Case Report - (2016) Volume 17, Issue 4
Ram Nawal Rao1, Ranjana Ranade1, Praveer Rai2
Department of 1Pathology, 2Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, UP, India
Received January 18th, 2016 - Accepted March 30th, 2016
Context Primary myxofibrosarcoma of the pancreas is a very rare entity. Case Report Myxofibrosarcoma is a rare tumour of mesenchymal origin, composed of malignant fibrocytes in a myxoid matrix. Previously it was known as myxoid malignant fibrous histiocytoma. It usually involves the extremities, followed by trunk, retroperitoneum, mediastinum and head. Based on the degree of cellularity, pleomorphism and mitosis these lesions vary from low-grade to high grade. They have high rate of recurrence but metastasis is very uncommon. Cellblock and histopathology showed a characteristic distinct curvilinear vascular patterns. Conclusion Myxofibrosarcoma is uncommon neoplasm presenting as mucinous cystic mass, possibility of myxofibrosarcoma may be considered on cytology if the smears revealed occasional spindle cells, abundant mucinous and myxoid material in background.
Immunohistochemistry; Pancreatic Cyst
EUS-FNA endoscopic ultrasound-guided fine needle aspiration
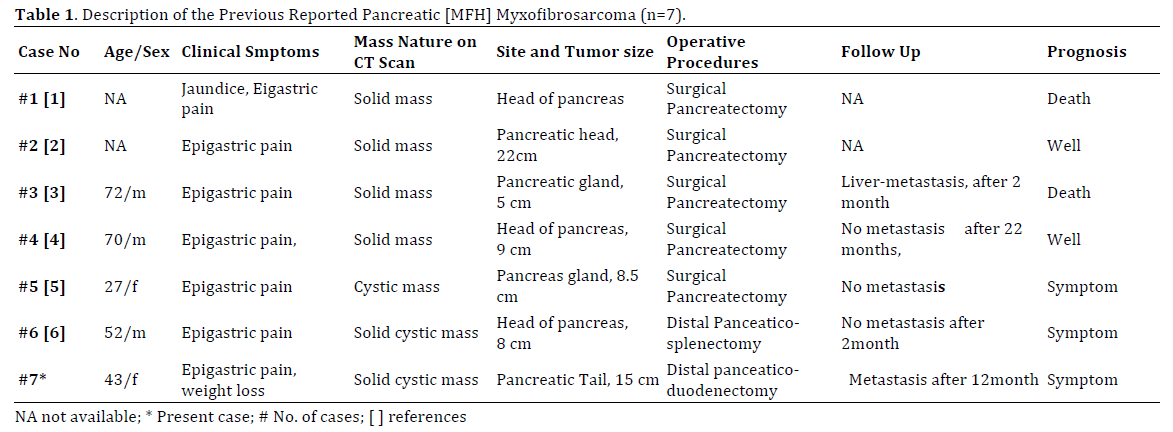
Myxofibrosarcoma of the pancreas is an uncommon neoplasm. Primary myxofibrosarcoma of the visceral organs like the lung, genitourinary tract, and cardiovascular system has also been described. To our best of knowledge, this patient is 7th case report of myxofibrosarcoma of pancreatic tail described in world literature till date (Table 1, cases #1-7). Based on the degree of cellularity, pleomorphism and mitosis these lesions vary from low-grade to high grade. Cellblocks and histopathologically a distinct curvilinear vascular patterns are seen. These neoplasms mainly affect patients in the sixth to eighth decades of life and the overall 5-year survival rate is 60–70%. Herein, we describe a first patient with myxofibrosarcoma of the pancreas reported by EUS guided fine needle aspiration cytology and immunocytochemical findings on cellblock with correlation of clinical, radiological, histopathology and immunohistochemistry findings.
A forty-three-old-year female presented with pain in left upper abdomen x 6 months, gradually progressive, radiating to back, relieved after antalgic therapy. She had history of dyspepsia, post prandial fullness, loss of appetite and loss of weight (7 kg in 6 months). No history of fever, vomiting, jaundice, upper and lower gastrointestinal bleeding. No other bowel or bladder complaints were seen. On objective perabdominal examination there was a visible lump in left upper quadrant (left hypochondrium,epigastrium, lumbar, umbilical approximately measuring 15x13x12 cm). She had also history of underwent 4 times lumpectomy for breast lump diagnosed as Phyllodes Tumor with negative lymphnode 2 year ago from the pancreatic lump. Patient had also history of Laproscopic tubectomy 16 years ago. Pancreatic fluid amylase was 93 IU/ml (normal 25-100 IU/ mL) and CA 19-9 is 13.29 (normal 0-37 U/mL).
