Review Article - (2017) Volume 3, Issue 5
Syed Aoun Muhammad Jafri1, Maha Ali2, Rabiya Ali2, Saifullah Shaikh2, Marium Abid1 and Iram Saddiqa Aamir2*
1Department of Community Health Sciences, Jinnah Medical College, Karachi, Pakistan
2Bahria University Medical and Dental College, Karachi, Pakistan
*Corresponding Author:
Iram Saddiqa Aamir
Department of Physiology
Bahria University Medical and Dental College
Karachi, Pakistan
Tel: +92 21 3452244987, +92 213003524750
E-mail: doctoriramaamir@yahoo.com
Received Date: July 21, 2017; Accepted Date: August 21, 2017; Published Date: August 31, 2017
Citation: Jafri SAM, Ali M, Ali R, Shaikh S, Abid M, et al. (2017) Prevalence of Depression among Pregnant Women Attending Antenatal Clinics in Pakistan. Acta Psychopathol. 3:54. doi: 10.4172/2469-6676.100126
Background: Depression is primarily a mood disorder affecting every 1 in 4 women at some point in time during their life, so it shouldn’t come as a surprise that this illness can also find its way to women who are with child. But much often, depression is misdiagnosed at the time pregnancy because mostly hormonal fluctuations that occurs in a woman are thought to be bringing about such changes. In hope of a way to diagnose at a very initial stage and further on apply preventive measures, prevalence of depression among pregnant women must be determined first. Data available to us that shows how prevalent depression is during pregnancy vary considerably. We are in need of a relatively more concise estimate that is essential to identify the level of disease burden that depression brings and develop strategies for managing depressive disorders.
Objective: To determine prevalence of depression among pregnant women attending antenatal clinics in Karachi, Pakistan.
Methods: Data was collected in the period of January-March 2017 from 300 pregnant women, by random sampling, during their antenatal visits in Lady Dufferin Hospital & Jinnah Medical College Hospital, Karachi, Pakistan. Standard depression scale i.e. “Hamilton rating scale for depression” was made use of and score more than 7 was taken as depression according to its standard scoring scale. Analysis of the result was done with the help of the SPSS software. Chi-Square test was also applied.
Results: 81% prevalence of depression is among the pregnant women of Karachi. Mild depression is more prevalent (35.7%), then there is moderate (29.0%), severe (11.0%) & least prevalent is very severe form of depression (5.3%). 0.011 was the P value which is statistically significant.
Conclusion: Data indicates a high level of depression in pregnant women of Pakistan, 81%. Depression is more prevalent in women with young age, those who have less number of parity & gravida and the ones that live in a joint family system.
Keywords
Prevalence; Depression; Antenatal period and pregnancy; Mood disorder; Psychiatric disorders
Introduction
Pregnancy and the complications that comes along with it have been a concerning issue of public health around the globe. Pregnancy and then the following transition to motherhood comprises of major psychological and social changes in a woman, which have been linked to symptoms of anxiety as well as depression.
There is quite a hand full of risk factors that predisposes to depression during pregnancy. A few of them are meager antenatal care, poor nourishment, stressful events in life like economic instability, gender based discrimination and violence, previous history of psychiatric disorders, any puerperal complications in the past, incidents during pregnancy like prior miscarriages, and the delivery modes like past instrument facilitated or operative delivery. Other factors include age of the mother, her marital status, gravidity, whether pregnancy was planned or is a result of spontaneous conception, previous history of any stillbirth, previous history of going into prolonged labor, and how well is her level of social support. All of these highlighted points mentioned above predispose a woman to the dark side of antenatal depression [1].
Some of the studies have put forward that pregnant women who suffer from depression have an augmented risk of complicated deliveries or miscarriages; also, it is a documented fact that there is a strong association between antenatal stress and preterm delivery or low birth weight, or at times both [2].
In Pakistan, studies have signposted a high prevalence of depression among women, but all in all there is a dearth of evidence about prevalence of depression during the antenatal period, especially among women who are residing in the remote rural villages of Pakistan. However, there are a few studies that have taken this into regard. According to a research done at the Aga Khan University Hospital, depression that was prevailing among rural pregnant women of Pakistan is as high as 62% [3]. Another study done by Karmaliani et al. [4], conducted in Hyderabad, Pakistan shows 18% of pregnant women were depressed [5].
