- (2009) Volume 10, Issue 4
Rakesh Kochhar1, Manphool Singhal2, Birinder Nagi1, Anupam Lal2, Usha Dutta1, Kartar Singh1
Departments of 1Gastroenterology and 2Radiodiagnosis, Postgraduate Institute of Medical Education and Research. Chandigarh, India
Received January 8th, 2009 - Accepted May 14th, 2009
Context Anomalous junction of pancreaticobiliary ducts is a condition in which the pancreatic duct and the bile duct join outside the duodenal wall with a long common channel. The most accepted classification of various types of anomalous pancreaticobiliary junction is the new Komi classification. The majority of cases of type III anomalous pancreaticobiliary junction are reported from Japan and very seldom from outside Japan. This study evaluates the prevalence of type III anomalous pancreaticobiliary junction in the Indian population. Objective To retrospectively evaluate the prevalence of type III anomalous pancreaticobiliary junction revealed by endoscopic retrograde cholangiopancreatography (ERCP) examinations carried out between 1985 and 2005. Design ERCP records of 3,827 patients satisfying inclusion criteria between 1985 and 2005 were retrospectively analyzed. Main outcome measure Patients demonstrating anomalous pancreaticobiliary junction were identified and classified according to the new Komi classification. Results A total of 101 patients had anomalous pancreaticobiliary junction (2.6% of all ERCP). Only 2 patients (2.0% of all anomalous pancreaticobiliary junction cases and 0.05% of all ERCP examinations) had type III anomalous pancreaticobiliary junction. Both cases were associated with choledochal cysts and chronic pancreatitis. Conclusion Type III anomalous pancreaticobiliary junction is a rare occurrence in Indian patients as compared to Japanese patients in whom the majority of cases are reported. This demographic variation is still unexplained.
Cholangiopancreatography, Endoscopic Retrograde; Choledochal Cyst; Congenital Abnormalities; Pancreatitis
APBJ: anomalous pancreaticobiliary junction; ERCP: endoscopic retrograde cholangiopancreatography
Anomalous pancreaticobiliary junction (APBJ) is a rare malformation in which the pancreatic duct and bile duct join outside the duodenal wall with a common channel which is longer than 15 mm [1, 2]. Komi [3] has proposed a new classification of APBJ, dividing it into three major types, and presently, this is the most accepted classification. In type I, the common bile duct joins the pancreatic duct at a right angle; in type II, the pancreatic duct joins the common bile duct at an acute angle. Both of these types are subdivided into subtypes “a” or “b”, according to whether the common channel is dilated or not. The normal caliber of the common channel is 3-5 mm. In type III, APBJ union is complicated with a patent accessory pancreatic duct with or without an intricate network of ducts, and is sub classified into types IIIa, IIIb, and IIIc (which is equivalent to Warshaw’s type pancreas divisum with biliary dilatation) [3]. Most cases of APBJ are reported from Asian countries, predominantly from Japan [4, 5, 6]. There are only a few studies on APBJ from India [2, 7, 8] but none of them specifically highlight the prevalence of APBJ, in particular the new Komi type III APBJ. We are among the largest gastroenterology referral centres of the country and have retrospectively analyzed our ERCP data obtained between 1985 and 2005, encountering only two cases of type III APBJ. We report these cases with their ERCP findings. This paper also highlights the rarity of type III APBJ in Indian patients with pancreatico-biliary disorders.
Patients
Retrospective analysis of all ERCP examinations carried out between 1985 and 2005 in our department for various pancreaticobiliary disorders was performed and cases of APBJ were identified and analyzed.
Techniques
All the ERCP examinations were carried out using Olympus sideviewing endoscopes (Olympus Corporation, Tokyo, Japan). Water soluble iodinated contrast was used for opacification of the pancreatic and bile ducts. Three to six spot films were taken for each patient.
Image Analysis
The inclusion criteria were adequate filling of the common bile duct and main pancreatic duct on ERCP, and distinct visualization of the opening of the two ducts separately or by a common channel into the duodenum. All ERCP films were reviewed by a gastrointestinal radiologist. The diagnosis of APBJ was made if the length of the common channel exceeded 15 mm with or without dilation (>5 mm). APBJ was classified according to the new Komi classification [3] and the prevalence of various types was calculated.
