, leukocytosis and/or organ failure.
While it is well documented that compliance to guidelines is suboptimal in other countries, no studies to date have directly examined how well physicians in North America are following guidelines in the treatment of acute pancreatitis [13, 14, 15, 16]. The objective of this study is to assess physician adherence to current practice guidelines with regards to antibiotics and nutrition in the management of acute pancreatitis in North America.
A 20 question survey was created, addressing physician attitudes toward the use of nutrition and antibiotics in acute pancreatitis (Appendix). Representatives from Stony Brook (including medical residents and gastroenterology fellows) distributed the survey to physicians in person at multiple North American regional and national internal medicine and gastroenterology conferences between 2009 and 2010: 2009 New York Society for Gastrointestinal Endoscopy Post Graduate Course in New York, NY, USA (636 physician attendees); 2009 American College of Gastroenterology in San Diego, CA, USA (4,103 total participants, 3,487 physician attendees); 2010 Digestive Diseases Week in New Orleans, LA, USA (13,000 total attendees); 2010 American College of Physicians Annual Internal Medicine Meeting in Toronto, Ontario, Canada (7,925 total participants, 6,026 physician attendees). Surveys were distributed outside conference lecture halls for 8 hours a day during the first 3 days of each conference. The surveys were distributed at random, and survey responses were made anonymously; surveys were collected immediately after completion [17]. At the conclusion of each conference, survey responses were entered in a centralized database.
Respondents
The survey was distributed to 462 physicians, a total of 451 completed surveys was returned, with a response rate of 97.6%. Thirty-seven surveys were excluded due to missing demographic data, yielding a total of 414 surveys for inclusion in this study (89.6% of the distributed surveys). There was a relatively even distribution with regards to age and years from training (Table 1). Of the survey respondents, 171 (41.3%) were gastroenterologists and the remaining 243 (58.7%) were primary care physicians. Respondents practiced in a variety of clinical settings, including community hospitals (n=169; 40.8%), universityaffiliated hospitals (n=139, 33.6%), and university/ tertiary care centers (n=106, 25.6%). Respondents identified themselves as having a full-time academic practice (n=121; 29.2%), a hybrid private/academic practice (n=130; 31.4%), or a full-time private practice (n=163; 39.4%).

This study was granted exemption from review by the Stony Brook University Medical Center Institutional Review Board. Informed oral consent was obtained from each respondent. No incentives were provided to the study participants.
Surveys without complete demographic data were completely excluded from the analysis. Blank responses to individual questions were excluded from the analysis of that question; no imputations were made for missing data. The chi-square test was used to assess the association between demographic variables and survey responses. Univariate and multivariate logistic regression analysis was used to determine which demographic variables were independently associated with route of nutrition (NJ tube versus TPN/PPN; NG tube and other route were excluded from these analyses). The simple contrast was applied to all variables in the logistic regression analysis in order to calculate odds ratios (ORs) together with their 95% confidence intervals. Statistical analysis was performed using Stata v9.0 (Stata Corp, College Station, TX, USA). A two-tailed P value less than 0.05 was considered statistically significant.
Nutrition and Acute Pancreatitis
When asked which route of artificial nutrition was most often utilized in the management of acute pancreatitis data were available in 406 surveys (98.1% of evaluable surveys). In particular, 43.1% (n=175) of respondents used TPN/PPN and 36.5% (n=148) chose NJ tube feeding (Table 2). The preferred route of administration was significantly (P<0.001) related to the practice type: academic physicians (52.1%, 61/117) were more likely to utilize NJ tubes compared to private practitioners (19.9%, 32/161), whereas private practice physicians (70.2%, 113/161) were more likely to use TPN/PPN than academic physicians (20.5%, 24/117). When comparing gastroenterologists to primary care physicians, both groups favored parenteral nutrition over NJ tube feeding (P=0.151).

