Original Article - (2017) Volume 18, Issue 6
David Mossad, Brian Dinh, Ronald Markert, Mustafa Musleh, Sangeeta Agrawal
Boonshoft School of Medicine, Wright State University, USA
Received Date: September 07th, 2017; Accepted Date: October 10th, 2017
Background and Aims Pancreatitis presents with significant risk for morbidity and mortality acutely. The purpose of this study was to evaluate demographics, comorbidity burden, and hospital characteristics and their effect on in-hospital mortality in patients with acute pancreatitis. Methods Data was collected from The National Hospital Discharge Survey for patients admitted for acute pancreatitis from 2001-2010. Patients were separated into those who suffered in-hospital mortality and those that were discharged. Data was analyzed regarding demographics, length of stay, comorbidity burden, mortality, principal payment, and hospital size. Statistical comparisons were made using SPSS with chi-square and student T tests with a significance level of 0.05. Results 27,259 cases of acute pancreatitis were identified, with 573 who suffered in-hospital mortality. The mortality group was significantly older and had a longer length of stay. Patients with four or more comorbidities had a higher mortality rate (2.5%) compared to those with three or less (0.1%) (p<0.001). Region displayed a difference in mortality, with the Midwest showing a lower rate (1.6%) compared to all other regions. Mortality was lowest in small hospitals. Hospital ownership, however, did not show any significant differences in mortality. There was a difference in mortality rate when comparing principal forms of payment (p<0.001), with Medicare and Medicaid patients having the highest mortality rates. Conclusions Pancreatitis poses significant implications in morbidity and mortality in the acute setting. This study shows that factors such as age, length of stay, comorbidity burden, principal source of payment, and regional demographics have an impact on in-hospital mortality.
Pancreatitis; Morbidity; Mortality
SPSS Statistical Package for the Social Sciences
Acute pancreatitis (AP) is an inflammatory process of the pancreas that affects approximately 4.9 to 35 per 100,000 in the general population [1]. It is the leading cause of gastrointestinal hospital admission [2]. A large epidemiological study found that between 1988 and 2003, the mortality from acute pancreatitis decreased from 12% to 2% with a higher incidence of mortality among black males in their early 50’s [3]. Overall mortality of patients with acute pancreatitis admitted to the hospital is estimated to be 5% to 10% varying from 3% in mild AP to 30% in severe AP [4, 5].
With significant risk of morbidity and mortality associated with acute pancreatitis, multiple scoring systems have been developed to assess its severity. However, no single scoring system has been shown to be superior to others in predicting in-hospital mortality [6, 7]. One of the early systems, Ranson’s criteria, focuses on 11 factors with 5 assessed at the time of admission and 6 assessed 48 hours into admission. For scores <3, mortality was estimated to be 0% to 3%, scores ≥3 were associated with a 11% to 15% mortality, and scores ≥6 were associated with a 40% mortality. Although used widely, a meta-analysis showed that Ranson’s criteria had poor predictive value for acute pancreatitis severity [8].
Acute Physiology and Chronic Health Examination (APACHE) II, another cumbersome scoring system, was developed for use with critically ill patients, limiting its applicability. The APACHE II score uses age and 12 physiologic measures and can be calculated each day. Several studies have shown that an APACHE II score of less than 8 has a mortality rate <4% while a score greater than 8 results in mortality between 11% to 18% [5, 9].
Bedside Index of Severity in Acute Pancreatitis (BISAP) is a simpler calculation for determining early in-hospital mortality of patients admitted for acute pancreatitis. A BISAP score uses point assignments: 1 point for each of the following - BUN >25 mg/dL, abnormal mental status with Glasgow Coma Scale score <15, evidence of Systematic Inflammatory Response Sydrome (SIRS), >60 years of age, and imaging revealing pleural effusion. Patients with a score of zero have less than 1% mortality while a score of 3 to 5 is associated with >15% mortality.
A recent validation study found that BISAP had similar performance to APACHE II and Ranson’s criteria [10]. Moreover, BISAP compares favorably with newer scoring systems for bedside AP assessment, such as the “harmless acute pancreatitis score” and the “CT severity index” [10, 11].
In sum, AP severity scores are often unwieldy to measure and may require recalculation at later times during the hospital admission. In contrast, rather than focus on an AP score or index, other studies have investigated patient demographics (e.g., age), clinical characteristics (e.g., BMI, SIRS), various laboratory values, and radiological findings to determine AP severity and risk of mortality [12, 13, 14].
We examined selected demographic factors, comorbidities, and health care system characteristics that might be predictors of morality in hospitalized patients with acute pancreatitis.