From studies conducted in recent past it is quite evident that rate of depression in women are much higher during the childbearing years than at any other time in life. There are quite a number of people who are of no clue of the many transitions that occurs in a woman’s body during the entire gestational period. For many past years, authorities mistakenly alleged that pregnancy hormones are the protecting factor against depression, leaving women more susceptible to the illness only after a rise in their hormonal levels once the baby is delivered. They are now of the opinion that the swift increase in hormonal levels at the very start of pregnancy can interrupt brain chemistry and lead to depression.
The rates assessed of depression during pregnancy may vary from 7-15% in economically developed countries to 19-25% in poorer countries. According to the American Congress of Obstetricians and Gynecologists (ACOG), between 14-23% of women will fight with at least some sort of symptoms of depression during pregnancy.
Pariante conducted a research and from that he concluded, evidence that came chiefly from animal and cellular studies, that initiation of the core hormonal stress-response system, the HPA (Hypothalamic-Pituitary-Adrenal) axis, in mothers who are depressed during their pregnancy might affect in a negative way, maternal care as well as offspring's behavior and future psychopathology.
Our study was under taken for its entire period in conjunction with the Jinnah medical college hospital, situated in the Korangi district of Karachi. The core purpose of this study was to determine the existing Prevalence of depression in pregnant women attending antenatal clinics in Karachi. In order to prevent the harmful effects of depression on mother and baby, we should know its prevalence and only then necessary steps can be taken to prevent or decrease its prevalence and effects.
Methods
Sampling
A cross-sectional study was performed. Subjects were pregnant women and the sample size taken was 300. Women picked up for the study was done by the simple random sampling technique, attending Outpatient department of the Jinnah Medical College Hospital and Lady Dufferin Hospital, both in the city of Karachi from January-March, 2017.
Inclusion criteria
Women visiting O.P.D. who were pregnant. Women aged between 17-45 years. Primipara and multi Para both were included
Exclusion criteria
Pregnant women with any other serious medical complications leading to any level of disease related depression.
Instrument
To assess the existence and severity of depression, an eminent screening scale, “Hamilton Rating Scale for Depression”, was used. The scale comprises of all together 17 items, pertaining to mood characteristics, sleep pattern disturbances, somatic symptoms, suicidal propensities, weight loss, genital area symptoms and psychomotor bafflement, experienced during the period of pregnancy. Items scored on a continuum of 0-4, thus allowing total score between 0 to more than 23, where the score between 0 -7, was taken as normal and more than 7 indicates depression. High score indicates greater stress.
Scoring of scale is such: 0-7 Normal, 8-13 Mild, 14-18 Moderate, 19-22 Severe, >23 very severe.
Socio demographic variables were also considered like age of the mother, menarche, parity, family status, and husband’s financial good standing.
Procedure
Women visiting Jinnah Medical College Hospital and Lady Dufferin Hospital were invited to participate during their obstetrics antenatal clinical visits. The study purpose was explained in detail to every participant and each was assured that the information provided by them will be private and confidential. When they agreed to participate, consent was obtained. Approximately 80% of approached women participated.
Women who met the criteria were assigned to the study randomly. The participants were interviewed at the time of their clinical visits. Interview was conducted at medical facility by researchers, which lasted for about a good 10-15 min. Socio demographic variables and details were compiled and then they were screened for depression by using the standard Hamilton Rating Scale, the questionnaire, scale was translated in the local national language and responses were poised during the interview session.
Ethical permission was requested and acquired from both the Hospitals where then the research was taken place. Confidentiality was maintained with no compromise.
In our study the variable that is independent is pregnancy and the dependent variable is depression.
Statistical-analysis
A descriptive analysis of the data was performed using SPSS Software version. Bivariate analysis was done by using chi-square test. P value is 0.011, which is statistically significant.
