What is known on this subject
• Women from ethnically diverse groups living in deprived localities in theUKmay be at greater risk of poor
mental health, particularly at the postpartum stage.
• Exercise may enhance mental health and ameliorate mental illness at the postpartum stage, but there is
insufficient information about its effects on a variety of postpartum mental health problems across
cultures.
• Members of ethnically diverse groups engage in lower levels of physical activity.
• Research on exercise rarely reports outcomes for ethnically diverse women, or their views on how exercise
interventions should be delivered to promote their mental health postpartum.
What this paper adds
• Postpartum women in ethnically diverse priority groups believe in the value of exercise, and would
participate in order to achieve improved physical and social outcomes, but they have little knowledge of
the mental health benefits of exercise.
• Participation is dependent on the familial, social and environmental influences that shape these women’s
lives.
• Women do not share the same opportunities to engage in exercise.
• Forms and formats of exercise that are acceptable, relevant and deemed enjoyable have the potential to
encourage participation, particularly if they combine ‘worthy’ and ‘fun’ outcomes.
Key words
Keywords: exercise, health inequalities, mental
health, postpartum, priority groups, social influence
Introduction
The National Institute for Health and Clinical Excellence
(NICE) has recommended exercise as a nonpharmacological
strategy to promote postpartum
mental health, thus recognising its effectiveness while
responding to concerns that women are being failed
at a time of great vulnerability to illness (National
Institute for Health and Clinical Excellence, 2007).
According to the National Perinatal Mental Health
Project (Edge, 2011), women who are from disadvantaged
communities and/or who are members of minority
ethnic and ethnically diverse groups are particularly
at risk (see Box 1). Reports on physical activity for all
adults (Hillsdon et al, 2004) and physical activity and
mental health interventions (Whitelaw et al, 2008)
reveal a paucity of evidence on their effectiveness with
ethnically diverse populations. Whitelaw et al (2008,
p. 61) conclude that ‘equality strands of ethnicity and
race ... and religion, were almost completely absent ...
given that barriers to physical activity can be particularly
prominent and significant to these groups.’
Recent guidance from the Department of Health,
Physical Activity, Health Improvement and Protection
(2011) recommends a multi-agency, multi-level approach to involving members of ethnically diverse
groups in physical exercise. This guidance is particularly
relevant to women from deprived backgrounds.
There has been little attempt to understand the experience
of these women with regard to participation in
exercise and its benefits at the postpartum stage. This
paper presents findings from phase 1 of a larger study.
The aim of this part of the study was to explore factors
that should be considered when designing and delivering
exercise interventions to promote the mental health
of postpartum women in deprived, ethnically diverse
communities.
Ethnically diverse women, postpartum
health, mental health and exercise
interventions
There is very little information about the risk and
prevalence rates of different mental health problems
among postpartum women from ethnically diverse
groups, although a figure of 10–15% is generally proposed
as a conservative estimate for postpartum depression
across cultures (Edge, 2011). There appears
to be a general belief that these women face greater
challenges and experience poorer outcomes, particularly
in deprived communities. Postpartum exercise
interventions have rarely included or reported outcomes
for women from ethnically diverse groups (Whitelaw
et al, 2008; Biddle et al, 2000). Their requirements,
preferences, cultural obligations and social influences
have never been systematically determined. Previous
research in the USA with ethnically diverse women’s
groups and postpartum groups identified a complex
set of barriers and enablers. Family priorities, lack of
time, lack of previous experience of exercise and financial
considerations emerged as important across cultural
groups. Cultural barriers, which were nuanced and multi-layered, varied between groups, but included
acculturation issues, social influence and lack of family
and community support. Some studies recognised the
importance of safety and settings for participation
(Evenson et al, 2009; Eyler et al, 2002). Lack of understanding
about mental health (Edge, 2011; Greene
et al, 2008; Wittowski et al, 2011), fear, stigma, shame,
denial, negative family and community strictures, and
a paucity of culturally relevant, cross-cultural assessment
tools can make it difficult to access and deliver
support (Edge, 2011; Templeton et al, 2003; Zubaran
et al, 2010).
