Introduction
It is not more than a decade for recognizing nutrition as “nutrition is many things”. The first well recognized high-level declaration “eliminate hunger and all forms of malnutrition within a decade” have been held in Rome Italy in 1992 after decades of suffering. But ensuring healthy nutrition for citizens has an irreplaceable role beyond satisfying a sense of hunger by improving human capital, reducing healthcare expenditure, boosting learning potential and competitiveness, increasing work task force, improving productivity, resolving threats for climatic change, environmental degradation, conflict and migration and achievement of broad national and global goals [1].
Currently, nearly 1 billion people were undernourished; 1 billion of them were already overweight and obese and almost 2 billion were suffering from hidden hunger globally. When basic, underlying and immediate causes of malnutrition are examined critically the issue of malnutrition if not limited to food shortage. It can be addressed if and only if there is a commitment, multilevel, multi-sectorial and multi-stakeholder responsibility and evidence-based intervention focusing on the undertaking of nutrition specific and nutrition-sensitive programs targeting on prevention, control and treatment of malnutrition but not by dumping quintals of refined, energy dense nutrient empty agricultural products [2].
Children are with high nutritional need but most vulnerable due to low social status, poor diet, and ill health and inappropriate care. In addition, children of rural smallholders and urban poor were also highly vulnerable to malnutrition due to inability to withstand the effect of the climatic change, volatile food price, globalization and global trade on nutrition [2]. About 255 million under-five children were suffering from malnutrition that impacts mortality, morbidity, impaired learning potential, and limited participation in individual affairs, community and national development and productivity agendas. The problem was propagated from various factors including food insecurity, lack of provision of care, limited access to health care services, inability access and utilizes commonest community resources like water and land [3]. Therefore this systematic review was based on the argument of “malnutrition is so much more that shortage of food” and has no one fit for all solution to treat, control and prevention: evidence-based intervention is urgent and mandatory.
Objective of the Review
The objective of this systematic review and meta-analysis of literature was determining the prevalence and major contributors of under-five children malnutrition in developing countries in addition to visible food shortage and food insecurity.
Method and Materials
Materials
A nine-item new castle–Ottawa quality assessment tool was used to assess and appraise the quality of eligible articles for this systematic review. We used excel spreadsheet for extraction of data for meta-analysis and Meta-regression. Heterogeneity test, publication bias test, meta-analysis, subgroup analysis and metaregression were fitted using the Stata 11 software.
Inclusion Criteria
All primary research articles and national and international reports published on under-nutrition, obesity, and overweight between 2006 to 2016 on under five years children and reporting either form of malnutrition were included for this systematic review and Meta-analysis.
Search Strategy
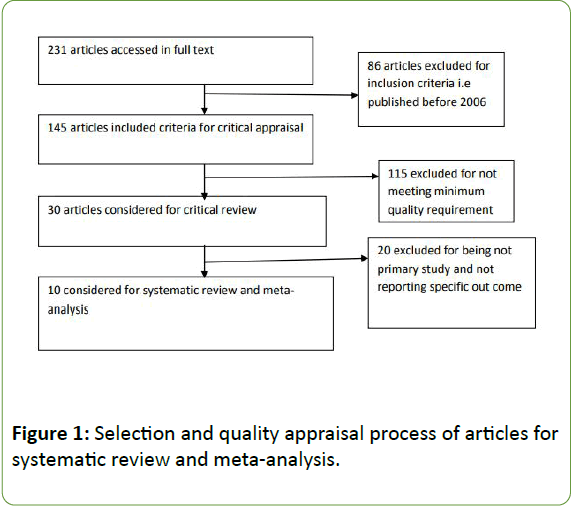
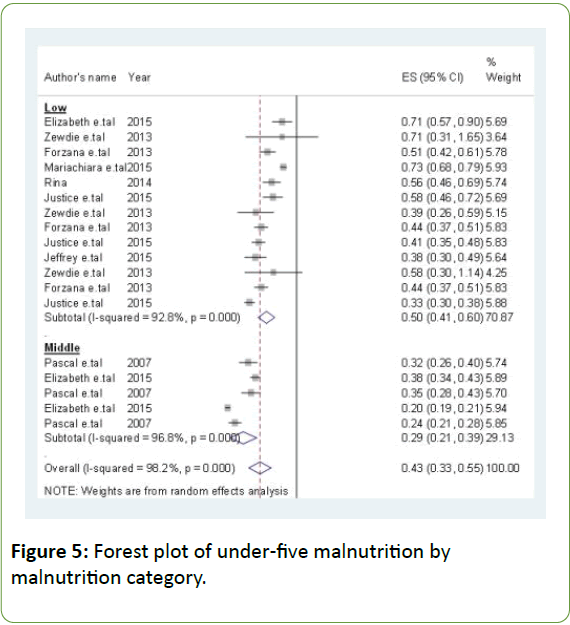
To archive reports and articles for this systematic review, we have searched evidence from PUBMED, EMBASE, and Google Scholar by using keywords of malnutrition, under-nutrition, acute malnutrition, chronic malnutrition, underweight, overweight, and obesity. During searching of PUBMED, we used (MeSH) [1] to search medical subject headings, (MESH) [2] to look up abstract and title and (MeSH) to combine [1] with [2] using Boolean logic (Figure 1).
