Letter to Editor - (2017) Volume 18, Issue 1
Maurizio Zizzo1, Carolina Castro Ruiz1, Lara Ugoletti1, Stefano Bonacini1, Alessandro Giunta1, Riccardo Valli2, Giuliana Sereni3, Antonio Manenti4, Claudio Pedrazzoli1
1Department of General Surgery, C.S. Surgical Oncology and Reconstructive Surgery,
2Department of Oncology and Advanced Technologies, C.S. Pathology,
3Department of Oncology and Advanced Technologies, C.S. Gastroenterology - Digestive Endoscopy, Azienda Ospedaliera – IRCCS Arcispedale Santa Maria Nuova, Avenue Risorgimento 80, 42123 Reggio Emilia, Italy and
3Department of General Surgery, Azienda Ospedaliero-Universitaria – Policlinico, Del Pozzo Street 71, 41124 Modena, Italy
Received October 07th, 2016 - Accepted November 11th, 2016
Follow-Up Studies; Pancreas; Perivascular Epithelioid Cell Neoplasms; surgery
CT computed tomography; EUS endoscopic ultrasound; EUS-FNAB endoscopic ultrasound-guided fine needle aspiration biopsy; HPF high-power field; PEC perivascular epithelioid cell; US ultrasound
We have recently read with great interest two articles published in your Journal years ago, by Baez et al and Zemet et al, both concerning the primary pancreatic PEComa, an extremely rare mesenchymal tumor composed of histologically and immunohistochemically distinctive perivascular epithelioid cells [1, 2]. In recent years similar cases (for a total of fifteen) have been published in the international literature, from the first case described by Zamboni et al. [3, 4]. All cases were treated by surgery, a therapeutic choice from which our working group has diverged on the basis of some important considerations.
We present the case of a 68-year-old man who came to our attention complaining of occasional episodes of mild upper abdominal pain. Physical examination was negative and the laboratory tests did not show any alteration, including tumor markers. The imaging (US and CT) showed an hypervascular, well-demarcated lesion of the pancreatic head with a maximum diameter of 28 mm and no relation with neighboring organs (Figure 1). Nothing to the other abdominal viscera. The cytological and immunohistochemical examination of the samples obtained by EUS-FNA (Figure 2), showed the typical features of PEComa in the absence of malignancy features. The cytological material consisted of multiple aggregates of large epithelioid cells, with oligomorphic nuclei and eosinophilic nucleoli. No mitosis could be found. The cytological background was devoid of necrotic debris or inflammation. In order to characterize the lesion, immuncytochemical stains were performed on a formalin-fixed clot obtained during the fine needle aspiration procedure (Figure 3a-d). The epithelioid cells were positive for HMB45 (clone HMB45, Roche), MART1/Melan A (clone A103, Roche) and Smooth Muscle Actin (clone 1A4, Roche); whereas they were negative for Pancytokeratin (clone AE1+AE3+PCK26, Roche), S100 (clone 4C4.9, Roche) and Synaptophysin (clone MRQ40, Roche).
Figure 3. Immunochemistry: (a). high power view of the epithelioid neoplastic cells (formalin-fixed and paraffin embedded clot, Hematoxylin-Eosin stain, 40X); (b). neoplastic cells show intense immunoreactivity for MART1/Melan A (Hematoxylin counterstain, 40X); (c). high power view of immunocytochemical stain for HMB45 (Hematoxylin counterstain, 40X); (d). strong immunoreactivity for Smooth Muscle Actin (Hematoxylin counterstain, 40X).
Given the extreme rarity of the disease, after several multidisciplinary assessments of the case and in collaboration with the National Network for Rare Diseases, we decided to perform a close clinical and instrumental follow-up on the basis of the absence of clear signs of uncertain potential or certain malignancy (Folpe's criteria) [5]. In the 13 months following the diagnosis the patient experienced only a couple of episodes of abdominal pain and the lesion remained stable in size.
