Keywords
Pregnancy induced hypertension; Antenatal care service; Diabetes;
Women
Introduction
Pregnancy-Induced Hypertension (PIH) is defined as a systolic
blood pressure of less than 140 millimetres of mercury and a
diastolic blood pressure of less than 90 millimetres of mercury, or both. PIH is a form of hypertension that develops after 20
weeks of pregnancy in women who previously had normal blood
pressure. Along with infection and postpartum haemorrhage,
it has long been one of the most serious issues for mothers during pregnancy. Gestational hypertension, preeclampsia, and
Eclampsia are the three broad categories of PIH [1,2].
Gestational hypertension is diagnosed in women whose blood
pressures rise to 140/90 mm Hg or higher for the first time
after 20 weeks of pregnancy, but who do not have proteinuria.
Preeclampsia is characterized as blood pressure of 140/90 mmHg
with or without Proteinuria (300 mg/24 hours) that appears after
20 weeks of pregnancy but resolves up to 12 weeks after delivery
and Eclampsia is defined as a convulsion that cannot be attributed
to another cause in a woman with preeclampsia. Seizures are
generalized and can occur prior to, during, or after labour. The
percentage of women who do not have seizures until 48 hours
after giving birth is about 10%. Any chronic hypertensive disease,
regardless of the cause, puts a woman at risk for developing
superimposed preeclampsia syndrome [1,3].
In 2013, approximately 289,000 people died worldwide as a
result of pregnancy-related causes, with 99% of deaths occurring
in developing countries. Sub-Saharan African countries account
for about 56% of all maternal deaths worldwide. In developing
countries, a woman's lifetime risk of dying from pregnancyrelated
complications is 14 times higher than in developed
countries [4,5].
According to a population-based study in South Africa,
hypertensive disorders of pregnancy affect 12% of pregnant
women, and they are the leading cause of maternal death,
accounting for 20.7% of all maternal deaths [3]. Ten percent of
all births are complicated by pregnancy-induced hypertension.
Every year, approximately 40,000 people, mostly from developing
countries, die as a result of PIH. Preeclampsia is thought to be
responsible for 40-60% of maternal deaths in developed countries
[2,3].
Many of these health issues are widespread in developing
countries such as Ethiopia. As a result, our country's maternal
mortality rate is 676 per 100,000 live births, compared to 12 per
100,000 live births in most developed countries [4,5].
According to a United Nations (UN) report, Ethiopia is one of
the five countries that together account for 50% of the world's
maternal death and rural areas mostly contribute to maternal
death [4]. A study conducted in Addis Ababa indicated that the
prevalence of Hypertensive Disorders of Pregnancy (HDP) among
diagnosed pregnant were 5.5% of which the majorities were due
to preeclampsia [6].
The cause for hypertension is unknown, there does appear to be
certain Risk factors postulated to influence the risk of Pregnancyinduced
hypertension Null parity, multiple pregnancies, history of
chronic hypertension, gestational diabetes, fetal malformation,
obesity, extreme maternal age less than 20 or over 40 years,
history of PIH in previous pregnancies and chronic diseases like
renal disease, diabetes mellitus, cardiac disease, unrecognized
chronic hypertension, positive family history of PIH which shows
genetic susceptibility, psychological stress, alcohol use, rheumatic
arthritis, extreme underweight and overweight, asthma and low
level of socio-economic status are the risk factors for PIH [7,8].
PIH is a major pregnancy complication associated with premature delivery, Intra-Uterine Growth Retardation (IUGR), abruptio
placentae, and intrauterine death, as well as maternal mortality
and morbidity [9,10].
Ante-Natal Care (ANC) is one of the maternal services in Ethiopia.
Blood pressure measurement, urine tests for Proteinuria and UTI,
HBsAg, VDRL, blood group and RH, PICT, and CBC are among the
component of routine ANC. According to 2019, EMDHS results
show that 74% of women who gave birth in the 5 years preceding
the survey received antenatal care from a skilled provider at least
once for their last pregnancy [11].