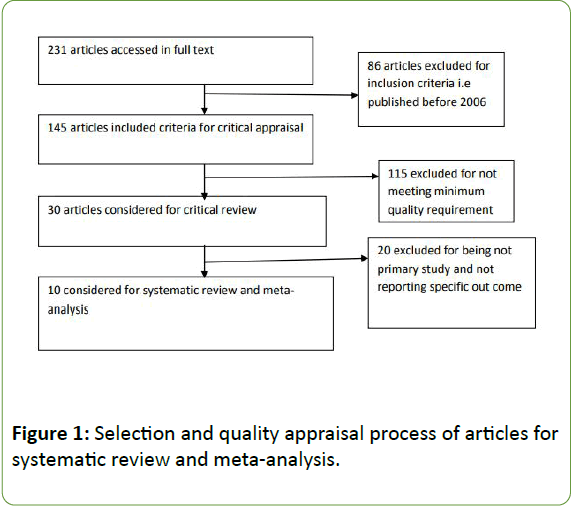
Figure 1: Selection and quality appraisal process of articles for systematic review and meta-analysis.
Results
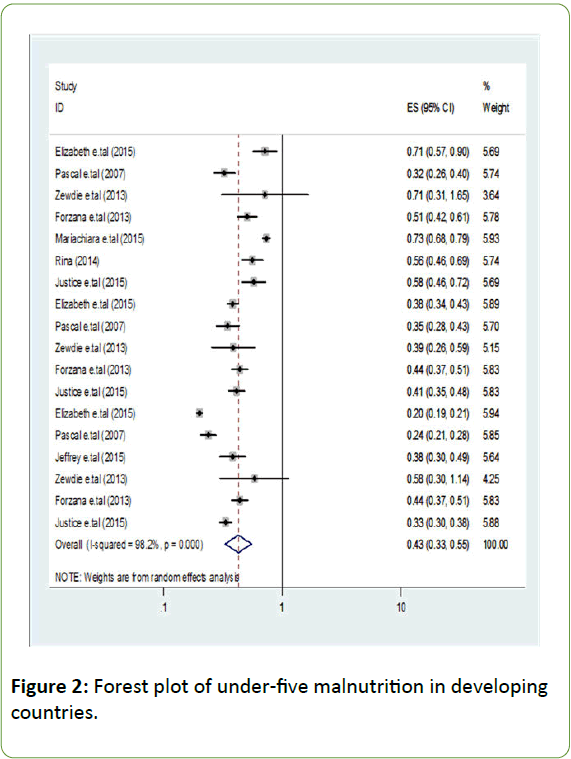
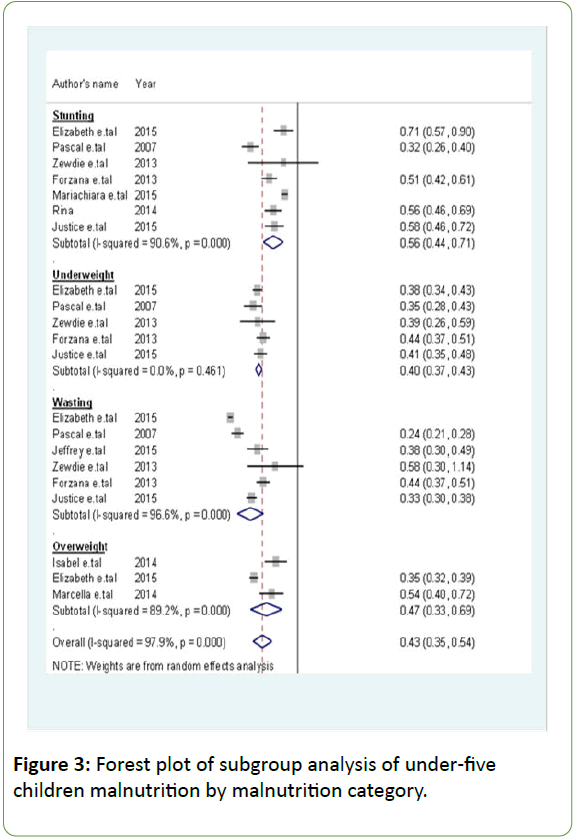
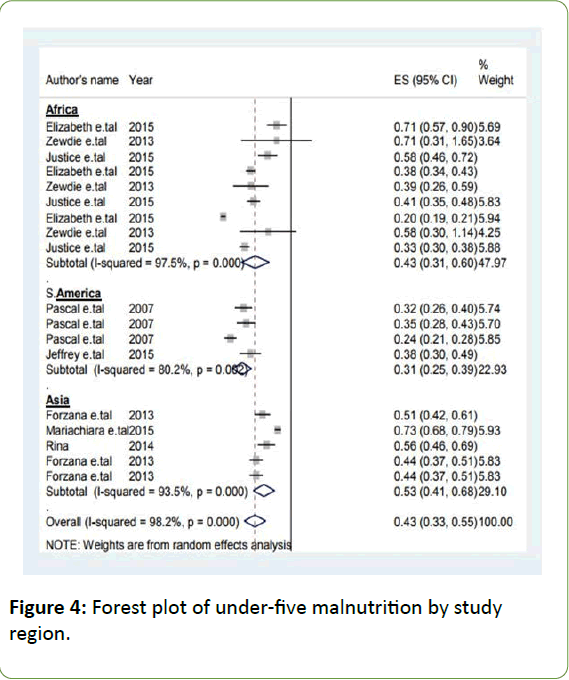
About ten articles were included in this systematic review and meta-analysis that scored at least three New Castle-Ottawa critical appraisal points. Among included articles five had reported stunting, underweight and wasting, one study had reported stunting and overweight, two reported only