Noel M Manga1,2*, Viviane MP Cisse-Diallo1, Ndeye M Dia-Badiane1, Sylvie A Diop-Nyafouna1, Desire ER Ngoma Yengo1, Cheikh T Ndour1, Papa S Sow1, Yémou Dieng3, Moussa Seydi1 and Pierre M Girard4
1Department of Infectious and Tropical Diseases, University Hospital Fann, Avenue Cheikh Anta Diop BP 535 Dakar, Senegal
2Unit 2 Training and Research in Health Sciences (URF2S), University Assane Seck, BP 523 Ziguinchor (UASZ), Senegal
3Laboratory of Parasitology and Mycology, University Hospital Fann, Avenue Cheikh Anta Diop BP 535 Dakar, Senegal
4Department of Infectious Diseases, Hospital Saint Antoine, Paris, France
Corresponding Author:
Noel M Manga
Department of Infectious and Tropical Diseases, University Hospital Fann
Avenue Cheikh Anta Diop BP 535 Dakar, Senegal
Tel: 221776455609
Fax: 221339916809
E-mail: noel.manga@univ-zig.sn
Received date: June 21, 2016; Accepted date: June 26, 2016; Published date: June 30, 2016
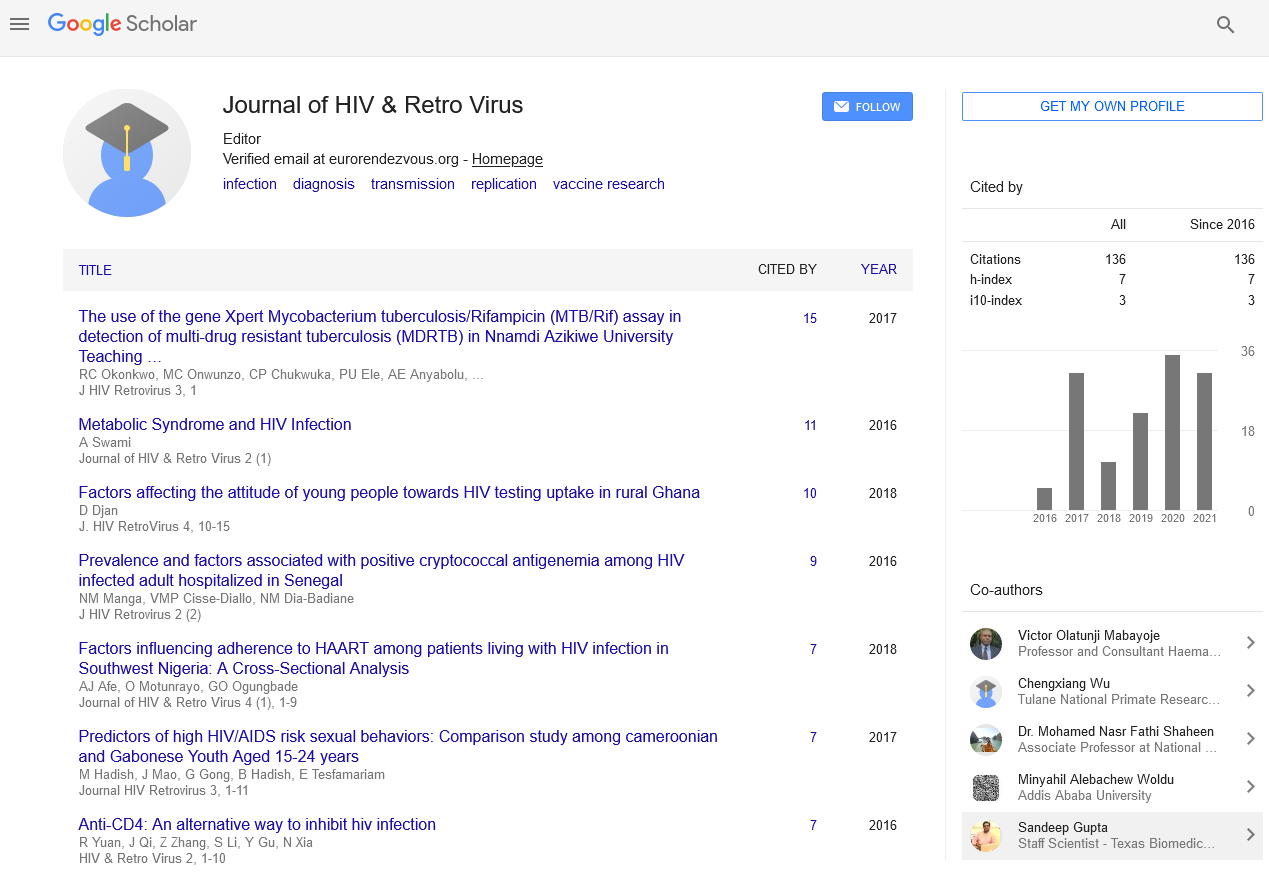
Citation: Manga NM, Cisse-Diallo VMP, Dia-Badiane NM, et al. Prevalence and Factors Associated with Positive Cryptococcal Antigenemia among HIV Infected Adult Hospitalized in Senegal. J HIV Retrovirus 2016, 2:2.