Hypertension caused by pregnancy is the leading cause of
maternal and perinatal morbidity and mortality. However, while
a few studies are looking into the prevalence and associated
factors of PIH in Ethiopia, none have been done in our study
field. As a result, the aim of this study is to find out how common
pregnancy-induced hypertension is and what factors contribute
to it.
Materials and Methods
Study period and setting
The study was conducted in Wachemo University Nigist Eleni
Mohammed Memorial comprehensive and specialized hospital.
The hospital is found in Hossaena town, Hadiya Zone, Southern
Ethiopia, at 7°c 3’ 19”-7°c 56’13” east longitudinal line. The town
is located 232 km south of Addis Ababa. The hospital provides
preventive, curative, and rehabilitative clinical services organized
in four case teams an outpatient, inpatient, emergency, and
critical care, maternal, child health and obstetrics and operation
theatre, with a capacity of accommodating 250 beds and 499
health professional and 382 supportive stuff. The study was
conducted from December 30, 2020, to February 2021 [12-14].
Study design and period
A hospital-based cross-sectional study design was conducted
at Wachemo University Nigist Eleni Mohammed Memorial
comprehensive and specialized Hospital.
Source population
All pregnant women who had ANC follow up in Wachemo
University Nigist Eleni Mohammed Memorial comprehensive and
specialized Hospital.
Study population
Selected pregnant women who had ANC follow-up and who fulfil
the inclusion criteria.
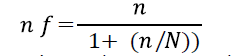
Sample size determination
The sample size was calculated using the single population
proportion formula, considering the following assumptions and
taking the prevalence of the proportion of PIH 45.5% which was
a study conducted in Jimma University Specialized Hospital, West
Ethiopia [15].

Where n=the desired sample size P=prevalence of PIH=45.5%
(which was taken from a study conducted at Jimma University
Specialized Hospital, west Ethiopia, 2011) Z1-α/2=Critical
value at 95% confidence level (1.96) d=the margin of error=5%
n=(1.96)2.0.455(1-0.455)/(0.05)2=381. Since our source
population (N), is below 10,000, we used correction formula.
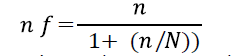
Where N is source population, nf was the final sample size,

Therefore, by taking a non-response rate of 10%, the final sample
size was 333.
Sampling procedure
A systematic random sampling technique was used to select the
study participants from the chart review. The sampling interval
(k) was determined by dividing the total number of pregnant
recorded data who seek ANC at the previous half of a year with
gestational age>20 weeks June 2019 to May 2020, which was
1472 by the calculated sample size 333. The first pregnant woman
data was selected by lottery method among the ANC service user
within the study period and the rest was selected by the interval
3 (Figure 1).
Figure 1: Schematic presentation of sampling procedure
pregnancy-induced hypertension among mothers
attending antenatal care in Nigist Eleni Mohammed
Memorial comprehensive and specialized, Hadiya zone,
southern nation nationality people region (n=333).
Study variables
Dependent variables: Prevalence of pregnancy-induced
hypertension (1: yes, 0: no).
Independent variables: Sociodemographic-related characteristics
of respondents like age, marital status, educational status, and
occupational status.
Obstetrics history-related characteristics of respondents like
gravidity, parity, the multiplicity of pregnancy, prior PIH, prior
gestational DM.
General medical history related characteristics of respondents like
DM, HTN, kidney disease, cardiac illness, and substance abuse.
Current pregnancy-related characteristics of respondents like
weight, lab results, signs, and symptoms.
Data collection procedures
Data was collected using a structured questionnaire for recorded
review developed for this study. Since the registration was
prepared in the English language, the checklist was also prepared
in English. So, data were collected by group members, and data
collection was done in the hospital. Data collectors were agreed
on how to collect data and discussed the tool in detail before
actual data collection.
All relevant information regarding demographic data, clinical
findings, and laboratory results were collected. Data about
antenatal care were extracted from the attendance history file
and antenatal card.
Inclusion and exclusion criteria
All pregnant women attending antenatal care service with
complete recorded data with gestational age is ≥ 20 weeks were
included and data not fully recorded were excluded.
