Original Article - (2017) Volume 18, Issue 6
Department of Surgery and Oncology, Graduate School of Medical Sciences, Kyushu University, 3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan
Received Date: October 20th, 2017; Accepted Date: November 27th, 2017
Objective Pancreatic head cancer is frequently associated with biliary obstruction and gastric outlet obstruction. We have performed biliary and gastrointestinal bypass, even for patients with unresectable pancreatic head cancer without either biliary obstruction or gastric outlet obstruction, to prevent biliary obstruction and gastric outlet obstruction and thus ensure planned chemotherapy as well as to maintain the patients’ quality of life. We therefore evaluated the safety and preventive effect of prophylactic biliary and gastrointestinal bypass. Methods We retrospectively reviewed the data of patients with unresectable pancreatic head cancer from 2001 to 2013. We then selected the patients without either biliary obstruction or gastric outlet obstruction and divided them into a prophylactic biliary and gastrointestinal bypass group and a control group. The perioperative outcomes of prophylactic biliary and gastrointestinal bypass were analyzed, and long-term outcomes including the incidence of biliary obstruction and gastric outlet obstruction were compared between the prophylactic biliary and gastrointestinal bypass group and the control group. Results Of 151 patients with unresectable pancreatic head cancer, 58 had neither biliary obstruction nor gastric outlet obstruction. Of these 58 patients, 32 underwent prophylactic biliary and gastrointestinal bypass. The median operation time, blood loss, and postoperative hospital stay were 272 minutes, 173 ml, and 18 days. Only one patient had postoperative morbidity after prophylactic biliary and gastrointestinal bypass. No patients in the prophylactic biliary and gastrointestinal bypass group developed either biliary obstruction or gastric outlet obstruction, while 81% developed biliary obstruction and 42% developed gastric outlet obstruction in the control group. Overall survival was comparable between the two groups. Conclusion Prophylactic biliary and gastrointestinal bypass showed excellent preventive effects on biliary obstruction and gastric outlet obstruction with low morbidity. Although nonsurgical palliative procedures are preferred for the treatment of biliary obstruction and gastric outlet obstruction, it is time to reappraise prophylactic surgical procedures for unresectable pancreatic head cancer.
Pancreatic Neoplasms; Prophylactic Surgical Procedures
BO biliary obstruction; GOO gastric outlet obstruction; PBGB prophylactic biliary and gastrointestinal bypass; PHC pancreatic head cancer, QOL quality of life
Pancreatic cancer is the most aggressive malignancy of the abdominal organs, and approximately 80% of pancreatic cancers are found in unresectable state [1]. The pancreas head is the most common site at which pancreatic cancer develops [2]. Pancreatic head cancer (PHC) is often associated with biliary obstruction (BO), which causes jaundice, liver dysfunction, and cholangitis, and gastric outlet obstruction (GOO), which develops in a relatively later period and leads to anorexia and vomiting. These complications deteriorate the quality of life (QOL) of patients with PHC. Although the best way to prevent or palliate BO and GOO is curative resection, most patients with PHC do not benefit from resection. The National Comprehensive Cancer Network guidelines propose endoscopic biliary stenting, percutaneous biliary drainage with subsequent internalization, and open biliary bypass to palliate BO and gastrojejunostomy, enteral stenting, and percutaneous endoscopic gastrostomy to palliate GOO in patients with unresectable PHC [3].
However, some patients with unresectable PHC have no symptoms of BO or GOO at the time of diagnosis. These patients are usually treated by chemotherapy without palliation. However, most patients are expected to develop BO or GOO as the lesions progress. These complications often interrupt continuation of chemotherapy. Cholangitis due to BO can be life-threatening, especially when patients have leukocytopenia secondary to chemotherapy. Therefore, it is reasonable to prevent the development of BO prior to chemotherapy. In addition, the usefulness of prophylactic gastrointestinal bypass for unresectable periampullary cancer has been shown in randomized controlled trials [4, 5].
