Research Article - (2024) Volume 9, Issue 2
Prevalence of Bottle Feeding Practice and Its Associated Factors among Mothers of Infants Less than Six Months at Addis Ababa Public Health Centers, Addis Ababa, Ethiopia, 2022
Gedifaw Birhan1*,
Shikur Mohammed2,
Sisay Tenia2,
Amanual Alem2,
Amlaku Alemante2 and
Abebe Belyneh2
1Department of Nursing, Addis Ababa University, Addis Ababa, Ethiopia
2Department of Public Health, Saint Paul Hospital Millennium Medical College, Addis Ababa, Ethiopia
*Correspondence:
Gedifaw Birhan, Department of Nursing, Addis Ababa University, Addis Ababa,
Ethiopia,
Tel: 918530728,
Email:
Received: 29-Jun-2023, Manuscript No. IPJHCC-23-16770;
Editor assigned: 03-Jul-2023, Pre QC No. IPJHCC-23-16770 (PQ);
Reviewed: 17-Jul-2023, QC No. IPJHCC-23-16770;
Revised: 05-Mar-2024, Manuscript No. IPJHCC-23-16770 (R);
Published:
12-Mar-2024, DOI: 10.36648/2472-1654.9.2.9012
Abstract
Introduct on: Bottle feeding practice should be avoided due to its influence on optimal breastfeeding
and its effect associated with morbidity and mortality resulting from diarrheal disease, infant and
child illness, and malnutrition. This study is aimed to assess the prevalence of bottle feeding practice
and its associated factors among mothers of infants less than six months in Addis Ababa.
Methods: An institution based cross-sectional study was conducted among 456 mothers who had
infants less than six months in Addis Ababa public health facilities. Data were collected through
interview, entered using Epi info version 7.1 and exported to statistical package for social science
version 26 for analysis. Variables with p-value <0.2 in bivariable binary logistic regression analysis
were entered to multivariable logistic regression analysis. Finally, variables with p-value <0.05 in
multivariable logistic regression were taken as significant factor.
Results: The overall prevalence of bottle feeding practice in this study was 39%. Being male infant
(AOR=0.589; 95% CI: 0.381, 0.911), infant hospitalization (AOR=2.114; 95% CI 1.246, 3.588),
cesarean section delivery (AOR=2.817; 95% CI: 1.764, 4.496), late initiation of breastfeeding
(AOR=5.526; 95% CI: 3.121, 9.786) and not having information on breast feeding (AOR=4.13; 95%
CI 2.21, 7.73) were statistically significant factors associated with bottle feeding practice.
Conclusion: The magnitude of bottle feeding practice is high in Addis Ababa. Being male infants,
infants hospitalized, cesarean section delivery, late initiation of breastfeeding and not having
information on breast feeding were significant factors for bottle feeding practice. Greater efforts
to promote breastfeeding should be targeted towards women with sub-optimal breastfeed.
Keywords
Bottle feeding; Prevalence; Associated factors; Malnutrition; Breastfeeding
Abbreviations
AOR: Adjusted Odds Ratio; ANC: Antenatal Care; BF: Bottle Feeding; CSA: Central
Statistics Agency; CI: Confidence Interval; COR: Crud Odds Ratio; ETB: Ethiopian Birr; EC: Ethiopian
Calendar; EDHS: Ethiopian Demographic and Healthy Survey; EPI: Expanded Program of
Immunization; HR: Hazards Ratio; HC: Health Center; IYCF: Infant and Young Child Feeding; NGO: Non-
Governmental Organization; RR: Relative Risk; SRS: Simple Random Sampling; SPSS: Statistical
Package for Social Science; WHO: World Health Organization.
Introduction
Adequate nutrition during the first two years of a child’s life is
essential to lower morbidity and mortality, reduce the risk of
chronic diseases, normal development and the future wellbeing
of the child [1]. The World Health Organization (WHO)
recommends optimal infant and young child feeding practices
which includes early initiation of breastfeeding within an hour
of birth, exclusive breastfeeding up to six months of age,
introduction of complementary feeding at six months and
continuing breast feeding up to 2 years or beyond and
ensuring proper use of breast milk substitutes [2].
Bottle feeding is an infant feeding modality that has been in
existence since ancient times and currently a significant
number of infants are being fed via a bottle with either breast
milk or breast milk substitutes (formula) [3]. Globally, 59% of
infants and around 85% of infants within Australia by five
months of age are being fed with either breast milk or
formula using bottles [4]. Breastfeeding is declining in almost
all over the world despite its nutritional and immunological
advantages. Improper breastfeeding practices may
significantly compromise the health, development and
survival of infants, children, and mothers [5]. Worldwide it
causes 820,000 children and 20,000 maternal deaths in a year.
It has been also found that non-exclusive breast feeding
(bottle feeding) in the first 6 months of life results in 1.4
million deaths and 10% of the disease burden in children
younger than 5 years [6].
Bottle feeding practices in infancy and childhood led to the
high prevalence of malnutrition, increased morbidity and
mortality in children in the developing world. Malnutrition
accounts for around two-thirds of all deaths among children
under the age of five worldwide. Each year more than 10
million children die as a result of malnutrition; 98% of these
deaths occur in underdeveloped countries. Death rates in
third world countries are lower among breastfed babies and
breastfed babies have lower infections than formula fed
babies [7].