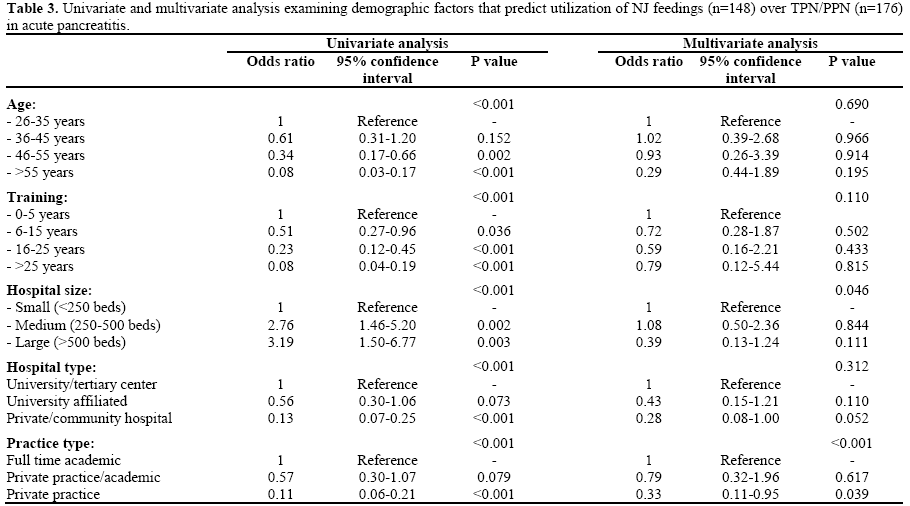
Table 3 shows the results of univariate and multivariate analyses made in order to determine which factors were associated with the use of NJ feedings over TPN/PPN. Five demographic factors were associated with route of nutrition at univariate logistic regression analysis: age, years from training, hospital size, hospital type, and practice type. Using a multivariate logistic regression model, practice type (P<0.001) was confirmed as an independent predictor of the preferred route of nutrition chosen by a given practitioner. In particular, private practice physicians were more likely to utilize TPN/PPN, whereas academic physicians typically used NJ tube feeding when initiating artificial nutrition in acute pancreatitis. As far as the other predictors were concerned, age, training, and hospital type lost their role while hospital size had an overall significant P value in the multivariate model, but it is hazardous to consider this an independent predictive variable for the utilization of NJ feeds because there was no trend amongst the different hospital size categories, as well as both ORs values were not significant.
Respondents were asked to identify barriers to initiating enteral nutrition in acute pancreatitis. Amongst the 411 respondents who did not first initiate enteral feedings, the most common reasons cited for using parenteral nutrition were need for complete bowel rest (37.0%, n=152) and ease of access (38.0%, n=156) (Figure 1). No significant differences were identified between gastroenterologists and primary care physicians with regards to barriers to initiating enteral nutrition (data not shown).
Respondents to our survey infrequently utilized antibiotics in the management of acute pancreatitis, with 62.3% (243 out of the 390 available responses) stating they used antibiotics in less than 25% of patients with acute pancreatitis. No significant differences were seen between academic physicians and private practitioners (80/112, 71.4% vs. 90/155, 58.1%, respectively utilize antibiotics in less than 25% of their patients; P=0.112; Table 4) while gastroenterologists utilized antibiotics less frequently than primary care physicians (126/163, 77.3% vs. 117/227, 51.5% use antibiotics in less than 25% of patients, respectively; P<0.001).

When asked what was the most common reason for initiating antibiotics in acute pancreatitis, fever (54.2%, 195 out of 360 available responses) and prophylaxis against infection (17.5%, n=63) were the two most common responses (Figure 2). Academic physicians (51.0%, 52/102) and private practitioners (47.2%, 68/144) chose fever as the single most common reason to initiate antibiotics in acute pancreatitis (P=0.605). While primary care physicians (69.6%, n=149/214) were more likely than gastroenterologists (31.5%, 46/146; P<0.001) to choose fever as the most common indication to start antibiotics in acute pancreatitis, fever was still the primary response in both groups.
In contrast, physicians often administered antibiotics in patients with severe acute pancreatitis, with 40.9% (n=159) of 389 respondents giving antibiotics in more than 75% of patients with severe acute pancreatitis, with academic physicians (34/112, 30.4%) and gastroenterologists (44/163, 27.0%) providing antibiotics less frequently than private practitioners (77/155, 49.7%) and primary care physicians (115/226, 50.9%), respectively (P=0.009 and P<0.001 for practice type and specialty, respectively) (Table 4). The most often cited reason for initiating antibiotics in severe acute pancreatitis was pancreatic necrosis (41.6%, 147 out of 353 available responses), followed by positive cultures (27.5%, n=97), and fever (18.4%, n=65), without any significant differences by practice type or specialty (data not shown).
Acute pancreatitis remains a common indication for hospital admission, both in the United States and across the world. Approximately 20% of these patients develop severe acute pancreatitis, requiring intensive medical and surgical management and prolonged hospital stays. The overall mortality from acute pancreatitis is 5%, with higher death rates in patients with severe acute pancreatitis. Recent developments have resulted in various guidelines on the management of acute pancreatitis favoring the use of enteral nutrition as well as limiting the use of empiric antibiotics.