Primary pancreatic PEComa is usually benign but few cases have been reported of uncertain malignant potential or certain malignant nature, on the basis of the classification proposed by Folpe et al. (Table 1) [5]. This classification indicates as “worrisome features” a lesion bigger than 5 cm, the presence of an infiltrative growth pattern, a high nuclear grade and cellularity, a mitotic rate > 1/50 HPF, the presence of necrosis and vascular invasion [5]. The authors developed this classification studying soft tissue and gynecologic PEComas, identifying the variables that appeared closely related with subsequent aggressive behavior of the lesion, increasing the risk of recurrences and metastases [5]. Up to date this classification is considered the main reference, although we can not confirm the accuracy of its criteria because of the extreme rarity of the disease. Nevertheless, all cases thus far described, diagnosed preoperatively by EUS-FNA and classified as benign, have been treated with surgery, except ours [4].
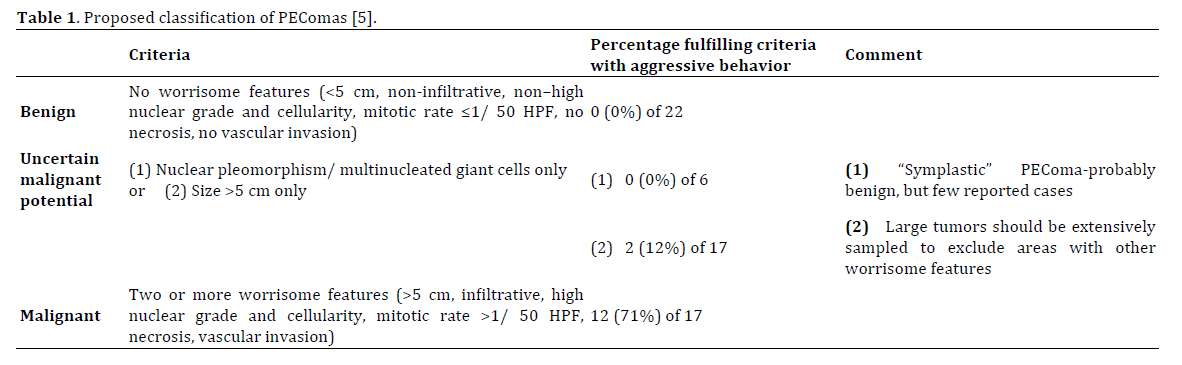
We believe that surgery is not always the correct treatment choice in a patient with primary pancreatic PEComa, especially if the EUS-FNA is clearly diagnostic, if the lesion is classified as benign, therefore lacks the “worrisome features” described by Folpe et al. and if the patient is in good general clinical condition and lacks symptoms and radiological signs suggestive of invasion or mass effect on neighboring organs. Especially given the considerable morbidity and mortality associated with pancreatoduodenectomy, the strong impact on quality of life that pancreatic surgery could have and an old patient, as in our case. Therefore, in such cases we suggest as follow-up the execution of physical examination, EUS-FNA and abdomen CT scan once every 12 months, on the basis of Folpe's criteria. EUS-FNA is of considerable importance in determining the cytological aspects of the lesion such as: nuclear grade, cellularity, mitotic rate and necrosis; furthermore, EUS itself gives us information regarding the size of the lesion, the relationship between the lesion and the main ducts (main pancreatic duct and common bile duct), and between the lesion and the neighboring organs. Abdomen CT scan, on the other hand, is essential to evaluate the morphological aspects of Folpe's criteria: size of the lesion, infiltrative growth pattern and vascular invasion, as well as the appearance of metastases. Only in the case of changes in the clinical presentation (eg. persistent or severe abdominal pain, jaundice) or the unveiling of features that reclassify the lesion among uncertain malignant potential or as a malignant lesion, the surgical treatment should be considered.
What we presented is the first case of primary pancreatic PEComa not submitted to surgery but follow-up alone. However, further studies on large series are needed to better understand the biological features of PEComa in order to be able to reach guidelines for diagnosis, treatment and follow-up, which today appears to be extremely difficult because of the rarity of this tumor.
The authors declare that they have no conflict of interest.