In Ethiopia suboptimal breastfeeding practices are the most
contributor around 70,000 infant deaths per year; 24% of the
total infant death annually and that be significantly prevented
by nutrition interventions such as exclusive breastfeeding [8].
Bottle feeding is one of the major causes of diarrhea among
the infants. The rate of bottle feeding practice keeps on
increasing among the mothers with infants older than four
months due to early weaning [9]. The major reasons for
bottle-feeding practice include insufficient breast milk, the
need to go back to work, maternal work load and illness, delayed ANC follow up, caesarean section mode of delivery
and improper birth spacing [10,11].
Even though, WHO recommends avoidance of bottle feeding,
there is a current shift from traditional feeding practice(bottle
feeding) towards shorter breast feeding and introduction of
bottle feeding in developed countries and urban communities
of developing countries [12]. Practice of bottle feeding and
associated factors are rarely addressed in urban community of
Ethiopia including Addis Ababa. So, this study aimed to fill this
gap and assess the prevalence of bottle feeding practice and
associated factors among mothers of infants less than six
month in Addis Ababa, Ethiopia.
Materials and Methods
Study Area and Period
The study was conducted from July 1, 2022 to July 30, 2022 in
public health centers of Addis Ababa, Ethiopia. Addis Ababa
has almost 4 percent of the Ethiopian populations with 11
per cent of under five years children [13]. The total population
of Addis Ababa is 3,602,000; 1,134,150 are under five children
according to 2019 projection based on the 2007 census [14].
In Addis Ababa there are around 116 health centers in eleven
sub cites [15].
Study design: An institutional based cross sectional study
design was conducted.
Study Population and Eligible Criteria
All mothers who have infants less than six months in Addis
Ababa were considered in the study. Those mothers who have
infants less than six months at selected health center were
included in the study. Mothers who have repeated visits
during the study period will be excluded from the study.
Sample Size Determination
The sample size required for the study is calculated using epi
info application or the formula of simple proportion
estimation:
n=n=(Zα/2)2 (p) (1-p)/d2
Where;
n=The minimum sample size required.
P=Proportion of bottle feeding associated factor in study done
at woldia hospital, maternal age 35-50 years (23.4%) [16].
Zα2⁄=Standard normal value at (1-α) 95.
Confidence level=95%.
Margin of error (d)=5%.
Design effect (de)=1.5 is used.
The sample size “n” for associated factor of bottle feeding
=(1.96)2(0.234) (1-0.234)/(0.05)2=275, since study uses multi
stage sampling, 1.5 design effect was used then the sample
size would be 414. The final sample size after addition of 10%
non-response rate was 456.
Sampling Technique
Multi stage sampling technique was employed to include
study participants in to the research. First from a total of 11
sub cities three sub cities were selected using simple random
sampling technique. Since 20% to 30% of the study
population represents the total population, average 25% of
Sub Cities (SC) was used to represent the population.
In the first stage of sampling, 25% of eleven sub cities (three
sub cities) Areda, Kolife Karanio and Nifas silk lafito sub cities
were selected by using simple random sampling technique.
These three sub cities have a total of 27 health centers
(Areda=7, Kolife Karanio=9 and Nifas silk lafito=11); 25% of 27
(seven) were used to allocate study participants in each
selected sub cities. The seven Health Centers (HC) (Areda=2,
Kolife Karanio=3, Nifas silk lafito=3) are allocated according to
the number of health centers in each sub cities.
In stage second sampling, Beta and Simegn Kebede health
center from Areda sub city, woreda 1, 3 and 4 health center
from Kolife Karanio sub city and woreda 2, 5 and 10 HC from
Nifas silk lafito sub city were selected by lottery method.
The registration of mothers who have infant less than 6
months on expanded program of immunization register was
used to get list of children from each health centers. Sample
from each health center was determined by using proportion
allocation to the sample size.
Finally, systematic random sampling technique was used to
select a representative population in the immunization unit.
The sampling interval (K) was established by dividing the
average number of women who visited the immunization unit
in the previous two months before data collection (average
n=2660) by the sample size, which produced K=2660/456=6.
Women were recruited daily by simple random sampling
technique using the lottery method, and the next respondent
was selected by adding a sampling interval to the number of
the selected women. The same procedure was done on
subsequent days until the required sample size was reached.
Proportional Allocation
In three selected sub cities there were 2660 children less than
6 months of age. Out of this 335 in Beta health center, 277 in
Simegn Kebede health center from Areda sub city, 360 in
woreda 1 health center, 431 in woreda 3 health center and
245 from woreda 4 health center of Kolife Karanio sub city
and 365 in woreda 2 health center, 347 woreda 10 health center and 300 from woreda 5 health center of Nifas silk lafito
sub city.
Based on proportional allocation to size, 456 study subjects
were distributed to Beta health center (57), Simegn Kebede
health center (47) from Areda sub city; woreda 1 health
center (42), woreda 3 health center (74) and woreda 4 health
center (62) of Kolife Karanio sub city and woreda 2 health
center (63), woreda 10 health center (60) and 300 from
woreda 5 health center (51) of Nifas silk lafito sub city.