Operational definition
Pregnancy-Induced Hypertension (PIH): A pregnant woman
attending delivery service with high blood pressure (140/90
mmHg) after 28 weeks of gestation was measured two times
six hours apart by trained data collectors and with or without
proteinuria. The diagnosis of PIH was confirmed by a physician
working in the labor ward. Pregnancy-induced hypertension
includes gestational hypertension, pre-eclampsia and eclampsia
[15].
Proteinuria: The presence of an excess of serum proteins in the
urine which is diagnosed by dipstick ≥ +1 [5].
Data quality assurance
To ensure the consistency of the data, the nature of the data
collection tool was emphasized for its simplicity and uniform
group rating scales, validity and reliability were taken into account
and data collectors were educated. To check the accuracy, the
questionnaire was prepared in English and then translated into
the local Hadiya language and back-translated into English.
To check the accuracy, the questionnaire was pre-tested on 17
mothers in Worabe Hospitals outside the study area, and the
interview was carried out in private. Throughout the collection of
data, interviewers were tracked at each location, daily meetings
were held between the data collectors, the supervisor, and the
principal investigator in which concerns resulting from interviews
performed and errors discovered during editing were addressed
and decisions were made. Until data entry, the collected data
were inspected and tested for completeness; incomplete data
was discarded. The prototype for the data entry format was
developed and programmed.
Data processing and analysis
Data were tested, coded, and entered in EPI Data version 3.1 and exported for analysis to Statistical Package for Social Sciences
(SPSS) version 20. The key investigator was responsible for data
entry. The variable description was performed and presented in
frequency, using tables, graphs, charts, and chi-square statistics
(χ2). Adjusted Odds Ratios (AOR) and a 95% confidence interval
using logistic regression were used to verify the existence and
intensity of the correlation between independent and dependent
variables. In the bivariate analysis, variables having P-values
less than 0.25 were entered into the multivariate analysis using
backward elimination. The fitness of the model was tested using
the 0.796 Hosmer and Lemeshow test. Based on their relationship
of importance (i.e., p<0.05), the final result was interpreted.
Results
Characteristics of respondents
A total of 333 pregnant women charts were incorporated into the
study. This made the response rate 100%.
Out of 333 women included in the study, above half the 184
(55.3%) respondents were urban residents. The majority,
199(59.8%), was 25-35 years old (Table 1).
| Variables |
Categories |
N (%) |
| Age in years |
18-24 |
74(22.2) |
| 25-35 |
199(59.8) |
| >35 |
60(18.0) |
| Address of women |
Urban |
184(55.3) |
| Rural |
148(44.7) |
Table 1: Selected socio-demographic characteristics of the study participants on pregnancy-induced hypertension among mothers attending antenatal care in Nigist Eleni Mohammed Memorial comprehensive and specialized, Hadiya zone, southern Ethiopia (n=333).
Basic obstetric and clinical characteristics were assessed in this
study. Out of 333, pregnant women who were participated in this
study almost half 168(50, 5%) of pregnancy were primigravida,
regarding parity of the women, 166(49.85%), 142(42.64%), and
25(7.5%) were nulliparous, multipara and grand multiparous
respectively (Figure 2). The majority, 236(70.9%) of mothers
were gestational ages between 20 to 37 weeks, majority
329(98.8%) of the pregnant mothers who attended for ANC had
single multiplicity, 31(9.3%) mothers had a history of PIH, only
11(3.3%) of them were having a history of gestational diabetic
Mellitus; while 2(0.6%) of mothers of the pregnancies had a previous stillbirth and majority of respondents 7(2.1%) mothers
were history of previous caesarean section (Table 2).
Figure 2: Parity distribution pregnancy-induced hypertension among mothers attending antenatal care in Nigist Eleni Mohammed Memorial comprehensive and specialized, Hadiya zone, southern Ethiopia (n=333).
| Variables |
Categories |
N (%) |
| Gravidity |
Primigravida |
168(50.5) |
| Multigravida |
165(49.5) |
| Gestational age (in the week) |
20-37 |
236(70.9) |
| >37 |
97(29.1) |
| Multiplicity |
Single |
329(98.8) |
| Multiple |
4(1.2) |
| History of PIH |
Yes |
31(9.3) |
| No |
302(90.7) |
| History of gestational DM |
Yes |
11(3.3) |
| No |
322(96.7) |
| Previous stillbirth |
Yes |
2(0.6) |
| No |
331(99.4) |
| Previous Cesarean surgery |
Yes |
7(2.1) |
| No |
326(97.89) |
Table 2: Obstetric and clinical characteristics of the study participants on pregnancy-induced hypertension among mothers attending antenatal care in Nigist Eleni Mohammed Memorial comprehensive and specialized, Hadiya zone, southern Ethiopia (n=333).