stunting and the rest two had reported only overweight. We run Metaanalysis which demonstrated high heterogeneity between studies. Heterogeneity between studies was high in subgroup analysis and meta-regression by the fitting of fixed and random effect model; we differed to systematic review only. Even though it is not possible to estimate the average due to high heterogeneity the prevalence of malnutrition was between 21% and 71% (Figures 2-5).
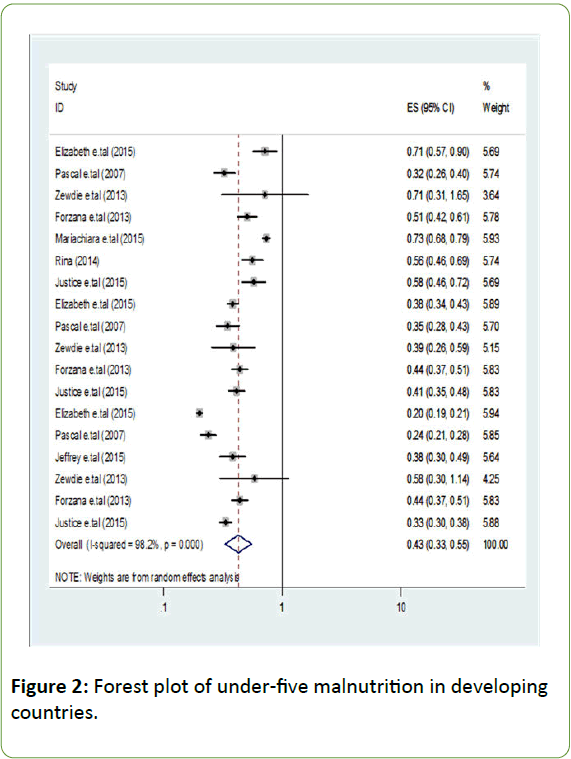
Figure 2: Forest plot of under-five malnutrition in developing countries.