Guidance on exercise for postpartum health is
sparse and non-specific (Royal College of Obstetricians
and Gynaecologists, 2006). There is little clarity on
appropriate and effective postpartum exercise, irrespective
of ethnicity. Published studies report various
forms of exercise and formats of services, but with
little clarity about their relative merits (Davis and
Dimidjian, 2012). The focus has been on physical
outcomes, such as chronic illness or weight management
(Evenson et al, 2009), or on the management of
postpartum mental illness, particularly postpartum
depression (Daley et al, 2007). There is little guidance
on exercise to promote postpartum mental health,
especially with a promotion and prevention agenda.
Methodology
Ethical review
A favourable ethical opinion was issued by the University
of Wolverhampton School of Health Research
Ethics Sub-Committee and the Staffordshire Research
Ethics Committee. Informed consent was obtained
from all participants, and their rights to withdraw, as
well as their confidentiality and anonymity with regard
to quotations, were upheld. Particular attention
was paid to managing safety in relation to participant
disclosure, as it was anticipated that some women
might express sensitive opinions.
Study design
The study was designed using the principles of
grounded theory because this is particularly appropriate
when little is known about a particular subject
(Glaser and Strauss, 1967). The location was one of 25
priority neighbourhoods, that is, localities that fall
within the worst 5% nationally for multiple deprivation
in England. The population of this part of the
country is very diverse, and it includes both established
and newer communities.
ecruitment and sample
Recruitment was through a combination of convenience
and purposive sampling from local health
centres, children’s centres and community agencies
through leaflets, by word of mouth and by personal
invitation. A total of 25 women from across the
ethnically diverse community agreed to take part in
the study (see Table 1).
Participants who were not health professionals (n =
8) were invited to Focus Group 1. Cre`che and breastfeeding
facilities were offered to everyone in order to
remove barriers to participation.Health andcommunity
professionals were invited to Focus Groups 2 (n = 7)
and 3 (n = 6). Most were parents, but the professional
roles that were represented included midwife, early
years professional, health promotion and family support
worker, community psychiatric nurse, exercise
professional, service provider/group facilitator, health
visitor, link worker and nursery nurse. Interviews were
conducted with four senior decision makers in local
organisations. Many of these women had occupied
between one and four roles during the previous 5 years.
A total of 48 roles, more than the sample size (n = 25),
were recorded (see Table 1).
Data collection and analysis
A flexible topic guide was utilised. The health promotion
model of Dignan and Carr (1991) and the
integrative framework of James and Prilleltensky
(2002) facilitated data organisation and analysis. The
health promotion model ensured systematic discovery
of all aspects of service design and delivery, including
assessment of need, planning, design, implementation
and evaluation. The integrative framework enabled
appreciation of the lived experience of women, recognising
socio-economic and socio-cultural factors and
local context.
The use of a semi-structured schedule, a flexible
topic guide informed by a health promotion model,
may seem at odds with a grounded theory approach.
However, the topics were not unique to this area of
research, but outlined the broad areas of intervention
design in health promotion. The integrative framework
helped to ensure understanding of cultural nuance
and expression. In keeping with grounded theory,
constant comparison helped to identify similarities
and differences. This enabled the discovery of crosscutting
core categories and themes in the context from
which they emerged.
In keeping with grounded theory, four steps were
followed.
1. Data collection and analysis were conducted concurrently.
Analysis of the first transcript (Focus
Group 1) informed subsequent data collection.
Table 1: Participant characteristics of sample (n = 25*)
2. Every segment of data was reviewed and checked
for similarities and differences, and compared with
other segments to clarify and ensure meaning.
3. Nine thematic concepts grounded in the data
emerged after axial coding.
4. After a review of the thematic concepts and continually
checking back to the raw data to preserve
context, four overarching core categories were
identified.
Findings
Four core categories were identified: first, postpartum
exercise, secondly, beliefs and values, thirdly, support
and influence, and fourthly, planning and resources.
Each category is presented below. Where relevant, the
ethnic group and/or role of the participant are included.