Study data was acquired from the National Hospital Discharge Survey (NHDS), which is collected every year through the National Center for Health Statistics.
The NHDS collects patient hospitalizations and discharges from nonfederal hospitals across the United States with average length of stay of <30 days and ≥6 beds. Patient data in the NHDS is de-identified and made available to the public via the Center for Disease Control, making it exempt from an Institutional Review Board. The NHDS database was searched using International Classification of Diseases – Ninth Revision (ICD-9) diagnosis codes for patients admitted to hospitals with acute pancreatitis (ICD-9 code 577.0) from 2001-2010. For all patients included in the study, the following data was obtained: patient demographics (age, sex, race, marital status), hospital length of stay (LOS), hospital size (by number of beds), location/ownership (proprietary, government, or church/nonprofit), type of admission (emergency/urgent/ elective), source of admission, comorbidity burden, and mortality. This cohort was separated into two groups: those who died during the hospitalization and those who survived the hospitalization.
Means and standard deviations are reported for continuous variables, and counts and percents for categorical variables. The independent samples Mann- Whitney Test was used for comparisons involving the two groups (mortality vs. no mortality) and a second variable measured on a continuous scale. The chi square test was used to compare the two groups on categorical variables. Inferences for these univariate statistical tests were made at the 0.05 level of significance with no corrections for multiple comparisons. Multivariable logistic regression was used to identify independent risk factors of mortality. Data was first recorded in Excel, and analyses were conducted using IBM SPSS Statistics 23.0 (IBM, Armonk, NY).
Table 1 shows the results for 27,259 patients admitted for acute pancreatitis during the 2001-2010 periods. Of this group, 573 (2.1%) suffered in-hospital mortality. The mean age of patients who died was 64.5 years, which was significantly higher than the survival group’s mean age of 51.8 years (p<0.001). Only two races had a large number of patients: white (n=13,610) and African-American/ black (n=4984), and there was no difference in mortality between these two groups (white 2.3% vs. A-A/black 2.2%; p=0.55).