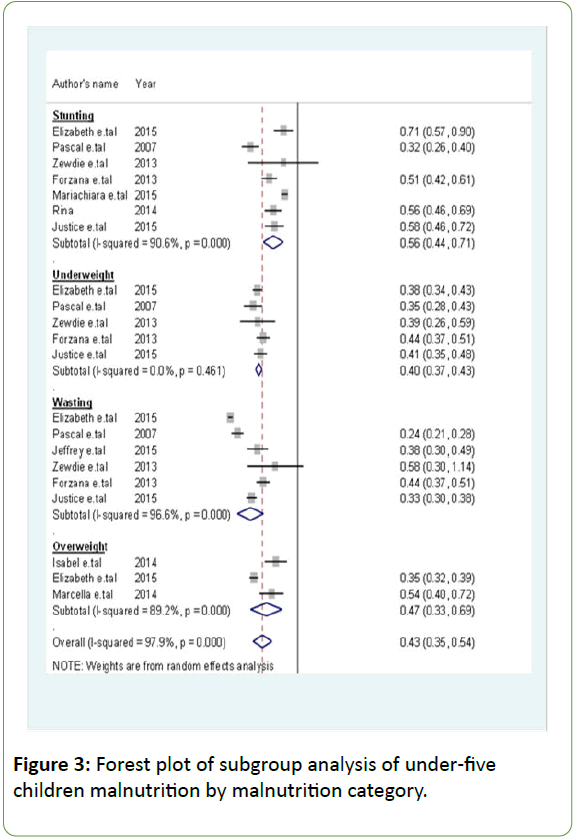
Figure 3: Forest plot of subgroup analysis of under-five children malnutrition by malnutrition category.
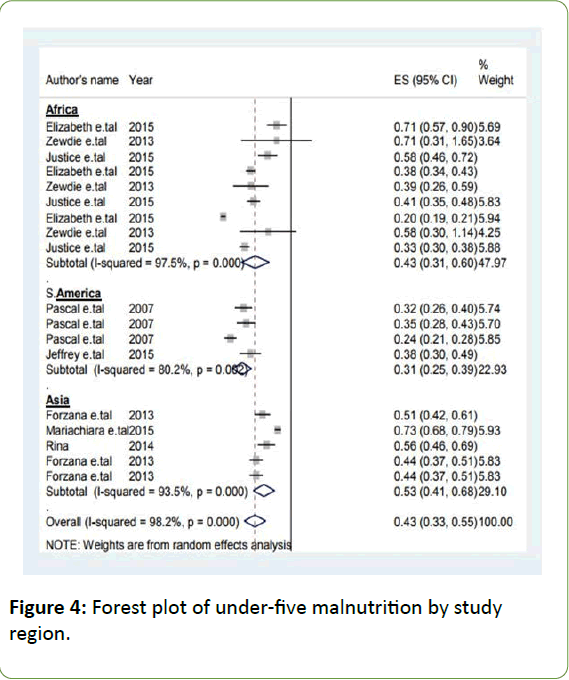
Figure 4: Forest plot of under-five malnutrition by study region.
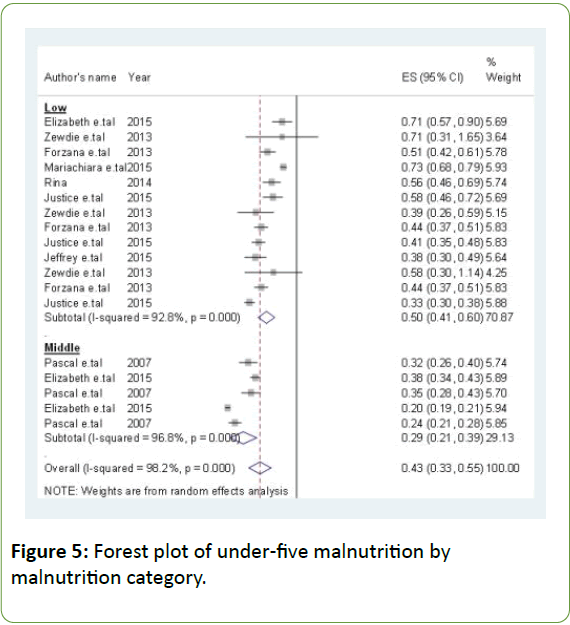
Figure 5: Forest plot of under-five malnutrition by malnutrition category.
Discussion
Malnutrition is so much more than Shortage of Food and Food Insecurity
Migration, household composition and greater distance from food store were associated factors with food insecurity and food shortage [4]. The issue of malnutrition is not only limited to the shortage of agricultural yield or its availability. Review of literature had indicated accessibility, utilization, and sustainability as important dimensions for malnutrition to be addressed. Those with the above characteristics were more vulnerable to malnutrition due to accessibility, utilization, and sustainability problems in addition to the availability of food. Borrowing money, sharing food, and relying on family and community programming were qualitatively identified food insecurity coping strategies [5]. Such coping strategies were potential risks for under-five children malnutrition by affecting the quality, quantity, and diversity of food served for under-five children. On the other hand, there would be none or less spending for health and education that affects all dimensions of nutrition. Altering food purchasing and eating pattern, reducing an amount of adult meal, purchasing less expensive food and consuming expensive food less frequently were coping strategies food insecurity and food shortage [6]. Such strategy has effect on the quality, quantity, diversity, and safety of food to be served for the family members including children putting at risk of malnutrition and illness.