Results
The data was appropriately analyzed by the help of the SPSS software. Hamilton scale of depression was used to asses’ depression. Individual age of patient, gravida, parity, years since marriage and onset of menarche are presented by mean ± S.D value (Table 1). In view of the Hamilton scale for scoring of depression; Normal (0-7) Mild (8-13) Moderate (14-18) severe (19-22) & very severe (>23). This study was conducted on three hundred patients out of which 57(19%) were found to be perfectly normal 107 (35%), were mildly depressed 87 (29%), were moderately depressed, 33 (11%) were severely depressed and 16 (5.3%) were very severely depressed (Table 2 and Figure 1). Total prevalence of depression was determined. Bivariate analysis between gears of socio demographic details and total score of depression was determined by applying Chi-square test. 0.011 was the P value which first handedly was statistically significant.
| N | Median | Standard deviation | |
|---|---|---|---|
| Age | 300 | 25.00 | 4.385 |
| Gravida | 300 | 2.00 | 1.765 |
| Para | 300 | 1.00 | 1.414 |
| Years since marriage | 300 | 3.000 | 4.0208 |
| Onset of menarche | 300 | 13.00 | 1.120 |
Table 1: Individual age of patient and analysis.
| Frequency | Percentage | Valid % | Cumulative% | |
|---|---|---|---|---|
| Normal 0-7 | 57 | 19.0% | 19.0% | 19.0% |
| Mild 8-14 | 107 | 35.7% | 35.7% | 5470.0% |
| Moderate 15-18 | 87 | 29.0% | 29.0% | 83.7% |
| Severe 19-22 | 33 | 11.0% | 11.0% | 9470.0% |
| Very severe >23 | 16 | 5.3% | 5.3% | 100% |
Table 2: Depression scale score.
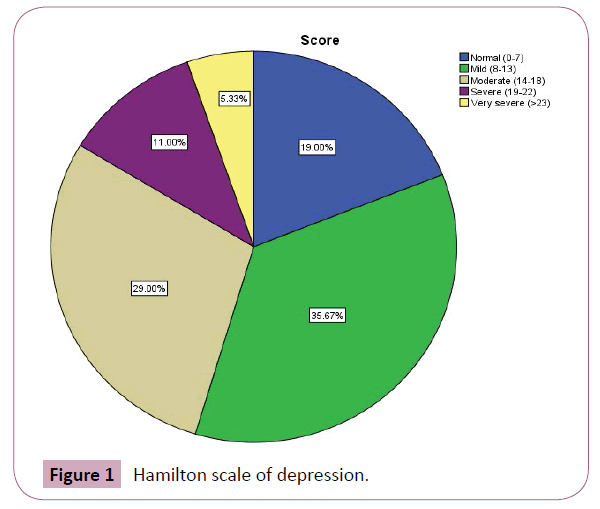
Figure 1: Hamilton scale of depression.
Comparison between the family statuses was done. Depression was found to be more prevalent in the women living in joint family system (Table 3).
| Score | Total | ||||||
|---|---|---|---|---|---|---|---|
| Normal (0-7) | Mild (8-13) | Moderate (14-18) | Severe (19-22) | Very severe (>23) | |||
| Family status | Joint family | 47 | 73 | 54 | 23 | 13 | 210 |
| Nuclear family | 10 | 34 | 33 | 10 | 3 | 90 | |
| Total | 57 | 107 | 87 | 33 | 16 | 300 | |
Table 3: Comparison between the family statuses.
Discussion
Mood disorders are deemed to inordinately affect women across their entire lifespan. In antenatal and postpartum period, they are regular and have weighty implications on the well-being of the women and their children. Such an impact of it is very noteworthy. These consequences can include obstetric and neonatal complications, dwindled mother-infant interactions, and, at the most extreme, maternal suicide and infanticide.