Data Collection Procedure
Data was collected by face to face interview using semistructured
pretested questionnaire. The questionnaire was
administered through face to face interview by five (5) trained
data collectors (diploma nurse) and the data collection was
supervised by two BSC health workers.
The questionnaire was constructed by adopting and
modifying from previous studies. First, the questionnaire was
prepared in English then translated into Amharic (local
language) and then back to English to check consistency.
The quality of the data collection process was monitored, and
clear uniform instructions were given to all data collectors. All
data collected as a part of this study was checked by the
principal investigator.
Operational Definitions
Exclusive breastfeeding: A mother gives to infant only breast
milk.
Maternal illness: Mothers difficulty to breastfeed an infant
due to illness (breast illness related problem).
Mixed breastfeeding: If an infant took breast milk with
addition of liquid foods like cow milk and formula milk and
soft foods.
Adequate knowledge: If a mother answers half and above
correctly from questions which are asked to measure bottle
feeding knowledge.
Inadequate knowledge: If a mother answers below half
correctly from questions which are asked to measure bottle
feeding knowledge [17]. Late initiation of breastfeeding:
Initiation of breast milk after one hour after delivery.
Bottle feeding: Mother uses bottle for Brest milk and or
breast milk substitutes (formula or others) [18].
Data Quality Control
In order to assure the quality of the data; a pre-test was
conducted on 5% of the sample size at Abinet health center
from mothers’ infants visiting for immunization before the
actual data collection to ensure the completeness and
consistency. In addition, one day training was given to data
collectors and the supervisor about the aim of the study,
about the data collection tools, and how to obtain
information [19]. The principal investigator undergoes quality
assessment on ongoing supervision each day during data collection to ensure quality of data by checking filled format
for their completeness’s and consistency. Data reliability was
checked by considering the Cronbach alpha which is greater
than or equal to 0.5 and multicollinearity between variables
was also checked by considering Variance Inflation Factor (VIF)
which is less than 2 which indicates there is no correlation
between independent variables [20].
Data Management and Analysis
Data obtained from institution based survey was checked for
completeness and inconsistencies, then coded, entered and
cleaned in the Epi info version 7.1 and Microsoft excel and
analyzed using Statistical Package for Social Sciences (SPSS)
version 26. After categorizing and defining variables,
descriptive analysis was carried out for each of the
independent variables using frequencies, cross tabulation and
percentages: Then presented by text, tables and chart.
Binary logistic regression analysis model was used to assess
the association between bottle feeding and associated factors
[21]. Variables with p-value <0.2 in bivariable binary logistic
regression analysis were entered to multivariable binary logistic regression analysis. Finally, variables with p-value
<0.05 in multivariable logistic regression were taken as
significant factor. Adjusted odds ratio with 95% CI was used to
show the strength of association between the dependent and
independent variables. Model fitness was tested with Hosmer
and Leme show goodness of fit test and fit with a pvalue=
0.440. In addition, there was no problem of
multicollinearity among explanatory variables, with variance
inflation factor <3 for all variables [22].
Results
Socio-demographic Characteristics
In this study, a total of 451 study participants were included
with a response rate of 98.9%. Among the study participants
most of the study participants, 444 (98.4%) were married.
Regards to religion more than half 235 (52.1%) were
orthodox. Related to occupation, 202 (44.8%) of mothers
were house wife (Table 1) [23].
| Variable |
Categories (N=451) |
Frequency |
Percent |
| Mothers age (years) |
18-23 |
118 |
26.20% |
| 24-29 |
202 |
44.80% |
| 30-35 |
94 |
20.80% |
| Above 35 |
37 |
8.20% |
| Marital status |
Married |
444 |
98.40% |
| Other |
7 |
1.60% |
| Religion |
Orthodox Christian |
235 |
52.10% |
| Muslim |
128 |
28.40% |
| Protestant |
76 |
16.90% |
| Catholic |
12 |
2.70% |
| Maternal education |
Unable to read and write |
31 |
6.90% |
| Primary school |
139 |
30.80% |
| Secondary and preparatory |
169 |
37.50% |
| Higher education |
112 |
24.80% |
| Husbands’ education |
Unable to read and write |
8 |
1.80% |
| Primary school |
105 |
23.30% |
| Secondary and preparatory |
169 |
37.50% |
| Higher education |
169 |
37.50% |
| Maternal occupation |
Housewife |
202 |
44.80% |
| Government employ |
69 |
15.30% |
| Private organization employee |
79 |
17.50% |
| Merchant |
76 |
16.90% |
| Daily labor |
25 |
5.50% |
| Husbands’ occupation |
Government employ |
101 |
22.40% |
| Private organization employee |
133 |
29.50% |
| Merchant |
141 |
31.30% |
| Daily labour |
76 |
16.90% |
| Monthly household income |
1500 birr-4500 birr |
89 |
19.70% |
| 4501 birr-7500 birr |
162 |
35.90% |
| 7501 birr-10000 birr |
127 |
28.20% |
| Above 10001 birr |
73 |
16.20% |
Note: Others=Single and divorced
N=Number.