Copyright: © 2016 Manga NM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Cryptoccocal antigenemia; HIV; Sub-Saharan Africa
Abbreviation
HIV: Human Immunodeficiency Virus; CrAG: Cryptococcal Antigenemia; LTCD4+: Lymphocytes T CD4+; CSF: Cerebrospinal Fluid, ARV: Antiretroviral; ART: Antiretroviral Therapy
Introduction
Cryptococcosis is a systemic fungal infection, responsible for causing neuro meningeal in people with HIV and other immune compromised patients. It causes over 600 000 deaths annually in the world, especially in tropical areas [1,2]. This condition has become the first confirmed neurological opportunistic infection in patients living with HIV, in the infectious diseases clinic of Fann teaching hospital in Senegal [3]. The lethality of this disease remains high in patients admitted to this clinic, as in many African countries [2,4]. This high mortality is due in part to delayed diagnosis [2,4]. Cryptococcal antigen may be detectable in the blood, several weeks to several months before the onset of clinical symptoms of cryptoccosis [5]. The screening of cryptococcal antigenemia (CrAG) in patients at risk, allows early identification of asymptomatic or mildly symptomatic cases [1,6]. A positive CrAG may conduct to more frequent monitoring or preventive treatment of asymptomatic cases [1,5]. This study aims to determine the prevalence and factors associated with positive CrAG in patients with HIV infection hospitalized in a teaching hospital in West Africa.
Materials and Methods
We conducted a cross-sectional study in the clinic of infectious and tropical diseases of Fann national teaching hospital located in Dakar, Senegal. This study was realized among patients admitted during the period between November 1, 2009 and October 31, 2013. We included in this study all HIV infected patients, older than 15 years and for whom a CrAG test was performed.
Parasitological analyses were performed in the laboratory of parasitology and mycology of the same hospital. Cryptococcal antigenemia or serum cryptococcal antigen was detected using a latex agglutination test (PASTOREXTM CRYPTO PLUS) following the manufacturer's instructions. The specimen was heat-inactivated (30 min at 56°C) to eliminate the risk of HIV contamination. Before the test an enzymatic treatment of all samples was performed in order to eliminate interferences and enhance detection sensitivity. After preparation, the agglutination card was placed on the shaker for 5 min at 160 rpm, at a room temperature. A positive reaction was indicated by an agglutination of the latex with the test sample. The CSF (cerebrospinal fluid) was examined for research of antigen with the same technique. A direct examination after India ink staining was also performed in CSF samples.
Epidemiological, clinical and paraclinical data were collected from the patients folders. Data was collected using a standard questionary including epidemiological information (age, sex, geographic origin), clinical aspects (history, neurological signs and other signs), paraclinical results (cryptococcal antigenemia, cryptococcal antigen in CSF, staining ink, blood count and lymphocyte T CD4+ count), treatment and outcome aspects (ARV and administered antifungal, evolution).