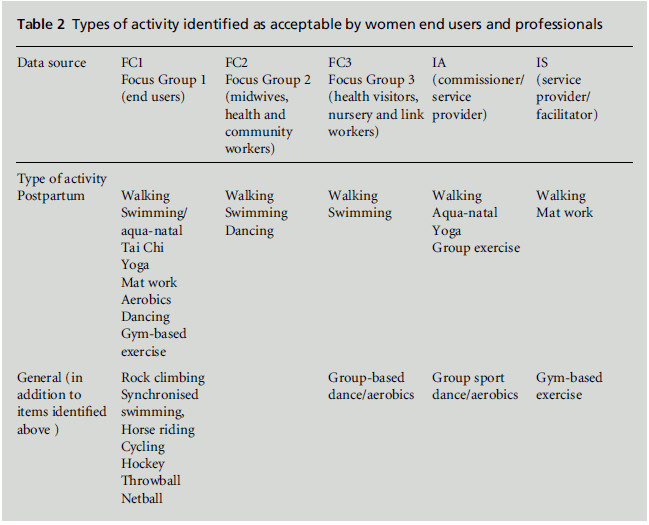
Postpartum exercise
This category highlighted the lack of clarity with
regard to postpartum exercise. It includes data on optimising the core content of exercise services, and
considerations of form, format, intensity, duration
and frequency of exercise for the postpartumstage and
to promote postpartum mental health.
Participants did not know what constituted appropriate
postpartum exercise, and had little personal
experience of it. Professionals were unclear about
what to advise in terms of content, setting and context
for enhanced mental health and well-being. However,
participants could identify what was considered enjoyable
and acceptable with a small baby and within
their family, community groups and neighbourhoods
(see Table 2). Some forms of exercise were deemed to
be ‘fun.’ Dancing was particularly popular, and mentions
of ‘Bollywood dancing’ as exercise (FC2p22) and
‘dance in the aerobics section’ (FC1p8) were enthusiastically
received. Personal goals were important, and
regular group sessions that included social time were
perceived as preferable: ‘allows you to leave all your
household stuff away for one day’ (FC1p16). Sessions
outside the home had the added value of providing
respite from family responsibilities.
Participants weighed up the pros and cons of
different types of exercise as well as permutations of
format, context and setting, that is, individual versus group, indoors versus outdoors, and home-based
exercise versus exercise in a public setting. It was a
deliberation that required a detailed appreciation of
influences, barriers and enablers for women. All of the
focus groups mentioned walking (FC1p4), and over
66% of women had increased their physical activity in
this way, although being outdoors presented challenges
in terms of safety and propriety for some
women. Some forms of exercise were heavily imbued
with religious and cultural connotations and were not
universally acceptable:
Table 2: Types of activity identified as acceptable by women end users and professionals.
Some men, they say that you cannot dance, some men in
Saudi Arabia ... but in Egypt, Yemen, they dance, they do
everything that they want. Nobody says that you cannot
do that, they are still Muslim, you cannot say that they are
not Muslim because they dance.
(FC1p9, Yemeni Arab mother)
Enjoyment appeared to be largely dependent on
personal preference rather than culture. Women felt
able to participate in a diverse range of activities, but
professionals were more conservative in their estimates
of what women liked. The moderating factor
appeared to be what was acceptable to women and the
wider community, particularly in Muslim families,
although it would be inappropriate to generalise. The
data did not support any particular, mandatory restrictions
for any of the ethnically diverse groups
represented; those mentioned may only reflect religious
or cultural traditions adopted within specific
local family or social circles.
Some perceived barriers might be due to lack of
understanding. Women were keen to learn better
exercise skills and indicated that the quality of instruction,
support and encouragement from facilitators
was important. However, they had difficulty with the
advice proffered in exercise classes, for example, to be
‘aware of their own bodies’ and do what ‘feels safe’:
The lady who teach us, she tell us if you get back ache do
not do the exercise. You are not sure, which means, which
back ache. ... Whether you have pressure in your back or
you just a bit tight because you not exercise before.
(FC1p6, Arab mother)
Social and cultural norms were also significant. Arab
and Pakistani participants reported issues with western
dress codes such as wearing trainers. This surprised
Black Caribbean and White participants, who
felt that it might be a ‘culture thing’ (FC1p10) but
seemed keen to understand and find solutions. Participants
indicated that exercise groups have a ‘culture’,
and that negotiating this culture can be tricky.
Some women were less familiar with or did not
understand the norms of participation, while others
found the norms uncomfortable. Women appeared to
find security, at least initially, in a more directive and prescriptive approach to exercise instruction and
delivery.