Table 1: Socio-demographic characteristics mothers (respondents) who have infants less than six months old, in Addis Ababa: Ethiopia, 2022.
Obstetric and Health Service Utilization Factors
In this study, 449 (99.6%) mothers had antenatal care in their
previous pregnancy. During their antenatal care follow up, 87
(19.6%) of women did not receive counseling about infant
feeding practice. The majority of the respondents 437 (96.9%) were give birth at health institution and 14 (3.1%) were
give birth at home. From 356 (78.9%) of mothers
received postnatal care, 289 (69.2%) had received counseling
on infant feeding up to six months (Table 2).
| Variable |
Response (N=451) |
Frequency |
Percent |
| Infant age |
0-3 months |
332 |
73.60% |
| 4-6 months |
119 |
26.40% |
| Infant gender |
Male |
268 |
59.40% |
| Female |
183 |
40.60% |
| Numbers of children |
1 |
196 |
43.50% |
| 2-5 |
254 |
56.30% |
| Six and above 6 |
1 |
0.20% |
| Birth order |
First |
195 |
43.20% |
| Second |
180 |
39.90% |
| Third |
59 |
13.10% |
| Fourth and above |
17 |
3.80% |
| Birth interval from preceding birth |
1-2 |
94 |
36.40% |
| 3-4 |
119 |
46.10% |
| Above 4 |
45 |
17.40% |
| ANC follow up |
Yes |
449 |
99.60% |
| No |
2 |
0.60% |
| Receive infant feeding counseling during ANC visit (N=449) |
Yes |
362 |
80.60% |
| No |
87 |
19.40% |
| Place of delivery |
Health institution |
437 |
96.90% |
| Home |
14 |
3.10% |
| Mode of delivery |
Cesarean section |
120 |
26.60% |
| Spontaneous delivery |
331 |
73.40% |
| Infant hospitalization |
Yes |
87 |
19.30% |
| No |
364 |
80.70% |
| PNC follow up within 45 days of delivery |
Yes |
356 |
78.90% |
| No |
95 |
21.10% |
| Receive infant feeding counseling during PNC visit (N=356) |
Yes |
289 |
79.20% |
| No |
76 |
20.80% |
Table 2: Obstetric and health service utilization characteristics of study participants in Addis Ababa, Ethiopia, 2022.
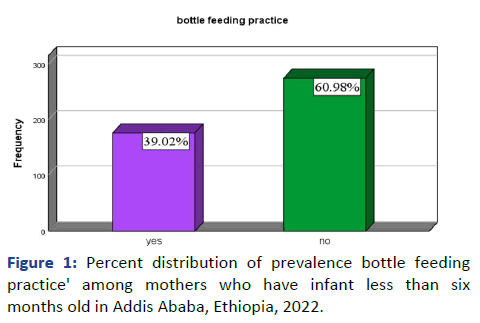
Prevalence of Bottle Feeding Practice
Prevalence of bottle feeding practice was 39% (95% CI 35, 44).
The following Figure shows the prevalence of bottle feeding
practice among mothers who have infants less than six month
(Figure 1). Among respondents who used bottles for feeding,
103 (58.9%) used formula, 30 (20.8%) used expressed breast
milk and 5(3.5%) used caws milk. In this study in luential
bodies of mothers to start bottle fed were health professional
67 (30.7%), husbands 40 (18.3%) and mothers 17 (7.8%)
(Table 3).
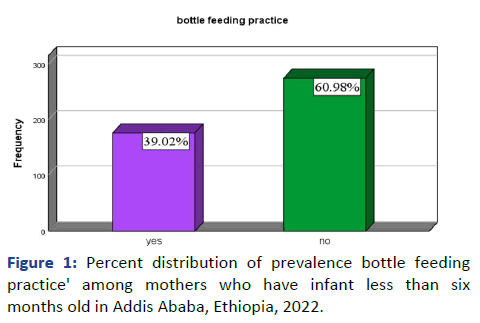
Figure 1: Percent distribution of prevalence bottle feeding
practice' among mothers who have infant less than six
months old in Addis Ababa, Ethiopia, 2022.
| Variable |
Response |
Frequency |
Percent |
| Initiation of breast feeding. |
Immediately after birth |
122 |
27.1 |
| After one hour |
131 |
29 |
| When mother feels comfort |
103 |
22.8 |
| I did not feed breast milk |
95 |
21.1 |
| Kinds of fluid you feed if not breast feed (N=144) |
Caws milk |
5 |
3.5 |
| Formula milk |
109 |
75.7 |
| Expressed breast milk |
30 |
20.8 |
| Youngest infant currently feed |
Breast feeding |
275 |
61 |
| Bottle feeding |
176 |
39 |
| Bottle feeding (N=451) |
Yes |
176 |
39 |
| No |
275 |
61 |
| Duration of bottle feed (N=156) |
0-3 months |
134 |
76.1 |
| 4-6 months |
42 |
23.9 |
| Influence to bottle feed (N=218) |
Own decision |
92 |
42.2 |
| Mother |
17 |
7.8 |
| Husband |
40 |
18.3 |
| Health professionals |
67 |
30.7 |
| Friends or family |
2 |
0.9 |
Table 3: Bottle feeding related practices of mothers who have infants less than six months old in Addis Ababa: Ethiopia, 2022.
