Research Article - (2023) Volume 8, Issue 1
Prevalence and Parental Perspectives of Obesity in Children with Autism Spectrum Disorder (ASD)
William Tasker*
Department of Pediatrics and Geriatrics, Berlin Medical Academy, UK
*Correspondence:
William Tasker,
Department of Pediatrics and Geriatrics, Berlin Medical Academy,
UK,
Tel: 07902992285,
Email:
Received: 02-Jan-2023, Manuscript No. IPJCO-21-11548;
Editor assigned: 04-Jan-2023, Pre QC No. IPJCO-21-11548 (PQ);
Reviewed: 18-Jan-2023, QC No. IPJCO-21-11548;
Revised: 23-Jan-2023, Manuscript No. IPJCO-21-11548 (R);
Published:
30-Jan-2023, DOI: 10.36648/2572-5394.23.8.002
Abstract
Objective: To identify the prevalence of obesity among children with ASD and possible exacerbating factors.
Design: Mixed methods; literature review, a retrospective cross-sectional measure of obesity prevalence and a telephone questionnaire.
Setting: Children’s outpatient clinic, University Hospital of North Tees.
Patients: Children referred for ASD assessment (less than 5 years at referral).
Measures: BMI centile (UK-90 data), overweight ≥ 85th centile, obese ≥ 95th centile.
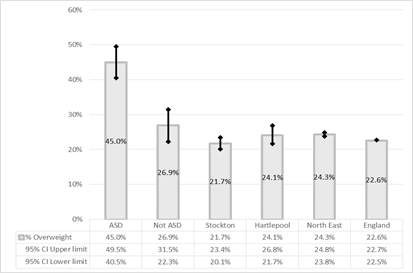
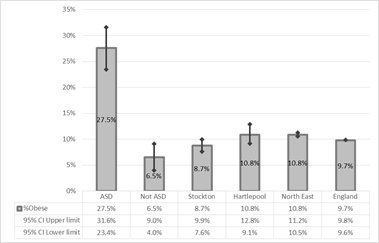
Results: 221 children referred for ASD assessment had recorded heights and weights. 45.0% (95% CI 40.5%-49.5%) with later diagnosed autism were overweight and 27.5% obese (95% CI 23.4%-31.6%). Significantly higher than; children referred but not meeting the criteria for autism, (26.9% (95% CI 22.3%-31.5%) overweight and 6.5% (95% CI 4.0%-9.0%) obese) and the local prevalence at school entry (24.1% (95% CI 21.7%-26.8%) overweight, 8.7% obese (95% CI 7.6-9.9%)).
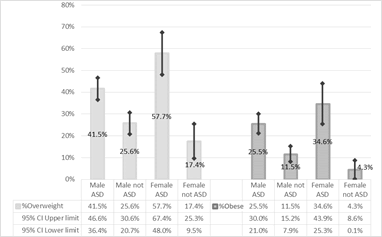
The prevalence of being overweight among females with ASD was significantly higher than males (57.7% (95% CI 48.0-67.4%) v 41.5% (95% CI 36.4-46.6%)).
A survey for parents of children with a BMI centile of ≥ 95% revealed that a significant proportion (48%) of parents were “not worried” about their child’s weight. Themes included a restrictive eating pattern, a lack of appropriate physical activity options and a lack of acknowledgement of weight by professionals.
Conclusions: The prevalence of being overweight or obese was significantly higher among children with ASD than those without ASD and the local population. Possible exacerbating factors that could be considered in further research include sex, parental and professional awareness, diet and barriers to physical activity.
Keywords
Patients; Overweight; Population; Height; Weight
Introduction
Children in North East England have the highest rate of obesity for
any region in England [1]. Autism is a common condition, estimated
to affect 1 in 100 children [2,3]. It had been noted anecdotally,
among community paediatricians, that many children presenting to clinic with suspected autism were obese, with little specific service
provision for affected children.
A literature review was undertaken to examine the existing literature
on obesity prevalence among children with autism. A Literature
search was carried out via healthcare databases advanced search using the databases: MEDLINE, HDAS, CINAHL, BNI, EMBASE
and PUBMED (Table 1).