Sending household members to the rural area and incorporating additional members were also food insecurity coping strategies [7-10]. Both coping strategies have a great effect on malnutrition through reduced care, nutrition, emotional support, and separation could also make children more vulnerable to abuse, exploitation, and violation that worsens health and nutritional status. Annexation of an additional family member as food insecurity coping strategy exposes children to diarrheal and respiratory diseases related overcrowding and lack of hygiene a risk for child malnutrition. The absence of sewerage connection has had statistically associated with iron deficiency anemia and low anthropometric measurement among children [11]. Hygiene and sanitation problem can contribute to under-nutrition by increasing rate of parasitic and helminthic infection, altering consumption and increases expenditure and by increasing rate, frequency and severity of diarrheal diseases resulting loss of nutrients and electrolytes.
Severe acute malnutrition was coexisted with gastroenteritis among hospital admitted children [12]. Acute malnutrition can coexist with health disorders like gastroenteritis and HIV which usually manifested with diarrhea, abdominal pain, vomiting, and abdominal discomfort all resulting in reduced consumption, disturbed digestion, and distributed absorption and increases the loss of minerals and nutrients that attribute for child malnutrition. High prevalence of Plasmodium falciparum infection was positively associated with stunting [13]. Blood parasites may induce loss of appetite, make oral intake difficult during acute attack periods, increase the expenditure and make vulnerable to various infectious diseases that endanger the nutritional status of children.
Diarrhea, sepsis, bronchopneumonia, HIV, tuberculosis, scabies and otitis media were identified co-morbidities for children admitted to hospital due to protein-energy malnutrition [14,15]. All these have a negative effect on consumption, digestion, and absorption of menials and nutrients that increases the rate of expenditure and loss minerals and nutrients. Reduced weight gain was recorded with increased episode and duration of diarrheal and upper respiratory tract infection
Wasting can be a result of low consumption resulted from the suffering of diarrheal and respiratory symptoms and massive loss of minerals from diarrhea which increases with increased duration and episode.
Under-five under-nutrition was associated with food or water borne diseases [16,17]. Food and water-borne disease contribute for malnutrition by reducing consumption, increases loss and altered digestion and absorption of menials and nutrients due to disturbed integrity and function of the gastrointestinal system. Under-five children drinking water from sources of unprotected well, surface water, spring water and rainwater were with a high incidence rate of under-nutrition. Lack of sanitation and safe water supply are closely related to frequency and severity of acquiring of diarrhea, parasitic and helminthic diseases which have a direct and indirect effect on under-five malnourishment
Under-five children were risk group for a high rate of parasitic infection that simultaneously predisposes to malnutrition, hidden hunger, cognitive impairment and other chronic and acute infectious disease [18]. The absence of window screening material was shown as a predictor for reduced weight for weight [19]. Using bed net and window screening materials can reduce the risk of vector-borne diseases risks for acute malnutrition. Immunization status, illness, antenatal care, family size, the household source of water supply and availability of latrine facility were strong predictors of undernourishment among under-five children [20]. All of the above factors can have a direct effect on children’s nutritional status through altering child and maternal health, breastfeeding, dietary consumption and care of children in case if there is the alteration of the health of mothers of caretakers.
Obesity has physiological background [21]. Children born from malnourished mothers, short stature mothers, mothers affected by stress, obesity, and chronic disease were highly vulnerable to overweight and obesity at their childhood period that may be related to disproportional weight gain than gaining of height, increased intake of energy-dense nutrient-empty food and limited physical activity risk the extent of overweight and obesity. Non-optimal feeding practice, dietary diversity, breastfeeding problem, hygienic problem, inability to feed iron rich food were factors that worsen stunting [22]. All of these factors were closely related to maternal health and awareness which can be effectively address through improving maternal health and awareness during a period of pregnancy and breastfeeding in addition to ensuring food supply.