Beliefs and values
This category reflected how ethnically diverse postpartum
women made decisions about health. They
appeared keen to participate in exercise, and identified
a variety of benefits, including weight loss, appearance,
and management of chronic conditions, for
example, diabetes: ‘to keep my blood sugar stable’
(FC1p2). Over 33% said that they would exercise to
lose weight and improve their body shape because:
When you have a baby, and then you notice you start to put
on weight, your shape changes, you want to look better.
(FC1p2)
Exercise promoted social interaction, particularly
with a group, irrespective of ethnicity or the ethnic
mix of the group:
I was kind of alone ... and then started in a group where
there was other people, it actually got me out of the house
and kept getting me out of the house.
(FC1p17 Black Caribbean, single parent)
To make me feel better about myself. Because if you are
doing something you feel better for it than just sitting
down at home in front of the TV.
(FC1p2)
These findings showed clear awareness of the physical
benefits and social advantages of exercise, including
friendship, shared values, working together and reducing
isolation. However, women did not associate
exercise with mental health or the prevention of
mental illness.
The role and status of the mother emerged as a
significant influence on her power to exercise choice
and to meet family and social responsibilities, obligations
and expectations:
If she is a mum ... living with her in-laws ... they are
concerned about the in-laws, ... you usually find that they
are tired, ... anaemic, ... run down, ... stressed out. ... Some
of them haven’t got time because they’ve got to do their
housework. It’s what they see as important instead of their
own health.
(FC3p5/6, health professional referring to Pakistani
mothers in extended families)
Participants described difficulty in pursuing independent
choices:
They may not like to ask ... like they are asking for
something for themselves ... if they are traditional and
living with their in-laws this may be something that will
stop them from coming.
(FC1p20, Pakistani mother)
Even when the women understood and accepted the
value of exercise, perceptions within the family about
whether participation was appropriate could determine
engagement:
If you have a baby and you are living with your husband’s
family, you are already tired – it’s not healthy to have to
fight, to challenge, because there are other things.
(FC1p11)
These findings showed that personal and family values
underpinned the way in which women exercised
choice. Caring for husbands, children and older relatives
often took precedence over their own health and
needs. Many women, particularly in Asian and Arab
families, chose acceptance of what they perceived was
expected. Avoidance of conflict and expectations of
propriety, dutifulness and virtue as a woman, mother
and daughter-in-law were highly valued and could be
more important than belief in the value of exercise.
Support and influence
This category refers to the influence of peers, family
and professionals with regard to taking part in exercise.
Women responded positively to referrals, advice
and support from peers, family and social circles.
Family members were able to provide encouragement
and practical support, particularly with transport and
childcare. Support from other postpartum women,
including those from other cultural and religious
backgrounds, was also helpful. Professionals outlined
individualised strategies to negotiate family barriers
and promote engagement with health services generally.
They also described the professional conflict that
this sometimes generated for them:
It is very disempowering to accept that the mother may
not be able to make the decision herself because there
would be consequences for her. Her mother-in-law ... her
husband may not like it ...
(FC3p14, Asian mother/health professional)
Some participants perceived a clash between the
approaches of westernised and traditional cultures
(FC3p5). They also felt that some women were ‘passive
to healthcare’ (FC3p12) and lacked motivation.
They expressed impatience with women who picked
and chose what suited them.
Although the dynamic with health professionals
could be difficult, women also reported that health
visitors’ interventions were helpful, and that their
influence was accepted and valued:
I actually saw it as positive when I had to have a
professional in because they were very protective over
me. And they [the family] had visitors waiting downstairs
to see the baby, because it’s all about baby.
(ISp6, Pakistani mother)
She [a young mother] had been in England for 3 years and
she had not left the house alone until the health visitor
went to the house and ... said this child has to come out.
(FC2p19, Pakistani community professional)
Thus the directive and prescriptive aspect of the
professional role could override family restrictions,
to the benefit of the mother.
There was conflict between the competing cultures
of standard health models and traditional beliefs,
which may warrant closer examination. Professionals
demonstrated understanding and the ability to manoeuvre
around challenges, but their remarks were
tinged with wariness about the possibility of a backlash.
They seemed to be constrained by their own
frameworks of practice.
Family responsibilities and obligations aside, other
influences could present significant and apparently
idiosyncratic barriers to participation in exercise.