Table 1: Literature search summary.
| Initial search terms |
Relevant expanded terms with thesaurus |
| 1. Autism |
Autism Spectrum Disorder OR Autism Disorder |
| 2. Obesity |
Overnutrition OR Overweight OR Obesity, Abdominal OR Obesity, Morbid, OR Obesity, metabolically benign OR Paediatric Obesity. |
| 3. Adolescent OR Child OR P(a)ediatric |
Adolescent OR Minors OR Child OR P(a)ediatric |
| 4. Prevalence OR Risk Factor |
Causality OR Risk |
Titles and abstracts were reviewed. Papers were included if the
aim was to investigate the prevalence of obesity in children with
autism. They were excluded if they were, for example, exploring
the relationship of autism to maternal obesity or looking at obesity
prevalence within populations with a more broad diagnosis of
Intellectual disability or other conditions e.g., Down Syndrome or
Prader Willi. Studies looking at populations with an age >18 years
were also excluded.
Studies found; Medline 23, BNI 8, CINAHL 35, EMBASE 29,
Pubmed 158.
After Exclusions; Medline 12, BNI None relevant, CINAHL 6, EMBASE
3, Pubmed 8.
6 were excluded as duplicates. Four excluded as full text not available,
of these three were from USA, one from Australia. References
were searched for other relevant studies. Two published
audits were identified; One from England looking at 77 patients
[4], another from Wales looking at 39 patients [5]. Neither compared
their results to a reference population, and in the published
audit reports the definition of obesity and the data set used was
not specified.
Therefore, 19 relevant and unique studies were identified. One
was a meta-analysis, the others compromised of case-control
and cross-sectional studies. 11 showed a significantly increased
prevalence of children with autism being overweight or obese
compared to a control group, four found no significant difference
and five studies did not compare to a reference population. Three
were based in China; two in Malaysia and one in Ireland, the rest
were from the USA. They all used Centres for Disease Control
(CDC) data, except one using World Health Organisation (WHO)
data (Chinese study).
10 studies studied ages across the paediatric population from
preschool through to adolescence, 3 mainly compromised of preschool
children less than 9 years and 6 studied adolescents above
the age of 10.
The literature review suggested that obesity was likely to be an issue
among children with autism, but that there was a lack of data
from the UK. Within the department it was agreed that the issue
should be investigated by calculating the prevalence of obesity in children referred for an autism assessment over the last year and
then comparing to the local average as published by Public Health
England (PHE). It felt prudent to investigate using the UK-90 data
as it allowed comparison to PHE data. In order to seek parental
perspective and form the basis of considerations for service provision,
it was agreed that qualitative data from parents and carers
of autistic children with obesity should be collected. The survey
was carried out during the coronavirus pandemic, which affected
clinic attendance; therefore questionnaires were carried out via telephone. Data collection was carried out after Trust Caldicott
approval was sought and confirmed. It was agreed by management
that as this project was a local service evaluation, ethical
approval was not required.
Methods
Hospital numbers for children referred to the clinic for suspected
autism were collected over a 1-year period from March 2018 to
March 2019.
From scanned notes, paper notes, as well as clinic letters the following
was recorded;
• Date of birth
• Sex
• Postcode
• Age at time of height/weight measurement closest
weight to 5th birthday. If the closest weight was under the age of
4 a weight at an older age was chosen if available, if not, then a
weight taken under the age of 4 was used.
• Height and weight
• Whether, after the Multiagency autism Team assessment,
a diagnosis of autism was confirmed or the criteria were
not met and a diagnosis not made.
Once data was collected the BMI and BMI centile was calculated
using the RCPCH growth chart app, using UK-90 data.
Results and Discussion
Children were then identified if they were overweight (>85th centile) or obese (>95% centile). This being the public health definition of being overweight or obese rather than the clinical definition which uses >91st centile as overweight and >98th centile as obese. Using public health definitions meant that data collected was able to be directly compared to PHE data.
The proportion of overweight and obese children was calculated according to whether they had confirmed autism. The prevalence of obesity in this cohort was compared to data for children aged 4 to 5 years (reception age) from PHE, both locally and nationally.