Bottle Feeding Related Factors
All mothers have breastfeed their current infant for a certain
period of time. From total, 122 (27.1%) mothers initiated
breast milk to infant immediately within one hour of birth and
131 (29%) mothers initiated breast milk to infant after one
hour of birth, whereas 103 (22.8%) initiates breast feeding
after mother feels comfort after delivery. In this study,
Influential bodies of mothers to start bottle feeding were
health professional 67 (30.7%), husbands 40 (18.3%) and
mothers 17 (7.8%).
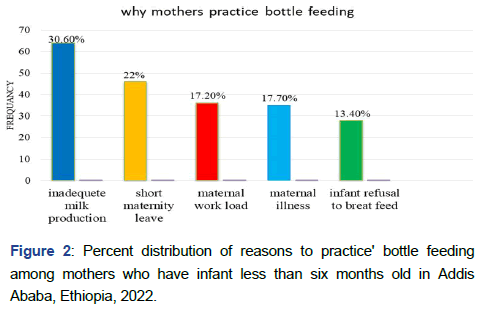
The following diagram also shows the reason why mother
who have infants less than six month practice bottle feeding
(n=209) (Figure 2).
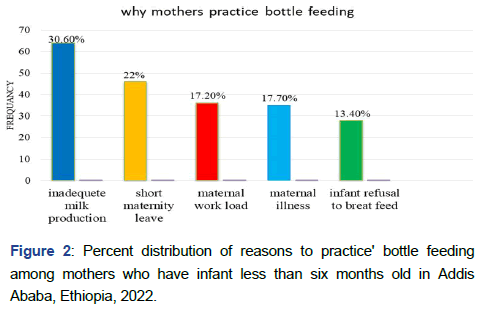
Figure 2: Percent distribution of reasons to practice' bottle feeding
among mothers who have infant less than six months old in Addis
Ababa, Ethiopia, 2022.
Mothers’ Knowledge and Information Source of Bottle
Feeding
Around two third (61.4%) of mother's who have infant
less than six month have adequate knowledge on bottle
feeding, whereas 38.6% of mother's who have infant
less than six month haven’t adequate knowledge on bottle
feeding [24].
Regarding to information about bottle feeding 352
(78.3%) mothers was informed about bottle feeding from
different sources (Table 4).
| Variable |
Response |
Frequency |
Percent |
| Have you ever heard bottle feeding |
Yes (informed) |
353 |
78.30% |
| No (not informed) |
98 |
21.70% |
| Source of information on bottle feeding (N=353) |
Mass media |
66 |
18.70% |
| Health facilities |
136 |
38.50% |
| Friends and family |
149 |
42.20% |
| Books and leaflets |
2 |
0.60% |
| Maternal knowledge on bottle feeding |
Inadequate knowledge |
174 |
38.60% |
| Adequate knowledge |
277 |
61.40% |
Table 4: Information and source information on bottle feeding among mothers who have infants less than six months old in Addis Ababa: Ethiopia, 2022.
Factors Associated with Bottle Feeding Practice
Binary logistic regression model was used to determine the
association between independent variables with dependent
variable. Variables which were associated with bottle feeding
practice in the bivariable binary logistic regression analysis
(p<0.2) were; gender of infant, initiation of breast milk,
mothers education, place of delivery, mode of delivery,
monthly household income, infant hospitalization,
information herd about bottle feeding and mothers
knowledge about bottle feeding. Variables which were
associated in bivariable binary logistic regression analysis
were tested in the final multivariable binary logistic regression
analysis to see their significant association with bottle feeding
practice.
By using backward likelihood ratio method multivariable
logistic regression analysis; infant gender, infant
hospitalization, mode of delivery, heard about bottle feeding
and initiation of breast milk were remained significant in the
final model. Model fitness was tested with Hosmer and
Lemeshow Goodness of fit test and fit with a p-value =0.440.
In addition, there was no problem of Multicollinearity among
explanatory variables, with variance inflation factor <3 for all
variables. After adjusting confounding variables the finding of
this study revealed that the odds of bottle feeding practice
among mothers having infants less than six months who had
male infant were 59% less likely to bottle feed than infants of
female gender AOR=0.589 (95% CI: 0.381, 0.911).
Mode of delivery was significantly associated with bottle
feeding practice. mothers who gave birth through cesarean
section were 2.8 times more likely to practice bottle feed than
mothers give birth via spontaneous delivery AOR=2.817 (95%
CI: 1.764, 4.494). Similarly, infant hospitalization after delivery
is significant for mothers to bottle feed an infant. Infants who
were hospitalized after delivery were almost 2 times more
likely to practice bottle feeding than infants who were not
hospitalized AOR=2.114 (95% CI: 1.246, 3.588). In addition,
time of initiation breast feed was significantly associated with
bottle feeding practice. Mothers who initiate breast fed after
one hour were 5.5 times more likely to practice bottle feeding
than mothers who initiate breast feed immediately after birth
(within one hour) AOR=5.526 (95% CI: 3.121, 9.786).