All analyses were performed using SPSS.16 (California, USA, 2007). Medians and frequencies (%) were used to describe patients' characteristics. Fisher's exact test was used to compare categorical variables where appropriate Student's test was performed to assess the differences between two means. Binary logistic regression was used to determine factors associated with positive cryptococcal antigenemia. A p-value ≤ 0.05 was considered significant.
This study was conducted with the authorization of the responsible of the infectious diseases clinic in Fann teaching hospital. The study protocol was approved for routine analyses by the institutional review boards of Fann teaching Hospital in Dakar and Cheikh Anta Diop University. An anonymity number was given to each patient to preserve the confidentiality. Personal data from participant and all diagnostic results were kept strictly confidential.
Results
During the period of study, a total of 4346 patients infected by HIV were admitted in the service. A cryptococcal antigenemia was performed for 541 patients. Fifty cases of positive cryptococcal antigenemia were confirmed, meaning a prevalence of 9.2%. The different characteristics of our study population and our groups of patients depending on the result of antigenemia are described in (Table 1).
| Parameters |
Cryptococcal antigenemia Positive n=50 |
Negative n=491 |
Total n=541 |
| |
n (%) |
n (%) |
n (%) |
| Sex |
| Male |
20 (40) |
216 (44) |
236 (43.6) |
| Female |
30 (60) |
275 (56) |
305 (56.4) |
| Age (years) |
| 15-30 |
5 (10) |
87 (17.7) |
92 (17) |
| 31-45 |
25 (50) |
237 (48.3) |
262 (48.4) |
| >45 |
20 (40) |
167 (34) |
187 (34.6) |
| Residence |
| Urban |
24 (48) |
215 (43.8) |
239 (44.2) |
| Suburban |
21 (42) |
215 (43.8) |
236 (43.6) |
| Rural |
5 (10) |
47 (9.6) |
52 (9.6) |
| Unspecificated |
0 (0) |
14 (2.8) |
14 (2.6) |
| Clinical signs |
| Fever |
48 (96) |
398 (81) |
446 (82.5) |
| Headache |
26 (52) |
106 (21.6) |
132 (24.4) |
| Confusion |
10 (20) |
46 (9.4) |
56 (10.3) |
| Coma |
14 (28) |
79 (16.1) |
94 (17.2) |
| Meningeal signs |
19 (38) |
56 (11.4) |
75 (13.9) |
| Intracranial hypertension |
0 (0) |
6 (1.2) |
6 (1.1) |
| Seizures |
11 (22) |
20 (4) |
31 (5.7) |
| Motor deficit |
8 (16) |
30 (6.1) |
38 (7) |
| Cranial nerve disorders |
4 (8) |
14 (2.8) |
18 (3.3) |
| Cough |
26 (52) |
250 (50.9) |
276 (51) |
| Diarrhoea |
18 (36) |
126 (25.7) |
144 (26.6) |
| HIV serotype |
| HIV-1 |
43 (86) |
454 (92.5) |
497 (91.9) |
| HIV-2 |
03 (6) |
25 (5.1) |
28 (5.2) |
| HIV-1 +2 (Dual) |
01 (2) |
10 (2) |
11 (2) |
| Unspecified |
03 (6) |
2 (0.4) |
5 (0.9) |
| LT CD4+ (cells/mm3) |
| 0-150 |
36 (72) |
337 (68.6) |
373 (68.9) |
| 151-300 |
03 (6) |
43 (8.8) |
46 (8.5) |
| >300 |
05 (10) |
37 (7.5) |
42 (7.8) |
| Unspecified |
06 (12) |
74 (15.1) |
80 (14.8) |
| Antiretroviral therapy |
| Yes |
21 (42) |
160 (32.6) |
181 (33.5) |
| No |
29 (58) |
331 (67.4) |
360 (66.5) |
Table 1: Characteristics of hospitalized HIV patients screened for cryptoccocal antigenemia in Dakar, Senegal.