Of the total 333 pregnant women, 10(3%) of mothers have had
a history of DM, and 3(0.9%) of mothers have had a history of
renal disease, 4(1.2%) mothers have had a history of cardiac
disease,2(0.6%) pregnant mothers have had known substance
abuse and 13(3.9%) mothers were had other medical disease like
TB, HIV, Malaria (Table 3).
| Variables |
Categories |
Frequency |
| History of diabetes mellitus |
Yes |
10(3.0) |
| No |
323(97.0) |
| History of renal disease |
Yes |
3(0.9) |
| No |
330(99.09) |
| History of cardiac disease |
Yes |
4(1.2) |
| No |
329(98.8) |
| Known substance abuse |
Yes |
2(0.6) |
| No |
331(99.4) |
| Another medical disease like TB, HIV, Malaria |
Yes |
13(3.9) |
| No |
320(96.1) |
Where: 3 TB, 5 Malaria and 5 HIV cases. |
Table 3: Behavioral and Life characteristics of the study participants on pregnancy-induced hypertension among mothers attending antenatal care in Wachemo University, compressive specialized hospital, Hadiya Zone, Southern Nation Nationality People Region (n=333).
Out of 333 total participants, with headache and blurring of
vision was reported by 6(1.8%), 4(1.2%) of the pregnant women
had epigastric pain, 3=(0.9%) were with history of shortness
of breath, 49(14.7%) mothers with a history of pitting edema,
15(4.5%) mothers were with convulsion or seizure, 71(21.3%)
with history of blood pressure between 140/90=160/110 mmHg,
12(3.6%) with platelet count<100000 which is abnormal, the
result of dipstick urine test, proteinuria ranges from negative
to +++ which was 55(16.5%) and 4(1.2%) mothers were with
history of abnormal liver function (Table 4). Out of the total
of 78(23.42%) pregnant women who had PIH, 22(28.2%) was
gestational hypertension, 28(35.9%) were preeclampsia without severity feature, 13(16.7%) were preeclampsia with severity
features and 15 (19.23%) were Eclampsia respectively (Figure 3).
Figure 3: The prevalence of pregnancy-induced hypertension and associated factors among mothers attending antenatal care in Nigist Eleni Mohammed Memorial comprehensive and specialized, Hadiya zone, southern nation nationality people region (n=333).
| Variables |
Categories |
N (%) |
| Headache and blurring of vision |
Yes |
6(1.8) |
| No |
327(98.2) |
| Epigastric pain |
Yes |
4(1.2) |
| No |
329(98.8) |
| Shortness of breath |
Yes |
3(0.9) |
| No |
330(99.1) |
| Pitting edema |
Yes |
49(14.7) |
| No |
284(85.3) |
| Convulsion or seizure |
Yes |
15(4.5) |
| No |
318(95.5) |
| Blood pressure |
<140/90 mmHg |
255(76.6) |
| 140/90-160/110 mmHg |
71(21.3) |
| >160/110 mmHg |
6(1.8) |
| Platelet count |
Normal |
321(96.4) |
| <100000 |
12(3.6) |
| Proteinuria |
Yes |
55(16.5) |
| No |
278(83.5) |
| Liver function normally |
Yes |
329(98.8) |
| No |
4(1.2) |
| Pregnancy-induced hypertension |
Yes |
78(23.42) |
| No |
255(76.58) |
Table 4: Characteristics related to current pregnancy of women on pregnancy-induced hypertension among mothers attending antenatal care in Nigist Eleni Mohammed Memorial comprehensive and specialized, Hadiya zone, southern nation nationality people region (n=333).