The antenatal period is considered to be one of the most compelling and crucial period for both the expecting mother and the developing fetus for it can have dire side effects. At the time of this period, there is a plethora of physiological and emotional changes in a mother. Hence, it can be stated that depression at the time of pregnancy has very solemn and deleterious side effects on both, the developing fetus and the soon to be mother. It can also very easily be misattributed to the usual physiological variations that do so occur in pregnancy, e.g., troubled sleep and fluctuations in appetite. Depression at the time of pregnancy or can be called antepartum depression, is just as any other clinical depression. It should be handled as nothing different and is as equally important to treat. The aggressive effects of depression on the developing fetus begin quite early in the antenatal period, with intrauterine growth retardation which may continue in the period of postpartum, as the much challenging to handle and manage, failure to thrive. Also, there are many chances of developmental delays, including intellectual infirmity, poor bonding with the mother, and glitches in psychological development of the child. Antenatal depression is not much different from that occurring in any other period. It upsurges the risk of postpartum depression. There are fewer chances of a depressed mother to attend antenatal clinics, and there is an inclination towards substance abuse. Anxiety and depression during pregnancy can be proven hurtful through altered excretion of vasoactive hormones or added neuroendocrine transmitters [6] which in turn may amplify the risk of hypertension. It is quite likely that depression may trigger such vascular changes and in due course induce preeclampsia. However, the clean-cut biochemical mechanism(s) remain largely pseudonymous. Almost 62% of the pregnant women in the rural Sindh in Pakistan are testified to suffer depression [1] compared to 36% of women from southern villages of Pakistan [7]. Also, a research which was completed in Hyderabad showed 18% prevalence of depression. Mumford et al. found a high prevalence (46%) of depression and anxiety among women in neighboring Chitral, Pakistan, where he used Bradford Somatic Inventory [8].
According to this study, depression is prevailing in Karachi and the data shows that it is about 81% by using the standard Hamilton rating scale for depression. Nevertheless, the most prevalent form of depression is Mild depression and the figures show it is about 35.7%.
In this study the enduring predictors of depressed mood in the antenatal period were young age, less number of parity and gravid, number of failed pregnancies, family status, social belongings and social taboos. Rich-Edwards et al. [9] found that young maternal age was the sturdiest predictor of antenatal depression, as it was linked with financial adversity, undesirable pregnancies and absence of partner support [10]. In Pakistan, many women are married off at a very young age, few as young as 16 years old that may clarify the complex prevalence of antenatal depression observed in the current study.
In this study, high pervasiveness of depression is asserted in low to moderate socioeconomic status which implies the importance of screening at antenatal clinics & initial treatment. The increased prevalence of depression during pregnancy in Pakistani women is a matter of public-health concern. Maternal depressive symptoms contribute to disapproving patterns of health care seeking for women and their children [11]. Depression during the antenatal period has a firm affiliation with low birth weight and low nutritional status of the new born. And hence, as a consequence poor outcome of health are witnessed. In Pakistan, social norms, cultural practices and an alliance with in-laws may play a steadfast role in mental health of women. Suicides are not found to be that common during pregnancy [4] but as this study confirms, self-harm feelings are not infrequent in such women, and in particular in those women who acquire depression in its various forms during their pregnancy.
The WHO after much research, has put forth the recommendation that mental health should be integrated into the health policy at basic level of primary health care settings. Although further work is required in the research field to establish usefulness of interventions for depression at community grounds, this study puts forward a crucial step in highlighting the dire need for depression to be screened antenatally [5]. Gestational periods is one of the times in the life of a woman when she has high chances to access the health system by way of antenatal care, and is therefore an ideal time for screening and detection of depression along with further necessary intervening steps to be taken for its cure. Given the high prevalence of antenatal distress, premature detection as well as intervention may have groundbreaking child health implications.
Antenatal depression intensifies the risk of postpartum depression, and both antenatal and postnatal depression has a drastic impact on the health outcomes of the child. Even though maternal mental health is at the moment a squat priority in the health care authorities, ours study goals to highlight this health issue and leave a pilot here to carry on in further researches.
Conclusion
Quite a number of pregnant women battle against depression during their antenatal period. According to this study, prevalence was figured to be 81% with the severity of depression ranging from mild to severe. Depression in its mild form was figured to be the most prevalent. Prevalence is highest in expecting mothers who are young, low parity & gravida and the ones who live in a joint family system with no internal core support.
The results of this study put forward that the prevalence of antenatal depression, that is seen and caught much earlier in its process in antenatal clinics, is merely the tip of the huge unseen and hidden iceberg. Syndromal depression in expecting women is far exceeded by sub threshold depression.
There is quite a possibility that many of the subsyndromal cases become syndromal much later on in the process and hence the need for early detection is quintessential. If the risk factors are taken into consideration, and the suspicion index is relatively high, it would help us enable early detection, and necessary intervention for antenatal depression can be taken.
Limitations
Because we had a grounded, principally middle class low-risk sample, prevalence of depression in the entire period of gestation may be markedly undervalued. Also, our research was mostly conducted on the much urban population and hence it cannot be generalized to the entire nation’s population.