Epidemiological aspects
The predominance of female patients was noted in our study population with a sex ratio of 0.77. The average age was 42 ± 11years and patients ranged from 31 to 45 years The predominance of female patients was noted in our study population with a sex ratio of 0.77. The average age was 42 ± 11years and patients ranged from 31 to 45 years.
Clinical aspects
The past history was dominated by chronic diarrhea (18.6%), tuberculosis (17.6%) and meningeal cryptococcosis (0.7%). High blood pressure (6.4%), asthma (3.1%) and diabetes (2.1%) were the major associated underlying diseases. The majority of patients (95%) were at stages 3 or 4 of WHO. Fever, present in 82.5% of cases, was more frequent in patients with positive antigenemia. The prevalence of neuromeningeal signs ranged between 1% to 14%. They predominated in patients with positive cryptococcal antigenemia.
The extra-neurological manifestations were dominated by coughing and chronic diarrhea.
Paraclinical aspects
HIV-1, the predominant serotype, was found in over 85% of cases in the 2 groups. The average LTCD4 + was 102 ± 165 cells/mm3 (IQ:1 and 1704 cells/mm3). The CSF analysis was performed in 142 patients. Cryptococcal antigen screening in the CSF was positive for 17 cases (12%) and India ink staining was positive in 9 cases (6.3%). Confirmation in CSF was performed in 11cas (50%) among 22 patients with positive antigenemia, but only 6 cases were confirmed (5%) among 120 patients with a negative antigenemia (p=0.0000006).
Factors significantly associated with positive cryptococcal antigenemia were (Table 2): having a history of cryptococcal meningitis (p=0.002) and presenting headache (p=0.000008), altered consciousness (p=0.001), meningeal signs (p=0.000005).
| Parameters |
CrAG Positive |
Negative |
OR |
IC 95% |
p-value |
| |
n (%) |
n (%) |
|
|
|
| Age (years) n=541 |
| 15-45 |
30 (60) |
324 (66) |
0.7 |
0.4-1.4 |
0.2 |
| >45 |
20 (40) |
167 (34) |
|
|
|
| Sex n=541 |
| Male |
20 (40) |
216 (44) |
0.8 |
0.4-1.5 |
0.3 |
| Female |
30 (60) |
275 (56) |
|
|
|
| History of cryptococcosis n=541 |
| Yes |
3 (6) |
1(0.2) |
8 |
4.5-16 |
0.002 |
| No |
47 (94) |
490 (99.8) |
|
|
|
| Fever n=541 |
| Present |
22 (44) |
210 (42.8) |
1 |
0.6-1.8 |
0.5 |
| Absent |
28 (56) |
281 (57.2) |
|
|
|
| Headaches n=541 |
| Present |
26 (52) |
106 (21.6) |
3.9 |
2.1-7.2 |
0.000008 |
| Absent |
24 (48) |
385 (78.4) |
|
|
|
| Meningeal signs n=541 |
| Present |
19 (38) |
56 (11.4) |
4.7 |
2.5-8.9 |
0.000005 |
| Absent |
31 (62) |
435 (88.6) |
|
|
|
| Altered consciousness n=541 |
| Present |
24 (48) |
125 (25.4) |
2.7 |
1.5-4.9 |
0.001 |
| Absent |
26 (52) |
366 (74,6) |
|
|
|
| LT CD4+ count (c/mm3) n=458 |
| Jan-50 |
25 (55.6) |
201 (48.7) |
1.2 |
0.4-2.2 |
0.3 |
| >50 |
20 (44.4) |
212 (51.3) |
|
|
|
| Antiretroviral therapy n=541 |
| Yes |
21 (42) |
160 (32.6) |
1.5 |
0.8-2.7 |
0.1 |
| No |
29 (58) |
331 (67.4) |
|
|
|
Table 2: Factors associated with a positive cryptococcal antigenemia among hospitalized HIV patients in Dakar, Senegal.
Therapeutic and outcome aspects
Patients on antiretroviral therapy (ART) represented 33.5% of the study population and their prevalence was higher in the case of positive antigenemia (42%) than in the case of negative antigenemia (32.6%). Fluconazole (800-1200 mg/day per os) was administered to all positive cryptococcal antigenemia cases.