The prevalence of under-five malnutrition has a wide variability within and between regions [23]. Geographic and socioeconomic inequalities among mothers and children resulted from variability in malnutrition by limiting equitable utilization public service and reducing the capacity of withstanding difficult situations that could complicated health and nutritional problem mothers and under-five children. Low birth weight, preterm birth, multiple birth and multiparity were predictors for stunting, wasting and underweight [24]. All could affect the nutritional status of a child due to maternal health problem as it is being children of morbid, disabled or died mother were less or non-breast feed and receives less care and service which have the effect on nutritional status. Being a child of older mothers was one of the identified risk factors for stunting [25]. Older age was generally associated with the highest prevalence of chronic maternal diseases which generally related reduced household income, increased health expenditure for chronic illness and complication of pregnancy and childbirth, the difficulty of breastfeeding and provision of care that affects health and nutritional status of under-five children.
Mothers who are not covered by national health insurance are associated with increased risk of malnutrition [26]. Health insurance may have an effect on motivation and utilization of health care services during pregnancy and breastfeeding periods that may have a direct effect on under-five nutritional status through influencing breastfeeding, optimum child feeding practice, maternal and child health. Heavy workload during the third trimester, abuse during pregnancy, home delivery, less frequent ANC visit and non-utilization of postnatal service were a risk for child hold malnutrition [27]. Childhood nutritional status is highly dependent on maternal health and nutritional status that the above factors affect maternal health and nutrition which were also determinants of under-five children malnutrition.
Low weights at birth, no feeding of colostrum and children from families without social security were highly vulnerable for stunting [27]. Stunting is a form of under-nutrition indicating a chronic deprivation of health, nutrition and stimulating environment of a child and failure to attain various maternal services at pre-pregnancy, pregnancy and post-pregnancy period during breastfeeding and care of the child that intensify the nutritional status of under-five children. Children who consumed animal source food were less likely to be stunted and underweight [28]. However animal sources food was less accessible for the vulnerable group of the population particularly for under-five children related to cost and cultural factors.
Picky eaters tended to consume fewer cereals, vegetable, fish, dietary fiber, iron and zinc [29]. Picky eating behavior reduces the diversity of dietary intake by eating only picked food or diet. Egg, fruit, and vegetables are least consumed food groups than cereals, potato crisp, noncarbonated beverage, sweets and sugar-sweetened carbonated beverages [30]. If there was a disproportional intake of cereals, potato crisp, none carbonated beverage, sweets and sugar-sweetened carbonated beverages it worsens the state of obesity and overweight have immense consequences.
Lifestyle has resulted in the highest burden of obesity and obesity-induced chronic diseases [31]. Most Asian countries like India and China were facing the double burden of malnutrition related to food insecurity, the disparity in food intake, influx of western foods and presence of high intake of animal foods, sugar, and fates related to lifestyle change. Nutrition specific and nutrition-sensitive programs have a key role in addressing under-five malnutrition [32]. These programs are important to deal with intermediate and underlying causes of child malnutrition by addressing of adolescent, preconception and maternal health and nutrition, maternal dietary micronutrient supplementation, and promotion of optimum breastfeeding.
Micronutrient powders were effective in tackling of anemia and improving hemoglobin level among women [33]. However effective distribution and utilization by the target group need coordinated effort of government, committeemen of health professionals and honesty of the manufacturers, importers and distributors in importing, manufacturing and distributing appropriate quality of the powder. The age of a person taking care of child determines the nutritional status of under-five children [34]. Children with the care of other children have a strong prediction for under-five under-nutrition which may relate with the absence of optimal feeding practice, reduction in diversity and frequency of diet and there may be also the probability of drinking unsafe water.
Sex has had a special contribution for under-five children under nourishment [35]. Male children were highly vulnerable to malnutrition when compared with female children may be related to frequency of eating, energy expenditure and exposure to health problems Feeding of under-five children with diluted cow milk has a key role for undernourishment [36]. In case of cow milk feeding it is not uncommon to dilute with ample of water and feeding children make their stomach full without considering it nutrition status. Household structure determines the extent and severity of undernourishment [37]. Children grow in female-headed households were more like to be malnourished because multiple responsibilities of mothers that reduces household income having direct relationship with child health and malnutrition.