We have performed biliary and gastrointestinal bypass in unresectable PHC patients without either BO or GOO who were fit for surgery and provided informed consent to prevent the development of BO and GOO and thus ensure planned chemotherapy as well as maintain the patients’ QOL. The purpose of this study was to evaluate the safety and preventive effect of prophylactic biliary and gastrointestinal bypass (PBGB) for patients without either BO or GOO. For this purpose, we analyzed perioperative outcomes of PBGB and compared long-term outcomes including the incidence of BO and GOO between patients with and without PBGB.
Study Population
This study was approved by the Ethics Committee of Kyushu University and conducted according to the Helsinki Declaration. We retrospectively reviewed the medical records of patients who had PHC that was considered unresectable owing to locally advanced or metastatic disease and who were treated at the Department of Surgery and Oncology, Kyushu University Hospital between January 2001 and December 2013. Patients without either BO or GOO at the time of their first visit were selected for the study. They were divided into a PBGB group and a control group according to whether they underwent PBGB. The perioperative outcomes of PBGB were analyzed. If patients had undergone palliative treatment for BO or GOO, the outcomes were also reviewed. The patients’ clinical backgrounds and long-term outcomes, including the incidence of BO and GOO and the survival rate, were compared between the two groups. Survival time was defined as the period between the first visit to our institute and death. For patients diagnosed with unresectable PHC by imaging findings, the treatment was selected at the discretion of the attending surgeons or physicians and the patients’ intentions. We generally recommended PBGB if patients were fit for surgery. However, chemotherapy or chemoradiotherapy was selected for patients who were considered to need early administration of chemotherapy, such as those with multiple liver metastases; patients with locally advanced disease who had possibility of conversion to resection; and patients whose life expectancy was considered short. If the PHC in patients who were planned to undergo curative resection was found to be unresectable at laparotomy, biliary and gastrointestinal bypasses were performed.
Biliary and Gastrointestinal Bypass
We mainly performed hepaticocholecystojejunostomy for biliary bypass and gastrojejunostomy for gastrointestinal bypass. These procedures have been previously described [6]. Briefly, approximately 1-cm incisions were created at the common hepatic duct and neck of the gallbladder, and a single-layer side-to-side anastomosis of the common bile duct and gallbladder was performed with an interrupted or running suture. Side-to-side cholecystojejunostomy and side-to-side gastrojejunostomy were carried out in a Rouxen- Y fashion. Side-to-side jejunojejunostomy between the afferent and efferent loops was then performed (Braun anastomosis). Both stapling devices and hand suturing were used for these anastomoses.
Statistical Analysis
Continuous variables were compared by Student’s t-test or the Mann–Whitney U-test. Categorical variables were compared by the chi-square test or Fischer’s exact test. The Kaplan–Meier method was used to estimate survival, and the log-rank test was used for comparison. A two-sided p value of <0.05 was considered statistically significant. All statistical analyses were performed using JMP software (version 9.0.2; SAS Institute, Cary, NC, USA).
In total, 151 patients with unresectable PHC were treated in our institution between January 2001 and December 2013. The reasons for unresectability were locally advanced disease in 77 patients (51%), metastatic disease in 33 (22%), and both locally advanced and metastatic disease in 41 (27%). The associations of BO or GOO with the patients’ palliative treatments are shown in Figure 1.
Ninety-three patients had either BO or GOO, and 60 of them initially underwent biliary and gastrointestinal bypass. Although 33 of the 93 patients were initially treated by biliary stenting, six of them required biliary and gastrointestinal bypass later.
Fifty-eight patients had neither BO nor GOO at the time of diagnosis. Thirty-two of these 58 patients underwent PBGB (PBGB group). The PHC of three patients in the PBGB group was found to be unresectable at laparotomy, and the PHC of the remaining patients was considered unresectable based on imaging findings. Hepaticocholecystojejunostomy, hepaticojejunostomy, and cholecystojejunostomy were performed for biliary bypass in 29, 2, and 1 patient, respectively. All patients underwent gastrojejunostomy. The median operation time, median blood loss, and median postoperative hospital stay were 272 minutes (range, 129–495 min), 173 ml (range, 30–610 ml), and 18 days (range, 4–59 days), respectively. Only one patient (3%) had postoperative morbidity (bile leakage); no perioperative mortality occurred. The patient with bile leakage was treated conservatively. During the postoperative follow-up, neither BO nor GOO was recognized in the PBGB group.