Overall mortality was 34.1%. This mortality was higher in positive antigenemia cases (46%) compared to patients with negative antigenemia (32.8%); p=0.08.
Discussion
Cryptococcal meningitis is a serious opportunistic infection. It most often occurs in severely immunosuppressed patients especially during HIV infection. The incidence of cryptococcosis has increased significantly all over the word with the advent of HIV infection, especially in developing countries [1,2,7]. Cryptococcal meningitis became the leading cause of adult neurological opportunistic infection in many African countries [3,7]. There is a great need of prophylaxis strategies and one of them is based in the screening of CrAg.
The prevalence of positive cryptococcal antigenemia in our study is 9.2%. A high diversity of cryptococcal antigenemia prevalence was noted in sub-Saharan Africa ranging from 2% to 21% [1,6,8].
Many studies in African countries showed comparable prevalence ranging from 7 to 10%: in Tanzania [9] and South Africa 7% [10], in Uganda 8.2% [11], in Ethiopia 8,4% [6].
In the same country the prevalence can depend on the targeted population. In a cohort of ART-naive patients in a rural area in Tanzania, Letang et al. detected 3.7% of positive cryptococcal antigenemia, while Magambo in a hospital of Mwanza had a prevalence of 7% [9,12]. In Uganda Andama noted a prevalence of 5.7% in patients hospitalized for suspected tuberculosis in a hospital of Kampala, but Oyella detected in the same hospital 19% of CrAG in inpatients and outpatients [13,14]. The same situation was noted in Ethiopia with a prevalence of 8.4% and 10.2% in two studies including patients receiving ART or not [6,15].
In Asia the same situation was noted in Vietnam with a global prevalence of 4%, higher in patients living in the south [16]. The prevalence in hospitalized patients was 13% in Thailand, and 11% for women attending a centre of ART [17,18]. A study in Indonesia noted 7% of positive CrAG in a referral hospital from in-and outpatients [19].
In Europe, a prevalence of 5% was noted in a cohort of London, but almost all positive cases were from Africa [20]. A prevalence of 1.6% was noted in Germany [21].
A history of cryptococcal meningitis was found in 0,7% of our patients. A study in Thailand revealed cryptococcal meningitis in the past year for 8,6% [17]. Tuberculosis, the first opportunistic infection in the history of our cases, was confirmed as the leading associated opportunistic infection of positive CrAG cases by some authors [13,17].
Cryptoccocal meningitis was confirmed on cerebrospinal fluid analysis for 34% of our patients with positive CrAG. Similar result was noted by Oyella et al in Ethiopia [14]. Cryptococcal meningitis occurred in 39% of CrAG positive patients and an antigen titer>1:160 was associated with meningitis development in a Tanzanian study [12].
Antigenuria test was not as concluent in a study [13], but blood culture detected Cryptococcus neoformans in 48% of positive CrAG patients in another work [17].
We did not found a higher prevalence in patients with CD4 count<150 cells/ml. But in many studies the prevalence was more important in people with a CD4 count <100 to 150 cells/ml [6,13,15,17,21].
Factors significantly associated with a positive cryptococcal antigenemia in our patients were clinical: the presence of neurological signs such as headache, altered consciousness and meningeal signs. The same findings were noted by some auteur [6,14,21].
Different others factors were found to be associated with a positive CrAG in many others studies: increasing age, fever, CD4 count<100 cells/ml, the site of screening, low body mass index of 15.4 kg/m2 or less, ART-naive and ART-defaulters patients [6,14,15,21]. In Thailand only dyspnea was significantly associated to CrAG+ in patients admitted for pneumonia [17].
These findings suggest that symptoms alone are insufficient criteria to determine which patient to test for CrAG [17]. A systematic CrAG screening would be a cost-effective strategy to prevent CM-related mortality among patients initiating ART in South Africa for Jarvis [22]. Others auteur (a film director who influences their films so much that they rank as their author.) sustain that CrAG testing should be consider in hospitalized patients or people with a LTCD4+ count ≤ 100 cells/ml [10,13,16,17].