Seemingly absolute restrictions were imposed on some
women, including those who understood the value of
exercise:
They don’t go to swimming because their husbands don’t
let them go to swimming even if it’s ‘women only’, but
maybe the lifeguard is men or the CCTV will see ...
(FC2p20, Arab community professional)
Other examples included restrictions on exercising to
music with a beat, female-only walking groups and the
need to be chaperoned, irrespective of safety or accessibility.
This obviously affected how women were
able to access services:
because in my clinic there are women who come on their
own to see me on the bus, they drive, they walk they come
by themselves but then there are other women who cannot
come because they are not allowed to come out by
themselves, their husband has to bring them . ... And
they are all, Pakistani, Islamic, but all very different.
(FC2p5, White midwife)
These findings point to negative power and control by
husbands and parents-in-law, based on personal interpretations
of what is appropriate. The findings also
suggest a high level of mistrust and fear in relation to
both young women themselves and their safety.
Education and acculturation could help women to
make better use of health services. Professionals described
barriers that stemmed from lack of education
associated with women either coming from ormarrying
into a family that was less educated or acculturated.
Education and the lack of it was reflected in child
rearing, understanding and using health information,
and in challenging or managing cultural issues that
inhibited engagement. Better educated, more acculturated
women displayed a greater ability and willingness
to work with the social norms of the majority
population without appearing to experience conflict.
Knowledge and understanding of mental healthwas
generally poor. Mental health problems were regarded
as taboo (FC3p9), and seeking help could be uncomfortable
and challenging for women.Women could
be ‘overpowered by family members who speak for
them’ (FC3p9). Women themselves might ‘think that
there is something really bad in it ... they will not ask
for help’ (FC2p15). Women with poor health literacy,
little acculturation and limited autonomy were particularly
vulnerable to secretiveness and denial about
mental health problems. Identifying and gaining access
to women who might benefit from a programme
designed to promote positive postpartummental health
may present challenges and require careful management.
Planning and resources
Access, timing, the availability of private spaces that
were not overlooked, and cre`che and breastfeeding
facilities were among the many practical issues that
needed to be addressed when delivering an exercise
programme. Service design and delivery appeared to
be informed by the experience of staff in community
organisations. There did not appear to be any systematic
exploration or documentation of differing needs
and perspectives. Despite the diversity of both the
workforce and the client group, there appeared to be
little institutionally driven learning and reflection on
matters linked to ethnicity and culture. Professionals
and health and community organisations seemed to
lack confidence in the resources available for identifying
women at risk of developing postpartummental
health problems. Instead they relied heavily on
their own strategies, which, although creative, did not
appear to be well documented or validated.
Although language skills were generally considered
useful, there were differences in how and when
language mattered. There was little consensus on the
usefulness of translation and interpretation services.
Women appeared to be less concerned about their
own or professionals’ language skills than about the
process of information provision, which they found
patchy, inconsistent and culturally disconnected. There
were specific issues relating to mental health, and
professionals described having to choose words carefully
in Arabic, Urdu, Mirpuri and Punjabi when
describing mental health concepts.
Professionals frequently mentioned resource allocation
and funding. This raised issues of fairness and
equity. The ever-changing nature of resource allocation
made it difficult to use learning from previous
experience to create, develop and sustain services. This
was attributed to funding and the way that it was used.
Professionals and local organisations appeared to see themselves as passive recipients of others’ decisions
about resources.
Discussion
The findings of this study show that factors involved in
the design and delivery of successful exercise interventions
to promote positive mental health among
postpartum women in deprived, ethnically diverse
groups are complex, intertwined and multi-layered.
Developing a programme of exercise may require a
pluralistic approach, as suggested in Tackling Health
Inequalities (Department of Health, 2003) and Start
Active, Stay Active (Department of Health, Physical
Activity, Health Improvement and Protection, 2011).
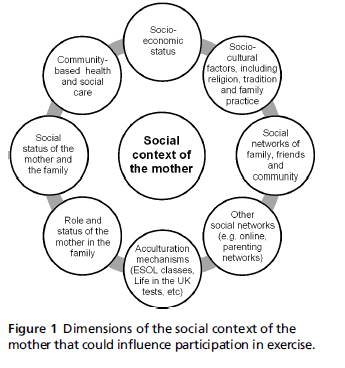
Figure 1 shows the dimensions of the social context of
the mother that could influence participation in
exercise.