Furthermore, mothers who have no information on bottle
feeding were significantly associated with bottle feeding
practice. Lastly, mothers not having information about bottle
feeding were 4 times more likely to practice than mothers not
having information about bottle feeding AOR=4.131 (95% CI:
2.208, 7.729) (Table 5).
| Bottle feeding |
| Variable |
Frequency |
COR |
AOR |
P value |
| Yes |
No |
| Infant gender |
Male |
93 |
175 |
0.64 (0.436, 0.941) |
0.589 (0.38,0.9) |
0.017 |
| Female |
83 |
100 |
1 |
|
|
| Maternal education |
Unable to read and write |
10 |
21 |
0.476 (0.21,1.10) |
|
|
| Primary school |
43 |
96 |
0.448 (0.27,0.75) |
|
|
| Secondary and preparatory |
67 |
102 |
0.657 (0.40,1.06) |
|
|
| Higher education |
56 |
56 |
1 |
|
|
| Monthly household income |
1500-4500 birr |
32 |
57 |
0.414 (0.22, 0.78) |
|
|
| 4501-7500 birr |
49 |
113 |
0.320 (0.18, 0.57) |
|
|
| 7501-10000 birr |
53 |
74 |
0.528 (0.29,0.94) |
|
|
| Above 10001 |
42 |
31 |
1 |
|
|
| Place of delivery |
Health institution |
173 |
264 |
2.403 (0.66,8.74) |
|
|
| Home |
3 |
11 |
1 |
|
|
| Mode of delivery |
Caesarean section |
77 |
53 |
3.258 (2.14,4.97) |
2.82 (1.76, 4.5) |
<0.001 |
| Spontaneous delivery |
99 |
222 |
1 |
|
|
| Infant hospitalization |
Yes |
51 |
41 |
2.329 (1.46,3.71) |
2.11 (1.25,3.59) |
0.006 |
| No |
125 |
234 |
1 |
|
|
| Time of initiation of breast feeding |
After one hour (late) |
157 |
172 |
4.948 (2.89,8.449) |
5.53 (3.12,9.79) |
<0.001 |
| Within one hour (early) |
19 |
103 |
1 |
|
|
| Have ever heard about bottle feeding |
No(not informed) |
161 |
192 |
4.64 (2.58, 8.36) |
4.13 (2.21,7.73) |
<0.001 |
| Yes (informed) |
15 |
83 |
1 |
|
|
Table 5: Bivariable and multivariable logistic regression analysis for factors associated with bottle feeding practice among mothers having infant less than 6 months at Addis Ababa health centers, Addis Ababa, Ethiopia, 2022.
Discussion
The aim of this study was to assess the prevalence of bottle
feeding practice and associated factors among infants less
than six months in Addis Ababa public health centers. In this
study, the prevalence of bottle-feeding practice was 39% (95%
CI: 35-44). This result is consistent with the studies done at
East Africa (Comoros), Sudan and Woldia, Ethiopia. On the
other hand, the result of this study is higher compared to the
national prevalence reported in the 2019 EDHS 22%, studies
conducted at Mettu town, Namibia, Nine East and South East
Asian countries and Nigeria. The possible reason for this
difference might be attributed to study period variation, as
there has been increasing advocacy for using formula in this
region recently and urbanization. In contrast, the prevalence
of bottle feeding in this study is lower than studies conducted
at Debrelibanos Ethiopia, Pakistan and Nine East and South
East Asian countries (Philippines). The difference might be
due to methodological variations between studies,
dissimilarities in infant and maternal socio-demographic
characteristics and other differences in sociocultural,
economical, health and health service utilization
characteristics between respondents of the referenced areas
and the study place.
The main reasons mentioned by mothers for bottle feeding in
this study are insufficient breast milk production for infants
(30.6%), short maternity leave (22%), and maternal work load
in house and outside house to breast feed (17.2%), maternal
illness (17.7%) and infant refusal to breast feed due to
childhood illness (13.40%). These results are consistent with
other studies done in Holata, Agaro, Namibia, Benghazi Libya,
Mauritius and Pakistan.
Short maternal leave (3 months) makes mothers prompted
to resort to the supplementation of infant formula before 3
months so that their infants familiarize to bottle feeding
during their absence, resumption of work, perception of
breast milk insufficiency and infants sucking problem are
factors that hiders breast feeding and facilitates for choosing
bottle feeding.
According to this study, mothers who gave birth through
cesarean section were 2.8 times more likely to practice bottle
feed than mothers give birth via spontaneous delivery.
This result is in line with studies conducted at Namibia,
Libya, Pakistan and India. This resulted due to delayed
initiation of breast feeding because of mothers take long
time to recover from anesthesia and additional discomfort.
Similarly, gender of the infant was significantly associated
with bottle feeding practice. An infant who is male was 59%
less likely to bottle feed than infants of female gender. This
result is similar with studies done in India this is due to
mothers belief of males high nutritional requirement
construction of gender influence to increase bottle feeding.
Among the various obstetric and health service utilization
factors assessed, infant hospitalization was significantly
associated with bottle feeding practice. Infants who were
hospitalized after delivery were almost 2 times more likely to
practice bottle feeding than infants who were not
hospitalized. This result is similar with studies done in India,
Kassel, eastern Sudan and Ethiopia particularly Holeta and
Agaro towns. This may result due infants sucking problem as
result of childhood illness that makes them to admit to
hospital [25].