Many studies found that positive asymptomatic CrAG is associated to a poor outcome including cryptococcal meningitis development, death and loss of follow up [12,18,19].
Pre-emptive treatment of positive asymptomatic CrAG patients may improve this poor outcome [12,23]. But lowdose fluconazole prophylaxis has a poor efficacy in preventing cryptococcal meningitis among patients with positive antigenemia [18].
There is a need for more research studies to better understand the signification of asymptomatic CrAG and practical implication of this condition [1].
Conclusion
The prevalence of positive CrAG is high in hospitalized HIV infected patients in our practice. The serum cryptococcal antigen test would be systematic in all HIV patients presenting these signs. Giving the poor prognostic of positive asymptomatic CrAG in many studies, we suggest a systematic screening of CrAG in all HIV patients if possible. It is associated with neurological and meningeal signs.
Declaration
This study was conducted with the authorization of the responsible of the infectious diseases clinic in Fann teaching hospital. The study protocol was approved for routine analyses by the institutional review boards of Fann teaching Hospital in Dakar and Cheikh Anta Diop University. An anonymity number was given to each patient to preserve the confidentiality. Personal data from participant and all diagnostic results were kept strictly confidential.
Acknowledgement
ESTHER (Together for Therapeutic Solidarity Network) and Fann Senegal: A French network for HIV patient’s care who provided a support for cryptococcal antigenemia testing. Dr. Doudou Sow and the technicians of the Laboratory of Parasitology and Mycology of Fann for their technical support
Funding
ESTHER (Together for Therapeutic Solidarity Network) and Fann Senegal provided a support for cryptococcal antigenemia testing. But we have no funding for the publication of this article.
Competing Interests
The authors declare that they have no competing interests.
Authors' Contributions
MNM* conceived the study and contributed to all the steps of the study, C-DVMP has made substantial contributions for analysis and interpretation of data, DERNY have contributed for acquisition of data, or analysis and interpretation of data; D-BNM and D-NSA participated to the drafting and the revising of the manuscript, DY has organized the tests performing, and CTN, SM gave important intellectual contribution for the revision of the final version. All authors read and approved the final manuscript.
References
- Alemu AS, Kempker RR, Tenna A, Smitson C, Berhe N, et al. (2013) High prevalence of cryptococcal antigenemia among HIV-infected patients receiving antiretroviral therapy in Ethiopia. PLoS ONE 8: 58377.
- Andama AO, den Boon S, Meya D, Cattamanchi A, Worodria W, et al. (2013) Prevalence and outcomes of cryptococcal antigenemia in HIV-seropositive patients hospitalized for suspected tuberculosis in Uganda. J Acquir Immune Defic Syndr 63: 189-194.
- Beyene T, Woldeamanuel Y, Asrat D, Ayana G, Boulware DR (2013) Comparison of cryptococcal antigenemia between antiretroviral naïve and antiretroviral experienced HIV positive patients at two hospitals in Ethiopia. PLoS ONE 8: 75585.
- Butler EK, Boulware DR, Bohjanen PR, Meya DB (2012) Long term 5 year survival of persons with cryptococcal meningitis or asymptomatic subclinical antigenemia in Uganda. PLoS ONE 7: 51291.
- Desalermos A, Kourkoumpetis TK, Mylonakis E (2012) Update on the epidemiology and management of cryptococcal meningitis. Expert Opin Pharmacother 13: 783-789.
- Ganiem AR, Indrati AR, Wisaksana R, Meijerink H, van der Ven A, et al. (2014) Asymptomatic cryptococcal antigenemia is associated with mortality among HIV-positive patients in Indonesia. J Int AIDS Soc 17: 18821.
- Harris JR, Lindsley MD, Henchaichon S, Poonwan N, Naorat S, et al. (2012) High prevalence of cryptococcal infection among HIV-infected patients hospitalized with pneumonia in Thailand. Clin Infect Dis 54: e43-50.