Prevalence of pregnancy-induced hypertension
of women
The overall prevalence of PIH was 23.42% of the respondents with
95% CI (21.8, 30.5) with a mean of 0.29 and standard deviation
of ± 0.44.
Multivariable analysis was used to control potential confounders.
Accordingly, Age 25 to 35 years (AOR=6.189; 95%CI;
2.232,7.164),urban residence (AOR=2.103; 95%CI; 1.046, 4.234),
primigravida (AOR=1.6; 95%CI; 1.642, 2.611),gestational age in
weeks (20 to 37 weeks) (AOR=5.278; 95%CI; 1.852, 6.038), past
history of PIH(AOR=1.358; 95%CI; 1.756, 4.351) and past history
of DM (AOR=7.347; 95%CI; 1.344, 9.372) were found to be
independently associated (Table 5).
| Variable |
Pregnancy-induced hypertension |
OR (95% CI) |
| Yes |
No |
COR (95%) |
AOR (95%) |
| Age in years |
18 to 24 |
16 |
32 |
1.302 (0.605, 0.2801) |
4.728 (1.585 , 9.103)* |
| 25 to 35 |
34 |
180 |
3.447 (1.891, 6.286) |
6.189 (2.232 , 7.164)* |
| >35 |
28 |
43 |
1 |
1 |
| Residency |
Urban |
37 |
154 |
1.690 (1.014, 2.815) |
2.103 (1.046, 4.234)* |
| Rural |
41 |
101 |
1 |
1 |
| Gravidity |
Primigravida |
42 |
84 |
0.421 (0.251, 0.705) |
1.6 (1.642, 2.611)* |
| Multigravida |
36 |
171 |
1 |
1 |
| Gestational age (in week) |
20 to 37 |
58 |
163 |
0.611 (0.396,1.079) |
5.278 (1.852,6.038)* |
| >37 |
20 |
92 |
1 |
1 |
| History of PIH |
Yes |
24 |
7 |
0.064(0.026,0.155) |
1.358 (1.756 ,4.351)* |
| No |
54 |
248 |
1 |
1 |
| History of DM |
Yes |
6 |
4 |
5.229(1.437,19.034) |
7.344 (1.344 – 9.372)* |
| No |
72 |
251 |
1 |
|
Where 1=Reference,*shows the variable significance at p-value = 0.05 in multivariable analysis |
Table 5: The final multivariable binary logistic regression model showing risk factors independently pregnancy-induced hypertension among mothers attending antenatal care in Nigist Eleni Mohammed Memorial comprehensive and specialized, Hadiya zone, southern nation nationality people region (n=333).
Discussion
The overall prevalence of pregnancy-induced hypertension
23.42%, which indicates that a significant number of women
attending ANC services at Wachemo University, Nigist Eleni
Mohammed Memorial comprehensive and specialized hospital.
This might increase the morbidity and mortality of the mother
and the fetus. If appropriate preventive measures are not taken
for the risk of pregnant women, in long term, it might be the first
cause of maternal mortality. The prevalence of PIH in this study is
greater than the study conducted in Jimma University Specialized
Hospital which was 8.48%, Karamara hospital which was 19% and Dessie Referal Hospital which was 8.4% respectively [16,17].
The prevalence of PIH in this study lowers when compared to
the prospective cohort study conducted in Tigray regional state,
Ethiopia which was 66.4% [2].
This difference might be attributed to differences in the study
period and study design. The population might also be different in
lifestyle and culture. However, the prevalence in this study is still
greater than the study done in Ethiopia at Tikur Anbessa Hospital
which was 5.3%, and Mettu Karl Hospital, 2.4% respectively
[18,19].
This discrepancy might be because of differences in the study
period, study design, and health-seeking behaviours of pregnant
women. Besides, the gap might be due to the current health
policy which focuses on the implementation of focused ANC and
exempted service for maternal care which increases the health
care seeking behaviour of pregnant women which increases
detection of the case.