The remaining 26 patients were designated as the control group. All patients in the control group developed BO or GOO and required intervention during the follow-up: 14 patients were treated by endoscopic biliary stenting, and the other 12 underwent biliary and gastrointestinal bypass. Among the 12 patients who underwent bypass, 1 developed BO, 5 developed GOO, and 6 developed both BO and GOO before bypass. Of the six patients who developed BO and GOO before bypass, two underwent endoscopic biliary stenting and two underwent percutaneous biliary drainage prior to bypass. In the control group, 81% (21/26) of the patients developed BO and 42% (11/26) developed GOO. The incidences of BO and GOO in the control group were significantly higher than those in the PBGB group (p<0.0001 and p<0.0001, respectively). Two patients (8%) developed morbidities after intervention. One patient developed a liver abscess after stent insertion, and another patient developed a brain infarction after bypass. Twelve of the 14 patients (86%) treated by biliary stenting required stent replacement at a median frequency of 2 (range, 1–10).
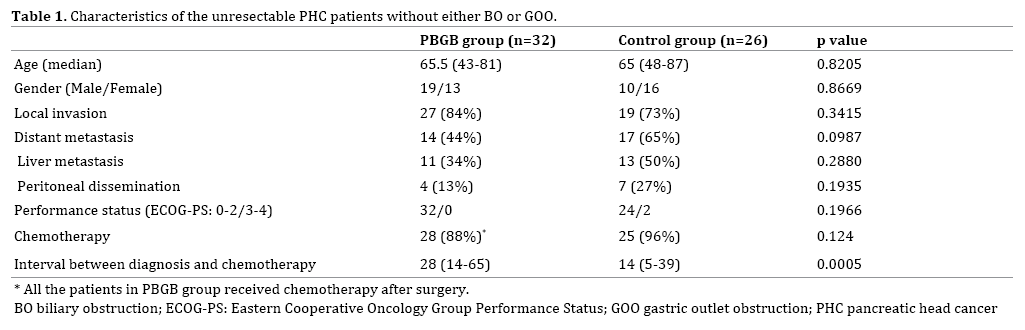
The patients’ characteristics including age, sex, local invasion, distant metastasis (including liver metastasis and peritoneal dissemination), performance status, and introduction of chemotherapy were comparable between the PBGB and control group (Table 1). Although interval between initial diagnosis and first chemotherapy was significantly longer in the PBGB group, the survival time from the patients’ first visit at our institution was comparable between 2 groups (356 days in the PBGB group and 358 days in the control group; p=0.6368) (Figure 2).
In the present study, the following findings were revealed: 1) PBGB effectively prevented development of both BO and GOO in patients with unresectable PHC, while all patients in the control group required subsequent palliative procedure; 2) The postoperative morbidity and perioperative mortality rates associated with PBGB were quite low; and 3) There was no difference in survival between the PBGB and control group.
Several studies, including randomized controlled trials and meta-analyses, reported a lower recurrence rate of BO in patients who underwent surgical biliary bypass than in those who underwent biliary stenting [7, 8, 9, 10, 11, 12, 13]. In our study, none of the patients who underwent PBGB developed BO, while 81% (21/26) of the patients in the control group developed BO. In addition, 86% (12/14) of the patients who were treated by biliary stenting in the control group had recurrence of BO and required stent replacement. Although some authors asserted that the main advantage of biliary stenting is a shorter hospital stay [8, 11], a literature review by Glazer et al. [9] showed that the total hospital stay from the procedure until death was longer in patients with biliary stenting than in patients with bypass because of repeated hospitalization for stent replacement. Most of the biliary stents used for the patients in this study were plastic stents because of the policy of our institute. The patency period of a plastic stent is shorter than that of a metal stent. A review by Moss et al. [10] showed that the median patency of a metal stent ranged from 108 to 273 days while that of a plastic stent ranged from 54 to 165 days. However, this result suggests that even metal stents require replacement if they are used for patients whose life expectancy is nearly 1 year, as in our series.