Late initiation breast feed was significantly associated with
bottle feeding practice. Mothers who initiate breast fed after
one hour were 5.5 times more likely to practice bottle feeding
than mothers who initiate breast feed immediately after birth
(within one hour). This result is in line with studies done in
Wuhan, China, Hula (Sidama Ethiopia) and Debra Birhan,
Ethiopia. This might be due maternal illness (pain full breast
experience), delayed milk secretion, caesarean section mode
of delivery, infant inability to suck breast and low counseling
service during ANC and PNC.
Access to information seems to affect a mother’s decision on
infant and young child feeding. Mothers who have no
information on bottle feeding was significantly associated
with bottle feeding practice. Mothers who haven’t
information about risk of bottle feeding were 4 times more
likely to practice bottle fed than mothers having information
about bottle feeding AOR=4.131( 95% CI: 2.208, 7.729).
This study supports study conducted in in Benghazi, Libya.
This may be resulted due to lack of information about
benefits of breastfeeding for mother and child and risks
followed after bottle feeding like diarrhea and other botte
sanitation related infections. Finally, lack of indication on
seasonal variation of bottle feeding, inclusion of only
governmental health centers and qualitative method of study
was limitation this study [26].
Conclusion
The overall prevalence of bottle feeding practice high in the
study area (39%) as compared to national prevalence (22%).
male infant, infant hospitalized, cesarean section delivery and
late initiation of breastfeeding. infant hospitalization and late
initiation of breast feeding and not having information on
bottle feeding were significant factors associated with bottle
feeding practice. Therefore, increasing breast feeding practice
and avoid bottle feeding practice, provide continuous
breastfeeding education, training of health care workers to
strengthen maternal and child health services increase
maternity leave are recommendations of the study.
Ethical Approval
The study was conducted after getting ethical clearance from
the institutional review board of Saint Paul hospital
millennium medical collage ethical review committee
(reference number PML3/757, on 9/6/2022) and Addis Ababa
health bureau public health research and emergency
management department(reference number A/A/16172/227,
on 23/6/2022). In addition, letters of authorization was
obtained from Areda sub city health office, Kolife Karanio sub
city and Nifas silk Lafto sub cities before contacting the
participants. The participants were then fully briefed about
the study’s purpose and benefits in their local language and
obtained informed written consent for both data collection
and publication. Confidentiality was maintained through
anonymity and privacy measures were taken to preserve the
right of the participants throughout the research work
including publication. Finally, the selected participants were
asked about their willingness to join the study. Any study participant willing to engage in the study and those who
wanted to stop an interview at any time were allowed to do
so. This study was conducted in accordance with the
declaration of Helsinki.
Consent for Publication
Not applicable.
Availability of Data and Materials
The datasets analyzed during the current study are available
from the corresponding author upon reasonable request.
Competing Interest
The authors declare that they have no competing interest.
Funding
There were no external organizations that funded this
research.
Authors' Contribution
GB developed the project, manage resource, and perform
supervision and investigation. GB, ST, SM, AA3, BM and AB,
participated in the methodology. GB, SM, ST, AA2, AA3 in data
analysis and conceptualization (developing the initial drafts of
the manuscript) and revising subsequent drafts. GB, AA2 and
SM prepared the final draft of the manuscript. All authors
read and approved the final manuscript.
Acknowledgment
We would like to thank Saint Paul hospital millennium medical
college to support this research project. The authors would
also like to extend their gratitude to Addis Ababa health
centers, data collectors and supervisor for their valuable
contribution.
References
- Rahman A, Akter F (2019) Reasons for formula feeding among rural Bangladeshi mothers: A qualitative exploration. PLoS One. 14(2):e0211761.
[Crossref] [Google Scholar] [PubMed]
- Kebebe T, Assaye H (2017) Intention, magnitude and factors associated with bottle feeding among mothers of 0-23 months old children in Holeta town, Central Ethiopia: A cross sectional study. BMC Nutr. 3(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Wu H, Zhao M, Magnussen CG, Xi B (2021) Global prevalence of WHO infant feeding practices in 57 LMICs in 2010-2018 and time trends since 2000 for 44 LMICs. EClinical Medicine. 37:100971.
[Crossref] [Google Scholar] [PubMed]
- Kotowski J, Fowler C, Hourigan C, Orr F (2020) Bottle-feeding an infant feeding modality: An integrative literature review. Matern Child Nutr. 16(2):e12939.
[Crossref] [Google Scholar] [PubMed]
- Tewabe T (2015) Assessment of exclusive breast feeding practice and associated factors among mothers in Motta town, East Gojam zone, Amhara reginal state. Addis Ababa University. 2:1-15.
[Google Scholar]
- Dibley MJ, Senarath U, Agho KE (2010) Infant and young child feeding indicators across nine East and Southeast Asian countries: An analysis of national survey data 2000-2005. Public Health Nutr. 13(9):1296-1303.
[Crossref] [Google Scholar] [PubMed]
- Kera AM, Zewdie A, Akafu W, Kidane R, Tamirat M (2003) Formula feeding and associated factors among mothers with infants 0-6 months old in Mettu town, Southwest Ethiopia. Food Sci Nutr. 11(7):4136-4145.