In this study, women having lower age categories 25 to 35 years,
almost 6.2 times more likely to develop PIH than age greater
than 35 years. Likewise, those women aged 18 to 24 years had
4.73 times more likely to develop PIH than age greater than
35 years. This finding similar to the study conducted in Dessie
Referal Hospital [5]. This could be explained as women get older
she is more likely to have cardiovascular problems. This would
particularly happen due to gradual loss of compliance of the
cardiovascular vessels that is mainly associated with ageing of
the uterine blood vessels and arterial stiffness. Besides, when the
woman gets older, the hemodynamic adaption during pregnancy
becomes more difficult [5].
In this study, an urban residence was 2 times more likely to
develop PIH than from rural residences. This finding might be
due to having those mothers who live in urban they experienced
different lifestyle than rural ones.
In our sample, mothers with a history of primigravida, 1.6 times
compared to Multigravida, a similar finding was recorded in the
study conducted in Karamara Hospital, Jijiga, Eastern Ethiopia.
A pregnant mother with a history of small gestational age in weeks
almost 5 times more likely was linked with the occurrence of PIH
than large for gestational age, which showed that women with a
gestational age greater than or equal to 37 weeks were less likely
to develop pregnancy-induced hypertension than women with
gestational age less than 37 weeks. This might be because the
population of this study was women attending delivery service so
that more women with PIH might be delivered before and around
37 weeks of gestational age to reduce the risk of maternal and
fetal complication. The study was similar to the study conducted
in Tigray regional state, Ethiopia, and was also similarly conducted
of the Omo district hospitals, Southern Ethiopia [2,20].
Those women with a history of PIH 1.4 times more, likely to
develop PIH than those without a history of PIH. This might have
occurred due to genetic factors that contribute to the physiologic
predisposition of PIH [5].
Those women with a history of DM 7 times more, likely to develop
PIH than without the PIH. This study also showed that women who had DM are at more risk to develop pregnancy-induced
hypertension than those who did not have DM. This is in line with
the study conducted in New York and Canada and similar to the
study conducted was also similarly conducted of the Omo district
hospitals, Southern Ethiopia [20-22]. This might be due to genetic
factors that predispose women to an increased risk of PIH and
recent studies done during pregnancy noted that mothers with a
history of diabetes mellitus may involve in the development of PIH
in which insulin resistance may play a role in the cause of PIH [20].
Conclusion
The prevalence of PIH among women receiving antenatal care
at Wachemo University's Nigist Eleni Mohammed Memorial
comprehensive and advanced Hospital was higher than in other
studies. Age, urban residence, primigravida, gestational age in
weeks (20 to 37 weeks), PIH history, and DM history were all
found to be significantly linked to PIH. Improving PIH screening,
care, and preventive strategies is important to improve maternal
and child health.
Acknowledgments
I am grateful to local health managers, data collectors, and
supervisors. Wachemo University is greatly acknowledged for
funding the study.
Authors’ Contributions
YM participated in the study design, undertook the field study,
analyzed data, and wrote the manuscript.
Funding
This study was sponsored by the Wachemo University (WCU), as
one of the 3rd generations higher Institution University, Hossana,
Ethiopia, as part of the annual research submitted to research
and community service. The funder had no role in the design of
the study, data collection, and analysis, interpretation of the data,
and preparation of the manuscript.
Ethics Approval and Consent to
Participate
The study was conducted after ethical approval was obtained from
the Institutional Review Board (IRB) of the Wachemo University
(WCU) College of Medicine and Health Sciences. Permission from
the Hadiya Public Health Institute and the health authorities of
the study sites was also received before the start of the study.
Before enrolment, participants were informed about the study,
its aims, effects, and importance of screening. Written consent
was obtained by trained data collectors. Then, participants were
subjected to full history taking through clinical examinations and
laboratory investigations. All information was made anonymous
to maintain confidentiality. Participants diagnosed with GDM
were referred to health providers and get possible treatment
options in their respective public Hospitals.
Consent
The author and the organizations listed here have agreed to be named and recognized. The confidentiality of the information
was also anonymously guaranteed and collected.
Availability of Data and Materials
The datasets used and analyzed during the current research are
available upon request from the corresponding author.
Conflicts of Interest
The writer notes that they do not have any conflicting interests.
Copyright
Before the article can be processed, all authors must sign the
"submission form" agreement and we all agreed to submit the
manuscript in your journal.