Children with Obesity were identified. A questionnaire designed collaboratively within the department was then undertaken by telephoning their parents. It explored parental perspective on weight, diet and physical activity followed by current support and what could be done differently to manage weight.
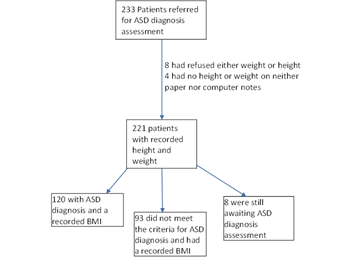
A BMI centile was calculated for 221 out of the 233 patients referred in a year and 120 of these had ASD confirmed (Figure 1).
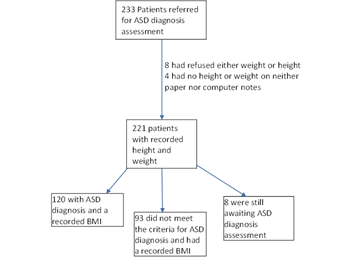
Figure 1: Number of children with height and weight recorded, outcome of ASD diagnostic pathway.
The mean age when measured was 4.44 ± 1.07 (1 standard deviation) with a range of 2.00 to 6.99 years.
Both males and females that had confirmed autism were statistically more likely to be overweight and obese than children who did not meet the diagnostic criteria. Obesity and overweight prevalence rates among children with confirmed autism were also significantly higher than local, regional and national averages (Figures 2 and 3).
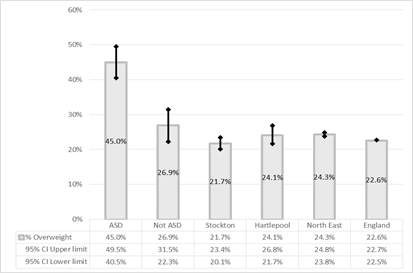
Figure 2: Prevalence of being overweight (BMI ≥ 85th centile). Comparing those with confirmed ASD, those referred but not meeting the diagnostic criteria, as well as local, regional and national data.
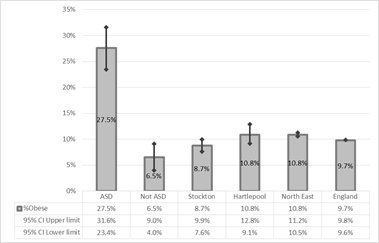
Figure 3: Prevalence of obesity (BMI ≥ 95th centile). Comparing those with confirmed ASD, those referred but not meeting the diagnostic criteria, as well as local, regional and national rates.
The difference among females was more marked, with autistic females being significantly more likely to be overweight than autistic males (Figure 4). Although the average prevalence of obesity was higher among females 34.6 (95% CI 25.3-43.9%) vs 25.5 (95% CI 21.0-30.0) this was not significantly different [6-9].
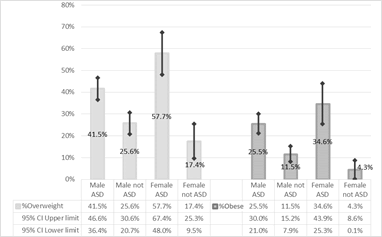
Figure 4: Prevalence of being overweight or obese, by sex. Comparing those with confirmed ASD and those not meeting the diagnostic criteria.
Questionnaire
33 Children with ASD were identified as Obese according to Public Health definition of a BMI >95th centile when plotted on using UK-90 data. Each child’s parents were telephoned twice in an attempt to complete the questionnaire. 21 questionnaires via telephone completed by one member of the paediatric team. For 13 there was no answer, giving at 62% response rate. All parents that were contacted agreed to complete the questionnaire. Questions were delivered as written and if there was no answer, repeated to prompt further consideration. Some definitions were given further clarification for example very active meaning at least 30 minutes of exercise daily making them breathless and very inactive being rarely does any activity making them breathless.
1. Parental concern about weight: Despite all the children plotting >95th centile for BMI 48% of parents indicated that they were “not worried” about their weight.