ETHICS
Written consent was obtained from each patient who underwent ERCP. The patients were treated according to the ethical guidelines of the "World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects" adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004
STATISTICS
All cases of ERCP fulfilling the inclusion criteria, and where the APBJ was clearly discernable were included for analysis. The percentage of patients demonstrating APBJ was calculated and classified according to the new Komi classification [3]. The percentage of the various types of APBJ was calculated for the purpose of estimating the prevalence of type III APBJ.
RESULTS
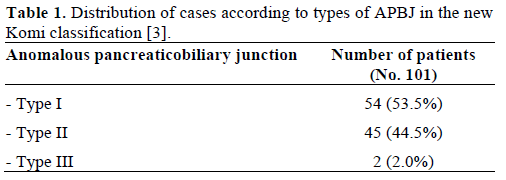
A review of the ERCP records of 3,827 patients yielded a total of 101 patients (2.63%) having APBJ. Of the 101 patients with APBJ, there were 48 males and 53 females, ranging from 3 to 85 years of age. The distribution of the types of APBJ is shown in Table 1.Only 2 patients (2.0% of all APBJ cases and 0.05% of all ERCP examinations) had type III APBJ. The relevant clinical details with detailed ERCP findings of the patients having type III APBJ are herein described.
A 31-year-old man presented having experienced recurrent pain restricted to the upper right quadrant for the past 10 years. He had had six episodes, one every 6-12 months, each lasting 7 to 10 days. He denied having fever or jaundice during the episodes of pain, He had never been examined before presenting at our centre. He had had a similar episode of pain for a week before presenting to our centre. On examination, there was no pallor, icterus or lymphadenopathy. There was no hepatosplenomegaly or lumps in the abdomen. Investigations showed hemoglobin of 11.5 g/dL (reference range: 11-14 g/dL), bilirubin of 0.4 g/dL (reference range: 0-1 g/dL), SGOT of 15 IU/L (reference range: 2-40 IU/L), SGPT of 20 IU/L (reference range: 2-41 IU/L) and alkaline phosphatase of 8 IU/L (reference range: 40-129 IU/L). An ultrasound was carried out which revealed a dilated common bile duct. ERCP through the major papilla with contrast injection demonstrated a ventral duct small in caliber with a long common channel (19 mm in length and 2 mm in diameter). The common bile duct and its intrahepatic right and left branches were also dilated which was diagnostic for a type IVb choledochal cyst (Figure 1). There was no communication with the dorsal duct consistent with complete pancreas divisum. The dorsal duct was the dominant duct with a calculus and prominent side branches consistent with the Cambridge type III changes for chronic pancreatitis. The overall features were consistent with APBJ type IIIa and a cyst excision with hepatico-jejunostomy was carried out. The patient has been regularly followed up for the last 18 years without any new complaints.
A 22-year-old female presented having experienced recurrent episodes of pain in the upper abdomen, radiating to the back, for the past 2 months. She had had multiple episodes of similar pain for the past 3 years. Serum amylase was at borderline levels (96 U/L; reference range: 20-100 U/L), SGOT was 30 IU/L, SGPT was 36 IU/L and alkaline phosphatase was elevated (183 IU/L). MRCP revealed dilated main pancreatic and common bile ducts without any dilation of the intrahepatic biliary channels. ERCP demonstrated complete pancreas divisum with the dorsal duct as the dominant duct. There was a long common channel (24 mm in length and 4 mm in diameter) with the ventral duct. The common bile duct was fusiformly dilated without dilation of the intrahepatic biliary ducts consistent with a type Ic choledochal cyst (Figure 2a). The dorsal duct and its side branches were dilated, consistent with Cambridge type III changes for chronic pancreatitis (Figure 2b). The overall morphology was consistent with APBJ type IIIa. A 5-F plastic pancreatic stent was placed in the dominant duct. The patient is being followed up and surgery is planned.