Participants, irrespective of culture, believed that
exercise was beneficial, but their exercise behaviour
was influenced by the women’s personal priorities and
the context of their lives. This finding resonates with
those of previous studies. For example, Evenson et al
(2009) examined the beliefs of 667 ethnically diverse
women in the USA. They described similar enablers
and barriers, albeit with some variation between
groups. There was also a suggestion that the experience
of women in the White group was more positive,
as they were more accustomed to exercise and its
norms, had greater knowledge and previous experience
of exercise, more financial power and a higher
level of education. In our study, the White and Black
African/Caribbean women appeared to be more able to engage with health services. They were not necessarily
better educated, but were English speaking and
acculturated. In contrast, the Asian and Arab women
did not always have sufficient personal or financial
autonomy to engage in the same way.
Figure 1 :Dimensions of the social context of the
mother that could influence participation in exercise.
Several studies have recognised the importance of
support, both practical support to enable women to
engage with services, and social support which could
promote participation and adherence (Biddle and
Mutrie, 2007, pp. 145–6, 152). Our participants
responded positively to the role of an exercise group
in reducing isolation, which is a particular problem for
immigrant mothers (Edge, 2011). The ethnicity of
other postpartum women was not a problem, and is
unlikely to inhibit participation, which bodes well for
services in an ethnically diverse community. In fact,
the women accepted other postpartum women as part
of their network, placing importance on shared values
alongside personal outcomes.
The lack of clarity about postpartum exercise and
the absence of well-researched guidance may contribute
to inequality irrespective of ethnicity and cultural
diversity (Royal College of Obstetricians and Gynaecologists,
2006). Research is needed to determine the
best types of exercise, and also those types of exercise
that women should avoid during the postpartum
period. The needs and preferences of ethnically diverse
women also require attention (Davis and Dimidjian,
2012). Although pram pushing may provide useful
postpartum exercise, walking outdoors was not an
option for some of our participants (Daley et al, 2007).
Lack of knowledge about mental health problems is
a significant issue in all ethnic groups. The women
were more aware of the physical and social benefits
associated with exercise than of the contribution that
it might make to their mental health. Public health
information strategies should include the link between
exercise and improvements in mental health. This
might also help to reduce stigma, fear and shame.
Our study highlights two other issues relating to
mental health, namely the lack of culturally sensitive
assessment and the need for means of educating
people about mental health in languages other than
English. Needs assessment, delivery and evaluation do
not appear to be explicit, systematic and consistent.
Tools do not appear to be culturally applicable. They
were deemed to lack resonance with professional and
client experiences at ground level. This could indicate
problems with the design of the tools (Zubaran et al,
2010), a need for training, or the sidelining of research
and theory in service design. Successful service development
should harness users’ and professionals’ experience
with theory (Farris et al, 2004). This might
help to offset the suggestions from earlier studies of
ethnically diverse postpartumwomen that health professionals
do not understand them (Wittowski et al,
2011). Our study suggests that professionals and organisations appear to be genuinely concerned about
health outcomes for mothers, but feel disempowered
in the face of family, social and cultural considerations
and the restrictiveness of their own practice models.
This led to frustration, impatience and ethical conflict
among professionals, and wariness, resentment and
perceived discrimination among the women. More
work in this area is required, particularly with regard
to individual and mutual values and the underlying
priorities and values that shape practice frameworks.
Culture, tradition, ethnicity and religion, which
often attract a disproportionate amount of focus and
misconception, did colour what women individually
found acceptable. However, they did not appear to
adversely affect the personal motivation of women
who were able to participate in exercise. Acculturation
was less about westernisation or relinquishing traditions
or beliefs, and more about accommodating,
understanding and absorbing other frames of reference,
without discomfort or when they had contextual
value. These findings support those of earlier studies
(Whitelaw et al, 2008; Davis and Dimidjian, 2012).
However, a complex set of less tangible cultural barriers
could influence participation. Family, community and
religion could provide practical, emotional, philosophical
and moral support, but they could also take
precedence over a mother’s own health. Negative
familial and social influences and lack of clarity about
religion may need to be addressed in forums away
from direct health promotion initiatives because, in
some instances, the pressure to behave in particular
ways is associatedwith religion, or is perceived as such,
and is complicated by considerations such as role,
status and propriety within the social group.