“Age when weight became an issue”
9 Patients stated that weight had not become an issue at any age. In children where parents felt weight had been an issue (12), ages ranged from 2 to 6 years with 5 parents identifying that issues started aged 3.
2. Parental perspective on diet: Most parents identified their child’s diet as very unhealthy or unhealthy (71%), with only one diet being identified as very healthy.
“What things make a healthy diet difficult?”
From the 20 completed questionnaires the themes that emerged from exploration of the factors that make health eating difficult included
• Sensory issues: The most common issue identified was with food texture, for example not liking runny foods. Other sensory issues with healthy foods identified included taste, for example only eating bland foods, appearance for example, preferring beige or red colour and smell
• Refusing healthy foods: Parents described the children disliking vegetables, fruit, meat and home cooked foods
• Behaviour: Regarding foods, issues with tantrums, mood, eating quickly and large volumes were described.
“What things could be done to encourage them to eat healthier?”
9 Parents/carers had no ideas or thoughts on the matter, however there were some thoughts from other parents/carers.
One theme was ingredient adjustments in diet, including hiding healthy foods (4 parents), and making direct swaps of foods to healthier ones (2 parents). Ideas of parental input on behaviour included persisting with healthy foods (3 parents) and using reward/ sticker charts (1 parent). Ideas for parental input on sensory issues included touching and handling healthy foods (2 parents) and arranging foods in sections on a plate (1 parent). Only two parents addressed amount of calories, one highlighting smaller portions as an option, another need for nursery to control the amounts eaten. Two parents/carers identified the possibility of education helping to identify healthy or unhealthy foods and one felt that supplements would help.
3. Parental perspective on physical activity:
“What things make keeping physically active difficult?”
From the 20 completed questionnaires nine parents/carers felt there were no difficulties with their child being physically active with 10 describing their child as “very active”. Among the other parents/carers themes included
• Their child enjoying being sedentary in their activities: For example liking video games (2 parents)
• Difficulty with the social aspect of physical activity: 3 said there was difficulty with group/team sports and that they do not understand games with other children (2 parents) or do not like losing (1 parent)
• Motor issues-Balance/spatial awareness (2 parents)
• Dislike of being active (2 parents) being outside (2 parents), noises associated with being outside (1 parent)
• Irregular sleep (1 parent)
• Supervision issues-one parent/carer stated they have to be cautious of surroundings.
“Is there anything that could be done to encourage them to be more physically active?”
11 Parents/carers felt there was nothing required, with one stating that they had already exhausted the options, however there were some thoughts from remaining 8 parents/carers.
One parent suggested that school support physical activity for children with ASD, with 2 other parents stating that activities or sports should be tailored to their needs, for example less emphasis on team sports and more water activities. Other thoughts included physiotherapy support (1 parent), signposting for opportunities or support locally across sectors (1 parent) and promoting active travel to school (1 parent).
4. Weight loss support: 20 of 21 identified no form of previous weight loss support. Two stated that the only time it had been raised as an issue was when being weighed at school. One had dietician input but stated that the emphasis was more on nutrition and vitamins.
“Is there anything we, as doctors, can do differently to make it easier for children with ASD to achieve a healthy weight?”
5 could not identify anything medical professionals could do, one stating that it was unlikely to help. Four parents were hoping for guidance/signposting to activities tailored to children with ASD. Some parents focussed on nutrition with one highlighting need for nutritional support, one looking for a plan to challenge the restricted diet, three parents looking to address food sensory issues. Suggestions to address this included leaflets (1 parent), and signposting for ideas (2 parents) e.g., Change for life ideas, which may need tailoring to children with ASD (1 parent).
Supplementary vitamins were suggested by 11 parents. Two parents felt that doctors should directly address issues such as weight and restrictive eating and another felt that only issues with being underweight were addressed.
Some parents focussed on dietician support and there was some frustration with the experience they had.
Three parents said that referrals were not picked up or accepted when younger; one felt the dietician referral process was too complicated and long. Three parents highlighted the need for broader support and education at the time of diagnosis. One felt that some positive steps at home were being undone by unhealthy eating at school.