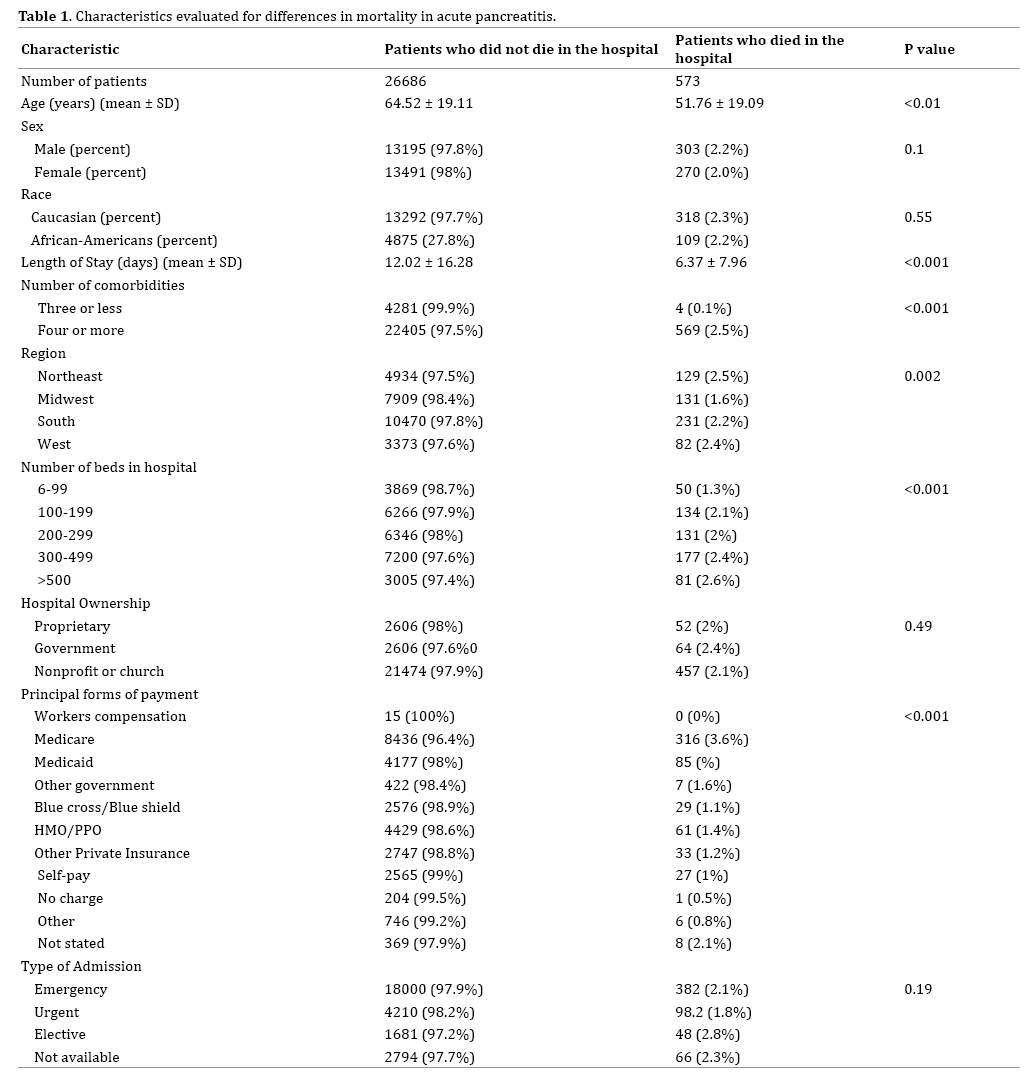
Mean length of stay was nearly double (12.0 vs. 6.4 days, p<0.001) in the mortality group. Patients with four or more comorbidities had a significantly higher mortality rate (2.5%) compared to those with three or fewer comorbidities (0.1%) (p<0.001).
Mortality was greater as hospital size increased, with the largest hospitals having the highest mortality rate (2.6%) and the smallest hospitals having the lowest mortality rate (1.3%) (p<0.001). Mortality did not differ by type of hospital ownership (p=0.49). Of the 10 principal forms of payment, Medicare patients had significantly higher mortality (3.6%) than patients with other insurers – e.g., Medicaid (2.0%), HMO/PPO (1.4%), and self-pay (1.0%) (p<0.001).
Mortality did not differ by type of admission (emergency n=18,382; urgent n=4,287; and elective n=1,729). Elective patients had a mortality rate of 2.8%, emergency 2.1%, and urgent 1.8% (p=0.06). The hospitals in the Midwest had a lower mortality rate (1.6%) compared to the Northeast (2.5%), South (2.2%), and West (2.4%) (p=0.002).
Multivariable logistic regression (MLR) analysis was used to identify independent predictors of mortality. Predictors entered into the MLR equation were: age, sex, race (white, African-American, other), comorbidities (3 or fewer, 4 or more), admission type (emergency, urgent, elective), hospital length of stay, hospital region (Midwest, other 3 regions), hospital size (99 or fewer beds, 100 or more beds), hospital ownership (proprietary, government, church/nonprofit), and principal payment (Medicare, 9 other insurers)
Table 2 shows the six independent risk factors. The highest adjusted odds ratio (AOR) was four or more comorbidities (AOR=15.22 [95% CI=4.87-47.54]; p<0.001), followed by hospital size of 100 beds or more (AOR=1.42 [95% CI=1.04-1.95]; p=0.029), Midwest region (AOR=1.31 [95% CI=1.05-1.64]; p=0.017), male sex (AOR=1.26 [95% CI=1.05-1.52]; p=0.015), increasing age (AOR=1.03 [95% CI=1.03-1.04]; p<0.001), and longer hospital LOS (AOR=1.03 [95% CI=1.02-1.03]; p<0.001).
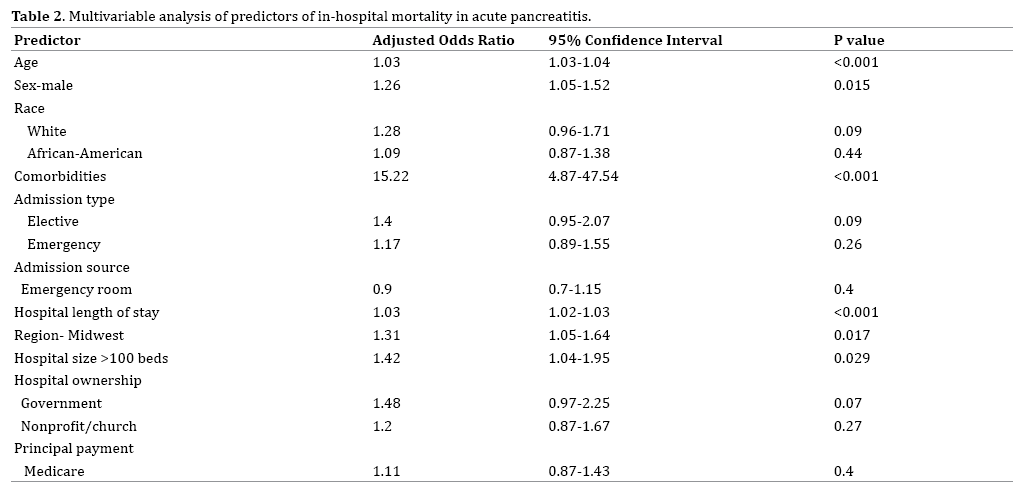
Using the National Hospital Discharge Survey (NHDS) database, we identified six independent risk factors of in-hospital mortality in acute pancreatitis patients: four or more comorbidities, larger hospital size, treatment outside the Midwest region, male sex, older age, and longer hospital length of stay.