Radiological Examination
Ultrasound examination showed a large (15x13x12 cm) irregular lobulated solid-cystic lesion abutting or displacing pancreatic tail, pushing stomach, spleen & left kidney. Rest was normal. Contrast Enhanced computed tomography (CECT) showed large approximately 15x13x12cm lobulated hypodense peripherally enhancing cystic mass lesion in region pancreatic tail and distal body. Mass was displacing stomach medially and visceral surface of spleen, splenic flexure of colon and anterior surface of left kidney. Lesion was abutting splenic vessels with loss of intervening fat planes. Another small (1.5x1.4 cm) hypodense lesion in uncinate process of pancreas was also seen. A clinical diagnosis of cystic tumour of head and tail of pancreas (mucinous cystadenoma) was made. Endoscopic (EUS) ultrasound showed a large cystic lesion in pancreatic body & tail with some solid component (Figure 1).
Cytological Examination
EUS-guided FNA from pancreatic mass was done after examination of pancreatic mass on EUS ultrasound and CECT. Smears and cellblocks were made from the aspirated material. Smears are paucicellular showed few dispersed lymphocytes, histioctyes and some elongated to spindle cells with condensed chromatin and moderate cytoplasm on a background of abundant mucinous and myxoid material admixed with hemorrhage (Figures 2, 3). Cytological diagnosis of mesenchymal neoplasm of pancreas -body and tail of pancreas was made. Sections from cellblock of pancreatic mass showed a mesenchymal neoplasm composed of sheets of spindle shaped cells with oval to elongated, mild to moderately pleomorphic nuclei with coarse chromatin, small conspicuous nucleoli at places and moderate amount of pale cytoplasm. Interveining stroma shows extensive myxoid change and curvilinear vessels (Figure 4). Necrosis is present. Few mitotic figures are also seen. Periodic acid schiff-Alcian blue stain (PAS after diastase-alcian blue stain- PAD-AB) was done on cellblock section that was negative for cytoplasmic mucin in tumor cells. FNA cytology from recurrent breast lumps were also done and smears showed features of phylloides tumor two year ago.
Immunohistochemistry
Three to five micron sections were cut from paraffin blocks made from tumor and were fixed on 10% poly-L-lysine coated slides, dewaxed in xylene and rehydrated in graded alcohol. Antigen retrieval was done by microwave method in which slides were placed in three cycles of 10 minutes each in 10 mmol citrate buffer p 6.2. Slides washed in TRIS buffer with Peroxidase block. Sections were incubated with the primary antibody at 1: 50 for Vimentin and CD34 at room temperature at 25°C for 3 hours. Sections were placed in chromogen diamnobenzidine (Dako Corporation Denmark) for few seconds. Counter staining was done by Mayer’s hematoxylin and slides were mounted in DPX.The immunocytochemistry was performed on cellblock and showed strong diffuse cytoplasmic positivity for Vimentin and focal Smooth Muscle Actin (SMA) (Figures 5, 6). CD34 show weak focal positivity. Desmin, CD117, CD10, S-100 and Cytokeratin were negative (Figures 7). Ki -67 was 2-4%. A confirmed diagnosis of low grade myxofibrosarcoma of pancreas was made due to strong positivity of Vimentin, focal SMA and weak CD34.
Macroscopic Examination
Distal pancreaticosplenectomy was done and showed a specimen conglomerate composed of distal pancreatectomy with splenectomy with attached part of stomach and part of intestine. Pancreas along with tumor measured 26×18×14 cm, stomach measured 20×10 cm, colon measured 5 cm in length. Cut surface of the tumor (15×13×12 cm) showed greyish solid and mucinous areas (Figure 8). Tumor was easily seperable from the spleen. Other pancreaticoduodenectomy composed of pancreaticoduodenectomy specimen comprising of duodenum measuring 22 cm in length, pancreas measuring 5×5×4 cm along with gall bladder measured 6cm in length was performed. Cut surface of pancreas showed another small mucinous neoplasm measuring 1.5×1.4 cm (Figure 9). Cut surface of intestine was unremarkable. Cut surface of gall bladder showed atrophic mucosa, wall thickness measured 0.2-0.3 cm. Two lymphnode with common hepatic artery each measuring 1×1 cm in size. After one year, she developed another globular chest wall mass measuring 1×1×0.8 cm seen. External surface was fatty with homogenous and whitish on cut surface.