References
- Lakew Y, Reda AA, Tamene H, Benedict S, Deribe K (2013) Geographical variation and factors influencing modern contraceptive use among married women in Ethiopia: Evidence from a national population based survey. Reprod Health 10: 1-10.
- Berhe AK, Ilesanmi AO, Aimakhu CO, Mulugeta A (2020) Effect of pregnancy induced hypertension on adverse perinatal outcomes in Tigray regional state, Ethiopia: A prospective cohort study. BMC Pregnancy Childbirth 20: 1-11.
- Moodley J (2004) Maternal deaths associated with hypertensive disorders of pregnancy: A population-based study. Hypertens Pregnancy 23:247-56.
- National high blood pressure education program working on high blood pressure in pregnancy (2000) Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am J Obstet Gynecol 183:S1-S22.
- Tessema GA, Tekeste A, Ayele TA (2015) preeclampsia and associated factors among pregnant women attending antenatal care in dessie referral hospital, Northeast Ethiopia: A hospital-based study. BMC Pregnancy Childbirth 15: 1-7.
- Mekbeb T, Ketsela K (1991) Pre-eclampsia/eclampsia at Yekatit 12 Hospital, Addis Ababa, Ethiopia (1987-1989). East Afr Med J 68: 893-899.
- Abate M, Lakew Z (2006) Eclampsia a 5 years retrospective review of 216 cases managed in two teaching hospitals in Addis Ababa. Ethiop Med J 44: 27-31.
- (2016) Government of Ethiopia MPCU of M Central Statistical Agency-Population and Housing Census 2007-IPUMS Subset 8.
- Dolea C, AbouZahr C (2003) Global burden of hypertensive disorders of pregnancy in the year 2000. GBD 2000 Working Paper, World Health Organization, Geneva:1-11.
- Parveen N, Haider G, Shaikh IA, Din I, Ujjan (2009) Presentation of predisposing factors of pregnancy induced hypertension at Isra University Hospital, Hyderabad. JLUMHS 8: 242.
- (2019) Ethiopian Mini Demographic Health Survey (EMDHS). The World Bank.
- (2007) Census report.
- (2021) Annual report of Zone.
- (2014) Central Statistical Agency Addis Ababa, Ethiopia.
- Gudeta TA, Regassa TM (2019) Pregnancy induced hypertension and associated factors among women attending delivery service at mizan-tepi university teaching hospital, tepi general hospital and gebretsadik shawo hospital, Southwest, Ethiopia. Ethiop J Health Sci 29.
- Wolde Z, Segni H, Woldie M (2011) Hypertensive disorders of pregnancy in Jimma University specialized hospital. Ethiop J Health Sci 21.
- Mekonen L, Shiferaw Z, Wubshet E, Haile S (2018) Pregnancy Induced Hypertension and Associated Factors among Pregnant Women in Karamara Hospital, Jijiga, Eastern Ethiopia, 2015. J Pregnancy Child Health 5: 1-4.
- Teklu S, Gaym A (2006) Prevalence and clinical correlates of the hypertensive disorders of pregnancy at Tikur Anbessa Hospital, Addis Ababa, Ethiopia. Ethiop Med J 44: 17-26.
- Seyom E, Abera M, Tesfaye M, Fentahun N (2015) Maternal and fetal outcome of pregnancy related hypertension in Mettu Karl Referral Hospital, Ethiopia. J Ovarian Res 8: 1-7.
- Fikadu K, Meskel GF, Getahun F, Chufamo N, Misiker D (2021) Determinants of pre‐eclampsia among pregnant women attending perinatal care in hospitals of the Omo district, Southern Ethiopia. J Clin Hypertens 23: 153-162.
- Lehrer S, Stone J, Lapinski R, Lockwood CJ, Schachter BS, et al. (1993) Association between pregnancy-induced hypertension and asthma during pregnancy. Am J Obstet Gynecol 168: 1463-1466.
- Martel MJ, Rey É, Beauchesne MF, Perreault S, Lefebvre G, et al. (2005). Use of inhaled corticosteroids during pregnancy and risk of pregnancy induced hypertension: nested case-control study. BMJ 330: 230.