At a policy level, the UK mental health strategy for
the general population places emphasis on diagnosable
conditions such as depression. However, pertinent
to the postpartum stage (Edge, 2011) are widespread,
undiagnosed mental health problems such as anxiety,
stress, low self-esteem, and impaired ability to cope
with everyday life (Biddle et al, 2000). In Biddle et al
(2000), Mutrie’s suggestion that all exercise interventions
should evaluate a wider range of outcomes,
including mental health outcomes, could have particular
resonance for ethnically diverse postpartum
women in priority groups. Exercise interventions should
target a range of mental health problems and focus on
prevention and promotion for a wider pool ofwomen,
particularly in deprived communities with reportedly
higher levels of poor mental health and greater risk
factors.
Conclusion
The lack of clarity about suitable exercise for postpartum
women is an important issue. Forms of
exercise that are known to have specific movements
for the postpartum stage, and which many women enjoy, such as yoga and pilates, require further investigation.
Facilitator training should include developing
cultural competence to equip professionals to work
with ethnically diverse women. The incorporation of
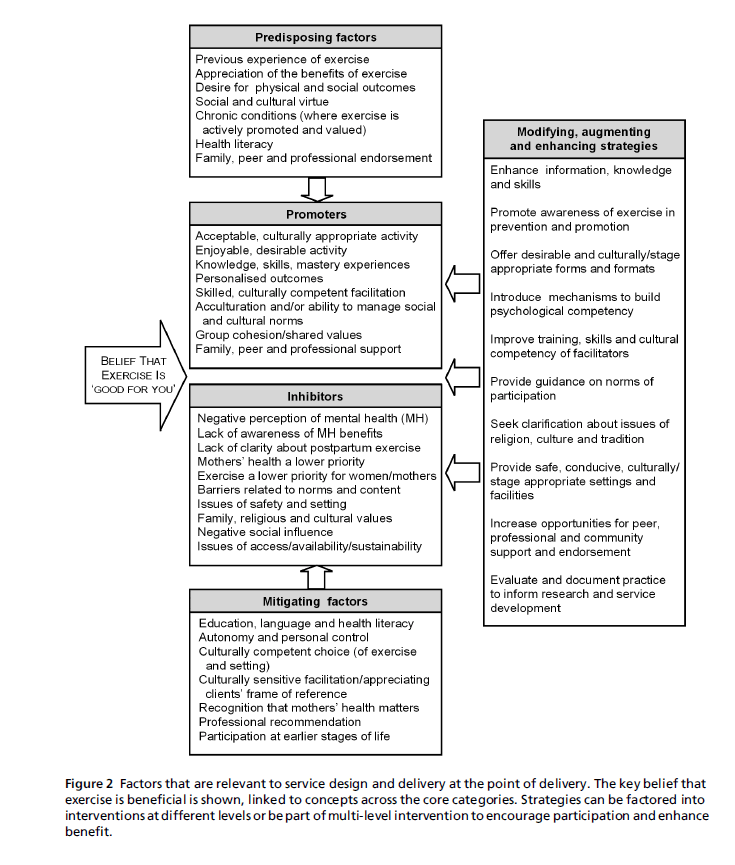
behaviour change models and health promotion frameworks
could help to optimise success (see Figure 2).
Figure 2:Factors that are relevant to service design and delivery at the point of delivery. The key belief that
exercise is beneficial is shown, linked to concepts across the core categories. Strategies can be factored into
interventions at different levels or be part of multi-level intervention to encourage participation and enhance
benefit.
The findings of this qualitative study are encouraging,
and indicate that it is reasonable to view exercise
as a suitable non-pharmacological intervention, as
suggested by NICE. A wide range of factors influence
exercise for postpartum women in ethnically diverse
priority groups, and these would need to be factored
into the design of future interventions. The findings
show a combination of practical considerations alongside
social–cognitive factors, mediated by sociocultural
influences relevant to exercise, mental health,
the postpartumstage (Evenson et al, 2009) and health
promotion in general (Farris et al, 2004). Influential
factors range from internal personal factors to external
factors associated with the context of postpartum
women’s lives (see Figure 1).We conclude that it appears
to be possible to design and deliver exercise interventions
that are relevant and effective, and offer a framework
of mechanisms that can potentially influence
successful design.