Our finding that AP patients with four or more comorbidities are at increased risk of mortality is in agreement with earlier studies [15, 16, 17]. Singh et al. found a number of associations between various comorbid conditions and mortality in patients with interstitial pancreatitis [15]. Frey et al. reported that an increasing number of chronic comorbidities were associated with higher morality for acute pancreatitis [16]. These authors also noted that older patients were more likely to die during their hospitalization with AP. An epidemiological study conducted in Japan found that patients older than 70 years with severe comorbidities (>3 comorbid conditions) had twice the risk of in-hospital mortality [17]. Also, Murata et al. showed that cardiovascular and renal diseases are factors that increase hospital length of stay and mortality among AP patients [14]. With more comorbid conditions, patients increase their likelihood of developing end organ damage [18]. In our study, patients in the in-hospital mortality group had a longer LOS. However, due to multiple pre-existing comorbidities, those with longer LOS may have had more complications. Others have found that in-hospital mortality was higher in obese patients [19].
We found that in-hospital mortality varied by geographical location. Midwestern states had a lower mortality rate compared to Southern, Western, and Northeastern states. These regional differences amongst hospitals may be related to demographic (e.g., age), clinical (e.g., obesity, number of comorbidities), and socioeconomic (e.g., poverty) factors, population size, and number of medical facilities per capita.
The scoring systems currently utilized to predict mortality in patients with acute pancreatitis are often inconvenient to calculate and do not facilitate efficient triaging. Investigators have used serum markers and radiological findings to predict AP severity and mortality. To our knowledge, no prior research has used the NHDS database to examine demographic factors, comorbidities, and health care system characteristics that may be related to in-hospital mortality in patients with acute pancreatitis.
While type of hospital ownership (proprietary, government, or owned by a non-profit organization or church) had similar rates of in-patient mortality, smaller hospitals had lower mortality rates. Smaller hospitals may manage primarily milder cases of acute pancreatitis with patients having severe pancreatitis and related complications transferred to large facilities more capable of handling critically ill patients. Future investigations of facility transfer related to pancreatitis may reveal why mortality is lower in smaller hospitals.
Additionally, patients with Medicare as their primary insurance had higher in-hospital mortality compared to other forms of payment. However, the Medicare/ mortality relationship found with the univariate analysis was not significant in the multivariable model. As mentioned earlier, unfavorable demographic, clinical, and socioeconomic factors may be more prevalent in Medicare patients than with those having commercial and private insurance coverage.
Mortality among elective and emergency admissions was marginally higher than urgent admissions, but neither hospitalization for elective or emergency reasons was an independent predictor when urgent admission was used as the reference standard. Emergency admissions receive aggressive treatment and higher acuity of care once admitted in comparison to those admitted electively. Without access to individual patient data, we were not able to examine clinical characteristics that might be related to the type of admission.
Our study has several limitations. First, only non-federal hospitals were included in the National Hospital Discharge Survey database; thus, generalizability to Veterans Affairs medical centers and other institutions should be done with caution. Second, the NHDS database included readmissions for acute pancreatitis; thus, the unit of analysis for the study was events of AP and not independent patients with AP. Finally, the NHDS data did not include lab values, treatment choices, or longitudinal follow-up information; thus, the impact of clinical characteristics could not be examined.
Our analysis of National Hospital Discharge Survey data shows that demographic factors (sex and age), clinical characteristics (comorbidities, length of stay), and features of the health care system (geographic location, hospital size) may be utilized as predictors of in-patient mortality for those diagnosed with acute pancreatitis. Future research may identify other predictors of mortality that would improve the scoring systems now used with acute pancreatitis patients. As more research is conducted, a more accurate, less cumbersome, and easily calculated scoring system may be developed aiding in the reduction of in-hospital mortality in patients with acute pancreatitis.
We declare that we have no conflict of interests.