APBJ is a congenital anomaly in which the main pancreatic and common bile ducts join outside the duodenal wall with a long common channel of more than 15 mm [1, 2]. Choledochal cysts are congenital cystic dilatations of the extrahepatic or intrahepatic bile ducts or both, and have been classified into five types by Todani et al. [9]. According to this classification, type I is a solitary fusiform extrahepatic cyst (further subclassified according to the shape of the affected segment into three types. Type Ia involves cystic dilatation of the common bile duct, type Ib involves focal, segmental dilatation of the common bile duct, and type Ic involves fusiform dilatation of the common bile duct, along with diffuse, cylindric dilatation of the common hepatic duct and common bile duct); type II is an extrahepatic supraduodenal diverticulum; type III is a choledochocele; type IVa are fusiform extra- and intrahepatic cysts; type IVb are multiple extrahepatic cysts, and type V are multiple intrahepatic cysts or Caroli's disease [9].
The association of APBJ with a choledochal cyst may be present in up to 90% of cases [8, 10, 11]. Various causative factors have been postulated for the association of choledochal cysts with APBJ, such as a congenital weakness of the common bile duct and reflux of the pancreatic juices into the bile duct because of high pressure in the pancreatic duct [12, 13]. Hence, this association is more than a chance finding and, once diagnosed, such patients should undergo a definitive surgical procedure to prevent potential complications, such as biliary strictures, cholangitis, and carcinoma of biliary tract, gall bladder and pancreas [1, 2, 7, 8, 14, 15].
Most of the cases of APBJ have been reported from Asian countries, predominantly from Japan [4, 5, 6]. Misra et al. and Nagi et al. from India have described APBJ and related disorders [2, 7, 8], but the prevalence of the various types of APBJ has never been reported from anywhere outside Japan. In their series, Komi et al. from Japan reported type I APBJ in 35.3%, type II in 21.6% and type III in 43.1% of cases [4]. Similar results were reported by Li et al. from Japan where the prevalence of type III APBJ was 41.5% [6].
The present study revealed only 2 cases of type III APBJ; i.e., 2.0% of all APBJ cases and 0.05% of all the ERCP examinations performed over two decades in our institution, a referral centre of North India. This analysis highlights the low prevalence of type III APBJ in symptomatic Indian patients with pancreaticobiliary disorders
Both of our cases showed the clinical and radiological features of chronic pancreatitis, choledochal cysts, long common channel and complete pancreas divisum consistent with the new Komi type IIIa APBJ. The chronic pancreatitis seen in our patients can be attributed to pancreas divisum and APBJ as both of these conditions are known to be associated with an obstructed flow of pancreatic secretions [4, 7, 16, 17]. Pancreatic duct calculi are only rarely encountered in APBJ and choledochal cysts [18, 19], and these are seen predominantly in adults [12]. However, subtype IIIc3 APBJ has been reported to be associated with ductal calculi in up to 43.8% of cases [4]. The proposed pathogenesis of pancreatic ductal calculi is protein plug formation and mucin overproduction [4, 20]. Whether the presence of pancreatic calculi makes a patient with APBJ symptomatic or not is controversial as only a few reports suggest that their presence results in symptoms [13, 20].
The classification of APBJ is important for management as types Ib, IIb, IIIc3 are associated with a dilated common channel (greater than 5 mm) and are frequently complicated by chronic relapsing pancreatitis due to the formation of a protein plug or pancreatic calculi [4]. For type IIIc3, a pyloruspreserving pancreatoduodenectomy is the surgical procedure of choice while, for type Ib and type IIb, a papilloplasty can be carried out if stenosis of the papilla is present [4]. For choledochal cysts, cyst excision with bilioenteric anastomosis should be carried out [9, 13, 21].
In conclusion, in this first report outside Japan, the prevalence of type III APBJ was only 2.0%. We encountered two such cases over two decades in a referral hospital of Northern India. A multicentric study to explore the incidence of APBJ in the general population using non-invasive radiological investigations, such as ultrasound, multidetector computed tomography or magnetic resonance cholangiopancreatography should be carried out to get a better perspective of APBJ and related disorders
The authors have no potential conflict of interest