Conclusion
Nutrition is many things. It has a bilateral relationship with health, economic development, social developments, and political system of the country. Under-five malnutrition is a phenomenon interwoven with community’s cultural, social, economic and political situation. Unlike adults, nutritional status of Under-five children was greatly influenced by maternal health and nutrition at adolescence, pre-pregnancy, pregnancy and breastfeeding period. Under-five children malnutrition has had the variety of causes or contributing factors where a single fit for all solution could not alleviate the problem rather it requires evidence-based multi-sectorial, multi-level and multistakeholder responsibility and committed politician’s good leadership promoting, facilitating and undertaking of nutritionsensitive and nutrition specific programs.
Limitation of the Systematic Review and Meta-Analysis
Articles on overweight and obesity were studies published in the year 2014 and 2015; may be difficult to representatives of the ten years.
Strength of the Systematic Review and Meta-Analysis
Since the systematic review considers large population from ten articles: able to suggest the contributors for under-five children in addition to the shortage of food shortage.
Ethical Approval and Consent to Publication
All article included in this systematic review and Metaanalysis were ethically approved and consent to publication was secured from University of Gondar institute of public health.
Competing Interests
No competing interests.
Funding
No funding source for this systematic review.
Author’s Contribution
All authors have equally contributed to the systematic review and Meta-analysis.
Acknowledgement
The authors are grateful to Institute of Public Health for encouraging this Systematic Review and Meta-Analysis.
References
- McLachlan M (2015) Delivering on the commitment to eradicate malnutrition in all its forms: The role of the UN System, U.i.a.w.o. Nutr, Editor, United Nations.
- Armstrong S, Curtis M, Kent R, Maxwell D, Mousseau F, Pearce F, Sadler K, Tamminga P, Tansey G (2011) World disasters report 2011: Focus on hunger and malnutrition. Lyons: Imprimerie Chirat.
- Webb P (2014) Nutrition and the post-2015 sustainable development goals, T.U.i.B. Friedman School of Nutrition Science and Policy, Editor, United Nations System, Standing Committee on Nutrition USA.
- Sharkey JR, Cassandra WRD, Johnson M (2011) Association of household and community characteristics with adult and child food insecurity among Mexican-origin households in colonias along the Texas-Mexico border. Int J Equity Health 10.
- Bhawra J, Rhona Hanning MJC, Wilk P, Gonneville SLH (2015) Community perspectives on food insecurity and obesity: Focus groups with caregivers of metis and off-reserve first nations children. Int J Equity Health 14.
- Mendoza EKNS (2015) Migrant and seasonal farmworker food insecurity: Prevalence, impact, risk factors, and coping strategies. Soc Work Pub Health 30:397-409.
- Battersby J (2011) The state of urban food insecurity in Cape Town. Urban Food Security Series 11.
- Oppitz IN, Nelson JAC, Neumann A (2014) Overweight among children under five years of age in municipalities of the semiarid region. Rev Bras Epidemiol 17: 860-872.
- Moreira MA, Haroldo PCC, Ferreira S, Lira PIC (2014) Prevalence and factors associated with overweight and obesity in children under five in Alagoas, northeast of Brazil: A population-based study. Nutr Hospitalaria 29:1320-1326.
- Murage EWK, Samuel SKM, Oti O, Mutua MK, Vijver S, et al. (2015) Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. PLoS ONE 10.
- Muniz PT, Thiago TGC, Araújo S, Nunes NB, Nunes MdS, et al. (2007) Child health and nutrition in the Western Brazilian Amazon: Population-based surveys in two counties in Acre state. Child Health Nutr 23: 1283-1293.
- Custodio E, MÁD, Villamor E, Molina L, Sánchez I, Lwanga M, et al. (2009) Nutritional and socio-economic factors associated with plasmodium falciparum infection in children from equatorial guinea: Results from a nationally representative survey. Malaria J 8.
- Ubesie AC, Ndiokwelu NSC, Uzoka CM, Nwafor CA (2012) Under-five protein energy malnutrition admitted at the university of nigeria teaching hospital, Enugu: A 10 year retrospective review. Nutr J 11.
- Torres AM, KEP, De-Souza AC, John Orav E, Hughes M, et al. (2000) Association of diarrhoea and upper respiratory infections with weight and height gains in Bangladeshi children aged 5 to 11 years. Bull World Health Organ 78:1316–1323.
- Ferdous F, Shahnawaz Ahmed SKD, Farzana FD, Latham JR, Chisti MJ, et al. (2013) Severity of diarrhea and malnutrition among under five-year-old children in rural Bangladesh. Am J Trop Med Hyg 89: 223–228.
- Islam MM, Md Tariquzaman MA, Kabir MA, Pervin R, Begum M, et al. (2013) Predictors of the number of under-five malnourished children in Bangladesh: Application of the generalized poisson regression model. BMC Pub Health 13.