[Crossref] [Google Scholar] [PubMed]
- Federal M (2004) National strategy for infant and young child feeding. Int J Innov Sci Res Technol. 1504–1510.
- Makwana DN (2020) Determinants of bottle feeding among 0-24 months children. Pediatr Rev: Int J Pediatr Res. 7(1):14-21.
[Google Scholar]
- Seid SS, Muluneh E, Sinbirro IA, Moga TT, Haso TK, et al. (2019) Utilization of bottle feeding practices and associated factors among mothers who have infant less than 12 months of age in Agaro town, Jimma zone South West Ethiopia, 2018. Health Sci J. 13(1):1-10.
[Google Scholar]
- Science F (2014) Determinants of child feeding practices in Pakistan; secondary data analysis of demographic and health survey 2006-07. J Med Nutr Nutrac. 3(2):78.
[Google Scholar]
- Andea F, Nida H, Jira C (2003) Infant bottle feeding practice, Agaro town, Southwest Ethiopia. Ethiop J Heal scince. 13(1):51-58.
[Google Scholar]
- Hassan AA, Taha Z, Abdulla MA, Ali AAA, Adam I (2019) Assessment of bottle feeding practices in Kassala, Eastern Sudan: A community-based study. Open Access Maced J Med Sci. 7(4):651-656.
[Crossref] [Google Scholar] [PubMed]
- UNICEF (2019) Situation analysis of children and women: Addis Ababa. UNICEF.
[Google Scholar]
- Mihret Y, Endalew F, Almaw H, Linger M (2020) Sociodemographic factors associated with bottle feeding practices in infants under two years of age: A hospital based study in Woldia, Ethiopia. Cent Asian J Glob Health. 9(1):e440.
[Crossref] [Google Scholar] [PubMed]
- Ekubagewargies DT, Mekonnen HS, Siyoum TM (2019) Assessment of knowledge, attitude, and practice of HIV positive mothers on antiretroviral treatment towards infant feeding in Gondar town health institutions, North West Ethiopia, 2017. Int J Pediatr. 2019:9107989.
[Crossref] [Google Scholar] [PubMed]
- Birhan TY, Birhan NA, Alene M (2021) Pooled prevalence and determinants of prelacteal feeding practice in Eastern Africa evidence from demographic and health survey data: A multilevel study. Risk Manag Healthc Policy. 14:1085-1095.
[Crossref] [Google Scholar] [PubMed]
- EPHI (2021) Ethiopia mini demographic and health survey. Ethiopian Public Health Institute. 1-25.
- Berde AS (2018) Factors associated with bottle feeding in Namibia: Findings from Namibia 2013 demographic and health survey. J Trop Pediatr. 64(6):460-467.
[Crossref] [Google Scholar] [PubMed]
- Akinyinka MR, Olatona FA, Oluwole EO (2016) Breastfeeding knowledge and practices among mothers of children under 2 years of age living in a military barrack in Southwest Nigeria. Int J MCH AIDS. 5(1):1-13.
[Crossref] [Google Scholar] [PubMed]
- Mekonnen M, Kinati T, Bekele K, Tesfa B, Hailu D, et al. (2021) Infant and young child feeding practice among mothers of children age 6 to 23 months in Debrelibanos district, North Showa zone, Oromia region, Ethiopia. PloS One. 16(9):e0257758.
[Crossref] [Google Scholar] [PubMed]
- Motee A, Ramasawmy D, Pugo-Gunsam P, Jeewon R (2013) An assessment of the breastfeeding practices and infant feeding pattern among mothers in Mauritius. J Nutr Metab. 2013:243852.
[Crossref] [Google Scholar] [PubMed]
- Abdulmalek LJ (2018) Factors affecting exclusive breast feeding practices in Benghazi, Libya. Libyan J Sci Techno. 7(1):36-38.
[Google Scholar]
- Huang L, Xu S, Chen X, Li Q, Lin L, et al. (2020) Delayed lactogenesis is associated with suboptimal breastfeeding practices: A prospective cohort study. J Nutr. 150(4):894-900.
[Crossref] [Google Scholar] [PubMed]
- Hoche S, Meshesha B, Wakgari N (2018) Sub-optimal breastfeeding and its associated factors in rural communities of Hula district, Southern Ethiopia: A cross-sectional study. Ethiop J Health Sci. 28(1):49-62.
[Crossref] [Google Scholar] [PubMed]
- Gultie T, Sebsibie G (2016) Determinants of suboptimal breastfeeding practice in Debre Berhan town, Ethiopia: A cross sectional study. Int Breastfeed J. 11:5.
[Crossref] [Google Scholar] [PubMed]
Citation: Birhan G, Mohammed S, Tenia S, Alem A, Alemante A, Belyneh A (2024) Prevalence of Bottle Feeding Practice and Its
Associated Factors among Mothers of Infants Less than Six Months at Addis Ababa Public Health Centers, Addis Ababa, Ethiopia,
2022. J Health Commun. 9:9012.
Copyright: © 2024 Birhan G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution
License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source
are credited.