Case Report - (2017) Volume 3, Issue 4
Metehan Yildirim1, Gülfizar Sözeri-Varma1*, ncel2, Ibrahim endur1 and Osman Özdel1
1Department of Psychiatry, Pamukkale University, Denizli, Turkey
2Department of Neurology, Pamukkale University, Denizli, Turkey
*Corresponding Author:
Gülfizar Sözeri-Varma
Associate Professor
Faculty of Medicine
Department of Psychiatry
Pamukkale Univercity, Turkey
Tel: +902582699000/4508
E-mail: gvarma@pau.edu.tr
Received Date: May 17, 2017; Accepted Date: June 14, 2017; Published Date: June 20, 2017
Citation: Yildirim M, Varma GS, Öncel C, endur I, Özdel O (2017) Primer Progressive Aphasia with Psychiatric Symptoms. Acta Psychopathol 3:36. doi: 10.4172/2469-6676.100108
Primary Progressive Aphasia (PPA) is a rare neurodegenerative disease that is rarely observed with the relative preservation of mental functions such as memory, visuospatial functions, personal characteristics but that causes degeneration of speech function. Even though cognitive and behavioral functions are preserved during the starting stages, psychiatric symptoms may develop with the advancement of the disease. The objective of this study was to present a primary progressive aphasia case followed due to conversion disorder and depression for about 30 years and to discuss the confounding effects of the existing psychiatric symptoms at the diagnosis stage.
Keywords
Aphasia; Primer Progressive Aphasia (PPA); Depression; Conversion disorder
Introduction
Primary Progressive Aphasia (PPA) is a neurodegenerative disease that causes progressive disorder of neural functions related with speech [1]. It is classified as part of Frontotemporal Lobar Degeneration (FTLD) group. FTLD has been defined for all neurodegenerative diseases due to focal atrophies in the frontal and/or temporal regions encompassing different clinical appearances such as PPA, frontal lobe dementia, Pick disease and PPA-amyotrophic lateral sclerosis, cortico basal degeneration etc. [2]. PPA starts mostly at ages around 50 and is more frequently observed in men. The primary term in PPA puts forth that the disease first affects the speech functions, whereas the term progressive indicates that the disease is progressive and degenerative and aphasia indicates that there is a speech problem [3].
Slow progressive aphasia syndrome without dementia was first defined in 1892 by Pick. Pick first stated a case with severe speech functions while he was alive and defined it as “isolated and progressive disorder in speech functions”. Six cases were defined 90 years afterwards in 1982 by M. Mesulam without dementia symptoms but with slow progressive aphasia symptoms which resulted in an increase in the interest towards this syndrome [3]. PPA is characterized by a progressive deterioration in speech functions (word use and comprehension) for at least 2 years. In addition, it is observed that other cognitive functions such as memory, visual-spatial functions, abstraction, judgment and personal characteristics are relatively preserved. However, deterioration in other cognitive functions may also occur in later years. Frequently, there is focal atrophy in the left temporo-polar region and two thirds posterior of the frontal lobe [4,5].
Psychiatric and behavioral problems such as anxiety, irritability, aggression, disinhibition, depressive and psychotic symptoms may arise in PPA due to frontotemporal network damage [6,7]. In this study, a case was presented that has been undergoing psychiatric treatment for 30 years due to conversion disorder and depression, defined by the relatives as “forgetfulness” which develops as problems in understanding and explaining words. The objective with this case presentation was to attract attention to and discuss the difficulties in diagnosis and definitive diagnosis due to the existing psychiatric symptoms.
Case Presentation
A 62 year old female applied to our polyclinic with complaints of continuous crying, not leaving the house, irritability and forgetfulness. The patient was a primary school alumni housewife and was living with her spouse. It was determined according to the information obtained from her and her spouse that: the patient has frequent pains in the head, neck and arms, has been going to physical treatment and rehabilitation experts and that they were told the pains could be psychological. It was also learned that the first psychiatric application of the patient took place 30 years ago with irritability, crying fits and fainting; that she has made many psychiatric applications until today, used many drugs the names of which were not remembered, that she has had partial relief from the medications but that the medications were not used regularly. It was learned that the patient has been experiencing problems in understanding and naming words since 3 years and that she cannot complete the sentences (e.g. she was using expressions such as “would you eat water?” instead of “would you drink water?”). The patient made various applications to neurology departments of different hospitals during this period. Memantin and donepezil was started with Alzheimer’s disease diagnosis but there was no amelioration. The patient applied to many psychiatrists during the same period; medications such as duloksetin 60 mg/g, mirtazapin 15 mg/g, venlafaksin 37.5 mg/g, trazodon 50 mg/g were suggested with depression diagnosis and the medications were used irregularly. She applied to our polyclinic with increasing body pains and crying. The patient was able to carry out her daily works and personal care (she could carry out daily chores in the house such as cooking, cleaning and she was also able to cater her own toilet-shower needs). It was learned that the patient had problems with her brother as psychosocial stressor, that they were not in touch for 3-4 years and that the patient was very sad about this. There was no alcohol and substance use. There was Alzheimer’s disease diagnosis and treatment case in her aunt and 2nd degree relatives in her family history. The premorbid personal characteristics were defined as meticulous, scrupulous and tense.