Two randomized controlled trials showed that prophylactic gastrojejunostomy significantly reduced the incidence of GOO in patients who were found to have unresectable cancer after laparotomy [4, 5]. In the trial in Netherland, 44% (12/29) of the patients with biliary bypass alone developed GOO, while only 6% (2/36) of the patients with biliary and gastrointestinal bypass did [5]. In a study performed at Johns Hopkins [4], 19% (8/43) of the patients with biliary bypass alone developed GOO, although surgeons had judged that they were not at a significant risk for duodenal obstruction at the time of surgery. In the latter study, none of the patients with biliary and gastrointestinal bypass developed GOO. In both trials, additional gastrointestinal bypass did not increase morbidity or mortality.
In previous studies, the morbidity and mortality rates associated with palliative biliary and gastrointestinal bypass reportedly ranged from 17% to 50% and from 0% to 5.9%, respectively [4, 5, 14, 15, 16, 17]. Compared with these results, the postoperative outcomes of our study (morbidity: 3%, mortality: 0%) were quite favorable. One possible reason for the low incidence of postoperative morbidity and mortality was that patients in the PBGB group did not have BO and GOO at the time of the operation. Singh et al. [18] reported that preoperative biliary stenting significantly increased morbidity and mortality after surgical bypass. Räty et al. [19] described that gastric emptying problems owing to GOO were a risk factor of postoperative morbidity after hepaticojejunostomy and gastrojejunostomy. Patients with GOO often have concurrent nutritional disorders. Malnutrition increases postoperative morbidity and mortality [20]. Additionally, PBGB can avoid the emergency setting. Bartlett et al. [15] showed that an emergent operation is a significant risk factor for postoperative morbidity and mortality.
Our results did not show a significant difference in the prognosis between the PBGB and the control groups. Suspension of chemotherapy due to BO or GOO in the control group might have few effects on survival in our series. Recently, combinations of chemotherapy regimens, such as FOLFIRINOX or nab-paclitaxel plus gemcitabine, have been shown to prolong survival of patients with pancreatic cancer metastasis [21, 22]. No patient in our study received these regimens because they were authorized in Japan quite recently (FOLFIRINOX, December 2013; nabpaclitaxel plus gemcitabine, December 2014). These new regimens are more frequently associated with neutropenia than the conventional regimen [21, 22]. Development or recurrence of BO might have resulted in severe cholangitis and prolonged suspension of chemotherapy in the control group if patients had been treated by new regimens. In addition, Conroy et al. [21] called for attention to BO in FOLFIRINOX because high bilirubin levels increase the risk of irinotecan-induced toxicity. Our results showed that PBGB had a reliable and preventive effect on BO. The PBGB group might have shown more favorable prognostic outcomes than the control group if they had been treated by these new regimens.
Recently laparoscopic approaches have been applied to BO and GOO [23, 24, 25]. They might reduce postoperative pain, enhance recovery of the patients and be options of palliative treatment for unresectable pancreatic cancer patients.
A limitation of our study was the retrospective, nonrandomized design; thus, there might be selection bias between the PBGB and the control group. The treatments that patients received were diverse because our policy for treating unresectable pancreatic cancer changed during the study period. To establish solid evidence of PBGB, prospective randomized control trials are needed.
PBGB showed excellent preventive effects on BO and GOO with low morbidity. At the present time, nonsurgical, palliative procedures are preferred for the treatment of BO and GOO associated with unresectable PHC rather than surgical prophylactic procedures. PBGB may have the potential to improve the QOL and prognosis of patients with unresectable PHC in the progress of chemotherapy. It is time to reappraise prophylactic surgical procedures for unresectable pancreatic cancer.
The protocol of this research has been approved by a suitably constituted Ethics Committee of the institution and it conforms to the provisions of the Helsinki Declaration. Ethics Committee of Kyushu University, Approved No. 28-112.
This study was supported by Grants-in-Aid for Scientific Research (KAKENHI; #16K10601).
Authors declare no conflict of interests for this article.