Histopathological Examination
Sections from pancreatic mass show a neoplasm composed of oval to stellate shaped cells arranged in fascicles interspersed by a curvilinear array of blood vessels in a background of myxoid connective tissue stroma with attached normal pancreas at periphery (Figures 10, 11). Areas of necrosis and few mitotic figures are also seen. Sections from stomach, intestine, spleen and gall bladder are free of tumor infiltration. Sections from proximal and distal resection margin of intestine are also free of tumor infiltraion. Sections from both the common hepatic artery lymphnodes are free of tumor metastasis.
Sections from a globular mass from chest wall shows a mesenchymal neoplasm composed of spindle shaped cells with oval to elonagted mild to moderately pleomoprhic nuclei with coarse chromatin, small conspicuous nucleoli at places and moderate amouont of pale cytoplasm. Interveining stroma show abundant myxoid change and characteristic curvilinear vessels. Necrosis was absent. Occasional mitotic figures are seen. The immunohistochemistry on resected pancreatic mass and chest wall also done and showed strong diffuse cytoplasmic positivity for Vimentin and focal Smooth Muscle Actin. CD34 showed weak focal positivity. Desmin, CD10, S-100 and Cytokeratin are negative. Ki-67 proliferating index was 2-4%. A confirmed diagnosis of myxofibrosarcoma-pancreas and metastasis to chest wall was made.
Primary myxofibrosarcoma of the pancreas is an extremely rare tumour composed of malignant fibrocytes in abundand myxoid matrix [1- 6]. Primary sarcomas of the pancreas are rare and represent less than 1% [7]. Main clinical symptoms was epigastric pain in all 7cases including our case (Table 1). Jaundice was seen in 1/7cases (case #1). Weight loss and loss of appetite were not seen in all cases excluding our case (case 7#). All the previous reported cases were diagnosed on histopathology sections while our case on Cellblock sections from EUS FNA of pancreatic mass. Radologically, all the cases revealed solid cystic mass except one revealed cystic mass (case #5).
In our case, EUS ultrasound and CT scan revealed a solid cystic mass involving the body and tail of the pancreas. The patient underwent EUS guided FNA cytology, Distal pancreaticosplenectomy and pancreaticoduodenectomy. After one year, patient developed metastasis to right chest wall. Five out of 6 earlier reported cases were diagnosed as malignant fibrous histiocytoma except first case (myxofibrosarcoma or malignant fibrous histiocytoma) on histopathology while our case diagnosed on EUS-FNA cytology as Myxofibrosarcoma.
Based on cytology smears findings, cellblock and immunocytochemistry, the tumor was characteriszed as myxofibrosarcoma of pancreas. Till date, this is the first case of myxofibrosarcoma of pancreas have been reported by Endoscopic ultrasound guided fine needle aspiration cytology in the world literature. Cellblock revealed a crucial role for the confirmative diagnosis of myxofibrosarcoma due to strong immunocytochemical staining positivity for Vimentin and focal SMA. Ki-67 index was 2 to 4% in our case but it was 20-30% in tumor cells with mitotic count 4-5/10hpf in case #6.
Mucinous cystic neoplasm are most closed differential diagnosis due to presence of abundant mucinous and myxoid material in the cytology smears and it should be ruled out by Cytokeratin immunostaining positivity on the section of cellblock but cytokeratin was negative in our case. Other closed differential diagnosis of myxofibrosarcoma which have spindle cells morphology with myxoid changes and immunocytochemical findings are described in Table 2. Liver metastasis was seen in one out of six previous reported cases as in our case seen as right chest wall metastasis (cases #3 & #7).

After distal pancreaticosplenectomy and pancreaticoduodenectomy, patient developed derrangement of sugar levels(persistant hyperglycemia), advised Insulin infusion and sugar monitoring. After 1 year of follow up, patient developed metastasis to right chest wall without any lymph node involvement or significant adhesion to retroperitoneum.
Myxofibrosarcoma is very rare neoplasm mainly affect patients in the sixth to eighth decades of life and presenting as mucinous cystic mass, possibility of myxofibrosarcoma may be considered on cytology if the smears revealed abundant mucinous and myxoid material in background.
Conflict of Interests
Authors declare no conflict of interests for this article.