During the psychiatric examination
Her general appearance was one that reflects her age, with sufficient self-care and an apathic appearance; she continuously cried during the interview, her general attitude during the interview was discordant; she had difficulties in understanding the questions and did not give proper answers to the questions. Her speaking speed had increased slightly, however she was not able to form comprehensible sentences; the speech was tangential and perseverative. She was saying in a perseverative manner that she went on pilgrimage 3 years ago and that she was better before that and that she did not feel good now but she was unable to tell what kind of a problem she was experiencing. Her affectivity was depressive but superficial. Immediate memory was normal (3/3), remembering was defective (0/3). Perception was ordinary. Associations were dispersed during her process of thinking, there was no psychotic content in the content of her thoughts, and there were passive thoughts of death. There were frequent somatic complaints (neck ache, arm ache…); all the attention of the patient was focused on her body and physical pains. The amount of sleep had decreased, whereas the appetite was normal. There was social withdrawal and conversive fainting in her story.
The patient was hospitalized in the psychiatric department with depression, conversion disorder and dementia process prediagnoses in order to re-examine the diagnosis and regulate the medical treatment (Figure 1).
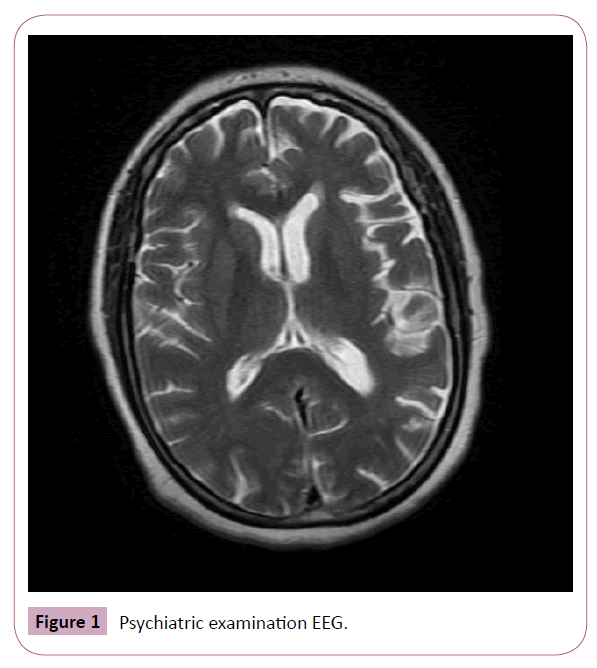
Figure 1: Psychiatric examination EEG.
Routine laboratory findings: Normal.
Standardized mini mental test score: 12/30.
Brain MRG: Focal atrophy was determined in left temporal region.
EEG: Was evaluated as normal.
Neuropsychological evaluation
It was observed during the test that the individual gives improper responses to the questions. It also attracted our attention that the individual could not cooperate with the test due to frequent somatic complaints. Severe deterioration was observed in the number sequences sub-test for attention in neuropsychological tests. A test performance indicating advanced deterioration was obtained in all sections of the verbal memory test. She was able to identify only 3 out of 10 words during the recall stage. She could not take the abstraction test. Advanced level of organicity findings were attained in accordance with Marley’s criteria in the Bender- Gestalt test. She was able to draw only 1 out of 9 figures during the recall stage. The drawing errors led us to think that her planning capacity decreased, attention and concentration weakened, that she was experiencing difficulty in remembering, that she had a tendency for chronicity of perseverative behaviors and that she experienced difficulties in abstract thinking, disengage from tasks-duties, conflicting ideas as well as difficulties in the capacity for learning new things. She was successful in cube drawing test towards visual structuring skill from among the frontal function tests, however advanced deterioration was observed in the clock-drawing test for planning skill and category formation test.
Process
Consultation was requested from the physical treatment and rehabilitation treatment for the physical pains of the patient and pain killer treatment was applied in accordance with their suggestions. Consultation was requested from the neurology department. No pathology was determined other than nonfluent aphasia as a result of the neurological examination. Primary progressive aphasia was considered. Gülhane Aphasia Test was applied, the patient received a score of 45/83 (errors were in awareness, understanding and executing commands sections). The treatment of the patient was organized as sertralin 50 mg/g, mirtazapin 15 mg/g. Crying fits and somatic complaints of the patient decreased over time, social communication slightly increased, sleep pattern got better. She was discharged from the hospital with suggestions to be followed up closely by the neurology and psychiatry polyclinics as well as with suggestions to continue the treatment.