It is important to note that many guidelines exist regarding the management of acute pancreatitis. A recent systematic review analyzed 30 acute pancreatitis guidelines using validated guideline scoring instruments. [18] Among the major American guidelines, the 2006 American College of Gastroenterology (ACG) guidelines had the highest quality scores, validating its use in this study. Internationally, however, there are three other wellvalidated guidelines in the management of acute pancreatitis: the 2002 International Association of Pancreatology (IAP) guidelines [19], the 2005 British Society of Gastroenterology (BSG) guidelines [20], and the 2006 Japan Society of Abdominal Emergency Medicine (JSAEM) guidelines [21].
The ACG, BSG and JSAEM guidelines all advocate for the use of enteral nutrition over parenteral nutrition (the IAP guidelines not comment on nutritional support). However, the role of prophylactic antibiotic administration is far more controversial. Although the ACG guidelines clearly recommends against prophylactic antibiotics, the JSAEM guidelines recommends the use of antibiotics with adequate tissue penetration (e.g. carbapenems) in severe disease [20].
The BSG guidelines recognize the lack of consensus regarding antibiotic use [19], and the IAP guidelines suggest that antibiotics may not improve survival [18]. These recommendations reflect the heterogeneity of the underlying clinical data, with different studies demonstrating varying benefits of antibiotics.
Recognizing the variability among these practice guidelines, this study assessed physician compliance from physicians attending the specifically mentioned North American medical conferences. Acute pancreatitis is typically treated with supportive care including aggressive fluid hydration, pain control, and controlled re-initiation of oral intake. Typically, a diet is reintroduced as the patient’s appetite returns and abdominal pain subsides. In order to minimize complications from malnutrition, nutritional support is indicated for patients with protracted symptoms beyond 5-7 days. TPN had historically been favored as the primary means of nutritional support in severe acute pancreatitis because it minimized enteral stimulation, allowing for suppression of pancreatic activity. However, studies in recent years have shown TPN to be associated with potential harms including an increased risk of electrolyte disturbances as well as local and systemic infection [22]. On the other hand, enteral nutrition minimizes the risk of bacterial translocation by preventing intestinal atrophy and improving gut barrier function [23]. Clinical trials have demonstrated that jejunal feeding does not exacerbate the disease process, and that concordantly, enteral nutrition has been associated with improved outcomes with a decreased rate of infection, length of hospital stay, and decreased cost of care [24, 25, 26].
Despite the clinical evidence and multiple practice guidelines, our study found no significant difference in the number of responders who chose NJ tube feeding (37%) compared to those who chose TPN/PPN (43%) for nutrition support in acute pancreatitis. A multivariable regression model demonstrated that practice type was the only independent predictor of the preferred route of nutrition; with academic physicians favoring enteral nutrition as compared to private practice physicians who favor TPN. Interestingly, gastroenterologists demonstrated a similar level of noncompliance with the guidelines as primary care physicians with both groups choosing TPN over enteral nutrition. Respondents cited ease of access to TPN (38%) and perceived need for bowel rest (37%) as reasons to select TPN over enteral nutrition.
It seems reasonable that academic physicians in North America would be more compliant with current practice guidelines. Understanding of up-to-date and high quality guidelines is a critical part of training programs; given the paradigm shift from TPN to enteral nutrition occurred in recent years, physicians who are not actively involved in maintaining an awareness of current guidelines may not be aware of the updated approach to nutrition in acute pancreatitis. Academic physicians are potentially more apt to be aware of current literature as compared to private physicians because of their heavy involvement with clinical training programs. The perceived need for bowel rest as a rationale for TPN further highlights the lack of awareness of current literature amongst physicians. Based on survey responses, however, the problem may not lie in knowledge but in the availability and accessibility of resources. Ease of access to TPN is an important consideration; establishing jejunal access has historically been quite challenging, requiring either specialized endoscopic techniques or interventional radiology. These services may not be readily available to private practice physicians, particularly those working in the community hospital setting. On the contrary, most hospitals have TPN services readily available. Increasing familiarity with and the availability of newer technologies such as self-advancing nasojejunal tubes or through-the-scope nasojejunal tubes may make jejunal access more feasible in the community hospital setting.