Conclusion
The proportion of children who are overweight or obese was significantly
higher in children referred to clinic with suspected ASD
than the local population and the children with ASD confirmed
later were significantly more likely to be overweight or obese
than children who did not meet the diagnostic criteria. The difference
in incidence seemed more marked among females although
the number of females referred was lower (n=43).
The questionnaire results suggested that parent’s perspective was
generally that they weren’t concerned about their child’s weight.
Two parents mentioned that the only time the child’s weight had
been mentioned as an issue was at school after routine weights
and heights were measured. It is likely that the issue is only raised
in clinic for children severely obese. Regarding issues of diet, parents
mainly identified restrictive eating. Regarding physical activity
the issues mainly revolved around barriers for people with
social and communication difficulties.
It is clear that in the local area that in order to address childhood
obesity, an increased focus needs to be made on children with autism.
The questionnaire established a range of viewpoints which
included early intervention, support and awareness but it is important
to note that this may not be acceptable to all parents and more routine discussion around weight and giving diagnoses of
obesity more regularly would need further evaluation.
The strengths of this evaluation included the fact that the data
available allowed direct comparison to local populations, the
number of children was adequate locally as it represented all the
children referred and diagnosed in a whole year and also there
was an attempt to obtain a parent perspective, even during the
pandemic, by doing a telephone questionnaire.
Limitations included exact age matching between children referred
for ASD assessment and local PHE data. Routine height
and weight is measured in reception year so children’s ages range
from 4 to 5 years. In the group of children referred the range was
from 2 to 7 years with a mean of 4.44. The children were therefore
more likely to be younger than the local population data.
Given that obesity prevalence increases with age, this is likely to
have, if anything, underestimated the eventual prevalence among
the referred group.
The results are not directly generalizable to a wider population
but have established clear justification for further research both
in establishing the extent of obesity among children with ASD and
also informing public health measures and clinical interventions
to help this population who are already enormously disadvantaged
by their condition, and who shouldn’t suffer inadvertent
further discrimination through the provision of services that are
wholly inappropriate to their needs.
Acknowledgement
None.
Conflict Of Interest
None.
References
- Taylor B, Jick H, MacLaughlin D (2013) Prevalence and incidence rates of autism in the UK: Time trend from 2004-2010 in children aged 8 years. BMJ Open 3: 3219.
[Google Scholar]
- Loomes R, Hull L, Mandy W (2021) What is the male-to-female ratio in autism spectrum disorder?A systematic review and meta-analysis. J Child Adol Psyc 56: 466-474.
[Crossref] [Google Scholar]
- Grylls E, Coxhead M, Dehiwelage P, Thomas S (2013) G109 obesity in children with Autism Spectrum Disorder audit. Arch Disin Child 98: 52-52.
[Google Scholar]
- Nasef H, Nasef H (2017) Prevalence of obesity in children with autism-a west wales study-eap 2017 congress and mastercourse. Eur Aca of paed.
[Google Scholar]
- He XZ, Baker DW (2004) Body mass index, physical activity, and the risk of decline in overall health and physical functioning in late middle age. Am J Public Health 94: 1567-1573.
[Crossref] [Google Scholar]
- Xiong N, Ji C, Li Y, He Z, Bo H (2009) The physical status of children with autism in China. Res Dev Disabil 30: 70-76.
[Crossref] [Google Scholar]
- Raiten DJ, Massaro T (1986) Perspectives on the nutritional ecology of autistic children. J Autism Dev Disord 16: 133-143.
[Crossref] [Google Scholar]
- Baird G, Simonoff E, Pickles A (2006) Prevalence of disorders of the autism spectrum in a population cohort of children in south thames: The special needs and autism project (SNAP). Lancet 368: 210-215.
[Crossref] [Google Scholar]
- Provost B, Lopez BR, Heimerl S (2007) A comparison of motor delays in young children: Autism spectrum disorder, developmental delay, and developmental concerns. J Autism Dev Disord 37: 321-328.
[Crossref] [Google Scholar]
Citation: Tasker W (2023) Prevalence and Parental Perspectives of Obesity in Children with Autism Spectrum Disorder (ASD). J
Child Obesity. 8:002.
Copyright: © 2023 Tasker W. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.