References
- Biddle SJ and Mutrie N (2007) Psychology of Physical Activity: determinants, well-being and interventions, 2nd edn. Oxford:
- Routledge. Biddle SJ, Fox KR and Boutcher SH (2000) Physical Activity and Psychological Well-Being. London:
- Routledge. Daley A, MacArthur C and Winter HR (2007) The role of exercise in treating postpartum depression: a review of the literature. Journal of Midwifery and WomenÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s Health 52:56ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â62.
- Davis K and Dimidjian S (2012) The relationship between physical activity and mood across the perinatal period: a review of naturalistic and clinical research to guide future investigation of physical activity-based interventions for perinatal depression. Clinical Psychology: Science and Practice 19:27ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â48.
- Department of Health (2003) Tackling Health Inequalities: a programme for action. London:
- Department of Health. Department of Health, Physical Activity, Health Improvement and Protection (2011) Start Active, Stay Active. A report on physical activity for health from the four home countriesÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ Chief Medical Officers. www.gov.uk/ government/uploads/system/uploads/attachment_data/ file/152108/dh_128210.pdf.pdf (accessed 19 June 2013).
- Dignan MB and Carr PA.(1991) Program Planning for Health Education and Health Promotion, 2nd edn. Philadelphia, PA:
- Lea and Febiger. EdgeD(2011) Perinatal Mental Health of Black and Minority Ethnic Women: a review of current service provision in England, Scotland and Wales. London:
- National Mental Health Development Unit. Evenson KR, Aytur SA and Borodulin K (2009) Physical activity beliefs, barriers, and enablers among postpartum women. Journal of WomenÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s Health 18:1925ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â34.
- Eyler AM, Matson-Koffman D, Vest JR et al (2002) Environmental, policy, and cultural factors related to physical activity in a diverse sample of women: the WomenÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s Cardiovascular Health Network Project ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â summary and discussion. Women and Health 36:123ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â34.
- Farris RP, Haney DM and Dunet DO (2004) Expanding the evidence for health promotion: developing best practices for WISEWOMAN. Journal of WomenÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s Health 13:634ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 43.
- Glaser B and Strauss A (1967) The Discovery of Grounded Theory: strategies for qualitative research. Chicago: Aldine Publishing Company.
- Greene R, Pugh R and Roberts D (2008) Black and Minority Ethnic Parents with Mental Health Problems and Their Children. London: Social Care Institute for Excellence. www.scie.org.uk/publications/briefings/files/briefing29. pdf (accessed 19 June 2013).
- Hillsdon M, Foster C, Naidoo B et al (2004) The Effectiveness of Public Health Interventions for Increasing Physical Activity Among Adults: a review of reviews. London: Health Development Agency.
- James S and Prilleltensky I (2002) Cultural diversity and mental health: towards integrative practice. Clinical Psychology Review 22:1133ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â54.
- National Institute for Health and Clinical Excellence (2007) Antenatal and Postnatal Mental Health: clinical management and service guidance. London:
- National Institute for Health and Clinical Excellence. Royal College of Obstetricians and Gynaecologists (2006) Exercise in Pregnancy (RCOGStatement 4). www.rcog.org. uk/womens-health/clinical-guidance/exercise-pregnancy (accessed 19 June 2013).
- Templeton LV, Velleman R, Persaud A et al (2003) The experiences of postnatal depression in women from black and minority ethnic communities in Wiltshire. Ethnicity and Health 8:207ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â21.
- Whitelaw S, Swift J, Goodwin A et al (2008) Physical Activity and Mental Health: the role of physical activity in promoting mental wellbeing and preventing mental health problems. An Evidence Briefing. Edinburgh: NHS Health Scotland.
- Wittowski A, Zumla A, Glendenning S et al (2011) The experience of postnatal depression in South Asian mothers living in Great Britain: a qualitative study. Journal of Reproductive and Infant Psychology 29:480ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â92.
- Zubaran C, Schumacher M, RoxoMRet al (2010) Screening tools for postpartum depression: validity and cultural dimensions. African Journal of Psychiatry 13:357ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â65.