- Mumtaz S, Tabinda Ashfaq HS (2009) Frequency and risk factors for intestinal parasitic infection in children under five years age at a tertiary care hospital in Karachi. J Pak Med Assoc 59: 215-219.
- Maketa V, Raquel Inocêncio da Luz HMM, Zanga J, Lubiba J, Kalonji A, et al. (2015) The relationship between plasmodium infection, anaemia and nutritional status in asymptomatic children aged under five years living in stable transmission zones in Kinshasa, Democratic Republic of Congo. Malar J 14.
- Abebaw TZD (2013) Determinants of child malnutrition: Empirical evidence from Kombolcha district of eastern hararghe zone, Ethiopia. Quart J Int Agric 52: 357-372.
- Astrup A (2015) The role of higher protein diets in weight control and obesity-related comorbidities. Int J Obes 39:721–726.
- Blaney S, Sukotjo S (2015) Feeding practices among indonesian children above six months of age: A literature review on their magnitude and quality. Asian Pac J Clinic Nutr 24:16-27.
- Cesare MD, Soofi SB, Fortunato L, Ezzati M, Bhutta ZA (2015) Geographical and socioeconomic inequalities in women and children’s nutritional status in Pakistan in 2011: An analysis of data from a nationally representative survey. Lancet 3: 229–39.
- Jing Zhang, JSP John H Himes, Yukai Du, Senbei Yang, Shuhua Shi, et al. (2011) Under-nutrition status of children under 5 years in Chinese rural areas-data from the national rural children growth standard survey, 2006. Asian Pac J Clinic Nutr 20: 584-592.
- Rina Tiwari, LMAaKEA (2014) Determinants of stunting and severe stunting among under-fives: Evidence from the 2011 Nepal demographic and health survey. BMC Pediatr 14.
- Justice Moses K Aheto, TJK Benjamin M Taylor, Peter J Diggle (2015) Childhood malnutrition and its determinants among under-five children in Ghana. Paediatr Perinat Epidemiol 29: 552–561.
- Candyce Hamel, JE Khalid Omer, Ndem Ayara, Yahaya Yarima, Anne Cockcroft, et al. (2015) Childhood malnutrition is associated with maternal care during pregnancy and childbirth: A cross-sectional study in Bauchi and cross river states, Nigeria. J Pub Health Res 4: 58-64.
- Chau Darapheak, TT Masashi Kizuki, Keiko Nakamura, Kaoruko Seino (2013) Consumption of animal source foods and dietary diversity reduce stunting in children in Cambodia. Int Arch Med 6.
- Yong Xue, AZ Li Cai, Baoru Yang, Ignatius MY Szeto, Defu Ma, et al. (2015) Growth and development in Chinese pre-schoolers with picky eating behaviour: A cross-sectional study. PLoS ONE 10.
- Nelia P Steyn, AdV Nomonde Gwebushe, Catherine E Draper, Jillian Hill, Marina de Waal, et al. (2015) Did health kick? A randomised controlled trial primary school nutrition intervention improve dietary quality of children in low-income settings in South Africa. BMC Pub Health 15.
- Sujin Song, WOSP (2014) National nutrition surveys in Asian countries: Surveillance and monitoring efforts to improve global health. Asian Pac J Clinic Nutr 23: 514-523.
- Marie T Ruel HA, The Maternal and Child Nutrition Study Group (2013) Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? Lancet 382: 536–51.
- Rehana A Salam, CM, Jai K Das, Zulfiqar A Bhutta (2013) Effectiveness of micronutrient powders (MNP) in women and children. BMC Pub Health 13.
- Teresa Janevic, OP Ivana Bjelic, Amber Kubera (2010) Risk factors for childhood malnutrition in Roma settlements in Serbia. BMC Pub Health 10.
- Pushpa Lata Tigga, JS Nitish Mondal (2015) Association of some socio-economic and socio-demographic variables with wasting among pre-school children of North Bengal, India. Ethiop J Health Sci 25: 64-72.
- Basit A NS, Chakraborthy KB, Darshan BB, Kamath A (2012) Risk factors for under-nutrition among children aged one to five years in udupi taluk of Karnataka, India: A Case Control Study. Australas Med J 5: 163-167.
- Rabia Fentaw, ABaDA (2013) Prevalence of child malnutrition in agro-pastoral households in afar regional state of Ethiopia. Nutr Res Prac 7: 122-131.