Discussion and Conclusion
This patient had been followed up from time to time by psychiatrists for 30 years with depression and conversion disorder diagnoses. The patient was aware that things were not going well during the past 3 years; however she could not express it sufficiently well. Upon close examination of the patient’s story, it was understood that what the patient relatives named as forgetfulness was actually deterioration in the areas of finding words, naming and understanding. It was determined as a result of the interviews after the crying fits of the patient decreased that she could not understand the words and sentences in speech, that she responded with irrelevant things because she could not understand the questions and that her own sentences contained uncertainties. The fact that the somatic complaints of the patient increased during this period could be a reflection of her difficulty in verbal expression.
Fronto-temporal Lober Degeneration (FTLD) may come up with different clinical appearances in relation with the underlying neuropathological processes. This results in contradictions in terms in this field. The three clinical prototypes of FTLD are: Frontotemporal Dementia (FTD), progressive nonfluent aphasia (PA) and Primary Progressive Aphasia (PPA, semantic dementia) [8]. Case presentations and studies on PPA contributed to a better understanding of the clinical picture. The diagnoses criteria defined by Mesulam et al. in 2001 have been given in Table 1; the PPA diagnosis criteria defined by the study group in this field during the international frontotemporal dementia congress in 2006 have been given in Table 2 [1,3,9]. The facts that there are deteriorations in understanding words, finding words and forming sentences for 3 years, that this has been progressing slowly, that the patient can continue her daily functionality and that there is no pathology in the brain scan other than the single side left temporal atrophy support the PPA diagnosis. The psychiatric symptoms and psychiatric treatment story of this patient were factors that made it difficult to find the exact diagnosis and to understand the current clinical state.
| S. No. | PPA diagnosis criteria |
|---|---|
| 1 | Intermittent and progressive disorder in finding words and naming objects, difficulties in understanding the words that emerge spontaneously during speech or during neuropsychological tests |
| 2 | Limitations in Daily life activities due to deterioration in speech functions for at least 2 years |
| 3 | Normal premorbid speech functions |
| 4 | Having no apathy, disinhibition, forgetfulness, visual-spatial disorder, visual recognition disorder or sensory motor function disorder during the first 2 years |
| 5 | Rarely acalculia and ideomotor apraxia |
| 6 | Distinctive deterioration in speech functions after 2 years followed by deterioration in mental functions |
| 7 | Ruling out reasons such as stroke and tumor via imaging methods |
Table 1: PPA Diagnosis criteria [4].
| S. No. | PPA diagnosis criteria |
|---|---|
| 1 | Having one or more of the speech disorders listed below: Difficulty in finding words not related with dysarthria; Difficulty in naming objects; Weak syntax in speech and writing; Erroneous spelling; and Difficulty in understanding words |
| 2 | Slow progression |
| 3 | Preservation of identifying familiar faces and objects in the 2 year recent past in addition to behavioral and fundamental personality. |
| 4 | Having no lesion in imaging that might explain speech deterioration. |
Table 2: PPA diagnosis criteria during international front temporal dementia congress.
Deterioration in speech functions may also be observed in Alzheimer’s disease, corticobasal degeneration, frontotemporal dementia and motor neuron disorders. However, other cognitive disorders are incorporated in the clinical picture in a very short amount of time in such cases. The fact that deteriorations were existent in only the speech functions for 2 years was an important indicator. Attention in neuropsychological tests was observed in our case in addition to distinctive deteriorations in majority of all processes of memory (recording recall, storage), abstraction and frontal function tests. However, the patient should understand what is told and should be able to understand the directions well in order to evaluate these tests correctly. Indeed, the patient could not cooperate in the tests which prevented the correct measurement of the test performances. It was observed as a result of the Gülhane Aphasia Test of the patient that she experienced difficulties in understanding and carrying out the commands. Carrying out specific tests towards understanding the problems in speech may be more helpful in diagnosis instead of general neuropsychological tests. Cognitive disorders should be followed up for this patient.
Today, there is no known treatment for PPA. There are limited numbers of studies on acetylcholine esterase inhibitors and Memantin which are also used in Alzheimer’s disease and they have limited effectiveness. Treatment is based on drug treatment, speech rehabilitation and strategies for developing communication as well as providing support to the patient and the caregivers [10]. Indeed, our patient used acetylcholine esterase inhibitors but experienced no progress. It has been put forth as a result of the case presentations in recent years that TMS is partially useful in PPA cases [11,12]. Controlled studies that will be carried out in this area will put forth the effectiveness of TMS better.
PPA is a rare disease that starts in the ages of 50’s which is 40% based on a positive familial history. Deterioration in our case started towards the late 50’s. There is AH story in the family. However, a similar clinical picture is defined and it might be a case with familial characteristics. PPA patients may lead very active and productive lives since they are perfectly normal in all other mental functions despite difficulties in speech. There are many patients who continue their artistic skills by painting, working on handcrafts, travelling or leading their social lives [3]. Our case is followed up with an increase in functionality following the betterment of psychiatric symptoms.
Psychiatric disorder story and existing psychiatric symptoms might make it difficult to define the symptoms that emerge in the cognitive area and to manage them properly. In this case, the problems experienced by the patient could be better understood after the psychiatric symptoms were controlled. A multidisciplinary approach involving a common study by neurology and psychiatry might be helpful in similar cases.