The 2006 ACG guidelines do not support the routine use of antibiotics in the management of acute pancreatitis. In this survey, respondents reported they used antibiotics in a minority (<25%) of patients with acute pancreatitis, consistent with current American practice standards. However, when asked for what reasons to start antibiotics in acute pancreatitis, the most common response was fever, followed by prophylaxis against infection and elevated WBC. Given that there is no proven role for antibiotics in acute pancreatitis, the correct response to this question is “none of the above”, which only 12 physicians (3%) chose. This survey suggests that although physicians in North America infrequently use antibiotics in the management of acute pancreatitis, that when antibiotics are used, the indications cited by physicians are not supported by current practice guidelines.
While there is no role for antibiotics in management of acute pancreatitis [27], the role of antibiotics in treating severe acute pancreatitis is a far more controversial issue. Early clinical trials seemed to demonstrate a benefit to using antibiotics for prophylaxis to prevent infection in severe acute pancreatitis; three more recent double-blind, placebo-controlled trials were equivocal in describing any benefits with regards to the prevention of infected necrosis, the need for surgery, and mortality [28, 29, 30, 31]. The use of prophylactic broad-spectrum antibiotics has been associated with fungal infections, Clostridium difficile infection and increased cost [32, 33]. As such, current ACG guidelines recommend against the usage of prophylactic antibiotics in severe acute pancreatitis. However, when there is pancreatic necrosis and suspected sepsis (fever, leukocytosis and/or organ failure), empiric antibiotics are warranted while a definitive source of infection is identified.
Pancreatic necrosis was selected as the most common indication to start antibiotics, regardless of practice type or specialty. This may not reflect a lack of awareness of current ACG guidelines, which state that pancreatic necrosis alone is not an indication for antibiotics, and that clinical suspicion for an infection is required. Pancreatic necrosis is commonly sterile initially. However, because these patients are often critically ill, empiric antibiotics are frequently administered. In severe acute pancreatitis, physicians appear to overuse antibiotics, with 41% of physicians administering antibiotics in >75% of patients; the overuse appears to be most significant amongst primary care physicians and private practitioners. Gastroenterologists and academic physicians may have more experience with severe acute pancreatitis and are therefore understandably less likely to utilize empiric antibiotics. It is also important to note that although the ACG guidelines do not support prophylactic antibiotics, multiple other society guidelines advocate for the routine use of antibiotics in patients with pancreatic necrosis/severe acute pancreatitis [34].
The limitations of this study are those inherent in any survey study. Handing out surveys in person, however, ensured a high response rate (98%) as 462 surveys were distributed and 451 surveys were completed. While there were over 25,000 total attendees at all conferences where the survey was distributed, this study had no affiliation to the societies sponsoring each conference, and thus infeasible to ensure survey distribution to all conference attendees. We recognize also that a selection bias may have been introduced in this method of survey distribution. However, the even distribution in responder demographics based on age, practice type, specialty, and academic affiliation suggests that the sample was indeed random. Additionally, we assumed that the survey responses are reflective of actual practice patterns, but there may have been a tendency for physicians to provide the “correct” responses as opposed to responses that reflect their clinical practice. Since the respondents were attendees at regional conferences, they may also have been more aware of current guidelines, especially if they attended recent lectures on acute pancreatitis. That being said, however, our data demonstrates a tendency towards guideline non-compliance. It therefore seems reasonable to suspect that responses of the general population would be even more skewed towards noncompliance than those from conference attendees. We recognize that many of the attendees at these conferences may not have been from North America therefore including a question asking the region of clinical practice of our respondents would have been useful in our survey demographics. Although there are many potential questions to be addressed regarding the management of acute pancreatitis, this study focused on nutrition and antibiotics for brevity purposes.
In conclusion, most physicians are not compliant with the 2006 ACG guidelines regarding the use of artificial nutrition in the management of acute pancreatitis. Most physicians were found to favor parenteral nutrition over enteral nutrition, although academic physicians correctly utilize enteral feedings (via nasojejunal tube) over TPN/PPN. Although antibiotics are infrequently being used in acute pancreatitis, they are being initiated for inappropriate indications such as fever and infection prophylaxis. It is difficult to assess compliance with guidelines for antibiotics in severe acute pancreatitis, given conflicting recommendations from various societies. Greater consistency among guideline recommendations and improved adherence to such guidelines promise to improve outcomes of patients with acute pancreatitis through reductions in associated morbidity and mortality.
No grants or institutional financial support contributed to the research conducted from this study. No potential conflicts of interest exist in any part contributing to this manuscript including study design, data collection and analysis, and manuscript preparation.