- Jarvis JN, Harrison TS, Lawn SD, Meintjes G, Wood R, et al. (2013) Cost effectiveness of cryptococcal antigen screening as a strategy to prevent HIV associated cryptococcal meningitis in South Africa. PLoS ONE 8: 69288.
- Jarvis JN, Lawn SD, Vogt M, Bangani N, Wood R, et al. (2009) Screening for cryptococcal antigenemia in patients accessing an antiretroviral treatment program in South Africa. Clin Infect Dis 48: 856-862.
- Katchanov J, Jefferys L, Tominski D, Wöstmann K, Slevogt H, et al. (2015) Cryptococcosis in HIV-infected hospitalized patients in Germany: Evidence for routine antigen testing. J Infect 71: 110-116.
- Kwan CK, Leelawiwat W, Intalapaporn P, Anekthananon T, Raengsakulrach B, et al. (2014) Utility of cryptococcal antigen screening and Evolution of asymptomatic cryptococcal antigenemia among HIV-infected women starting antiretroviral therapy in Thailand. J Int Assoc Provid AIDS Care 13: 434-437.
- Letang E, Müller MC, Ntamatungiro AJ, Kimera N, Faini D, et al (2015) Cryptococcal antigenemia in immunocompromised human immunodeficiency virus patients in rural, Tanzania: a preventable cause of early mortality. Open Forum Infect Dis.
- Magambo KA, Kalluvya SE, Kapoor SW, Seni J, Chofle AA, et al. (2014) Utility of urine and serum lateral flow assays to determine the prevalence and predictors of cryptococcal antigenemia in HIV-positive outpatients beginning antiretroviral therapy in Mwanza, Tanzania. J Int AIDS Soc 17: 19040-45.
- Mamoojee Y, Shakoor S, Gorton RL, Sarfo S, Appiah LT, et al. (2011) Short communication: Low seroprevalence of cryptococcal antigenaemia in patients with advanced HIV infection enrolling in an antiretroviral programme in Ghana. Trop Med Int Health 16: 53-56.
- Meya DB, Manabe YC, Castelnuobo B, Cook BA, Elbireer AM, et al. (2010) Cost-effectiveness of serum cryptococcal antigen, screening to prevent deaths among HIV-Infected persons with a CD4+ Cell Count? 100 cells/ml who start HIV therapy in resource-limited settings. Clin Infect Dis 51: 448-455.
- Meyer AC, Jacobson M (2013) Asymptomatic cryptococcemia in resource-limited settings. Curr HIV/AIDS Rep 10: 254-263.
- Oyella J, Meya D, Bajunirwe F, Kamya MR (2012) Prevalence and factors associated with cryptococcal antigenemia among severely immunosuppressed HIV-infected adults in Uganda: A cross-sectional study. J Int AIDS Soc 15: 15-21.
- Patel S, Shin GY, Wijewardana I, Vitharana SR, Cormack I, et al. (2013) The prevalence of cryptococcal antigenemia in newly diagnosed HIV patients in a Southwest London cohort. J Infect 66: 75-79.
- Rajasingham R, Meya DB, Boulware DR (2012) Integrating cryptococcal antigen screening and pre-emptive treatment into routine HIV care. J Acquir Immune Defic Syndr 59: 85-91.
- Sloan DJ, Parris V (2014) Cryptococcal meningitis: Epidemiology and therapeutic options. Clin Epidemiol 6: 169-182.
- Smith RM, Nguyen TA, Ha HTT, Thang PH, Thuy C, et al. (2013) Prevalence of cryptococcal antigenemia and cost-effectiveness of a cryptococcal antigen screening program – Vietnam. PLoS One 8: 62213.
- Soumaré M, Seydi M, Ndour CT, Fall N, Dieng Y, et al. (2005) [Epidemiological, clinical, etiological features of neuromeningeal diseases at the Fann Hospital Infectious Diseases Clinic, Dakar (Senegal)]. Med Mal Infect 35: 383-389.
- Soumaré M, Seydi M, Ndour CT, Dieng Y, Diouf AM, et al. (2005) [Update on neuromeningeal cryptococcosis in Dakar]. Med Trop (Mars) 65: 559-562.